Cancer Res Treat.
2023 Apr;55(2):618-625. 10.4143/crt.2022.852.
Colonoscopic Screening and Risk of All-Cause and Colorectal Cancer Mortality in Young and Older Individuals
- Affiliations
-
- 1Work Health Institute, Total Health Care Center, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea
- 2Center for Cohort Studies, Total Healthcare Center, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea
- 3Department of Occupational and Environmental Medicine, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea
- 4Department of Clinical Research Design & Evaluation, Samsung Advanced Institute for Health Sciences & Technology, Sungkyunkwan University, Seoul, Korea
- 5Division of Gastroenterology, Department of Medicine, School of Medicine, Kangbuk Samsung Hospital, Sungkyunkwan University, Seoul, Korea
- 6Samsung Health Research Institute, Samsung Electronics Co. Ltd., Hwaseong, Korea
- 7Institute of Environmental Medicine, Seoul National University Medical Research Center, Seoul, Korea
- 8Department of Occupational and Environmental Medicine, Hanyang University College of Medicine, Seoul, Korea
- KMID: 2541248
- DOI: http://doi.org/10.4143/crt.2022.852
Abstract
- Purpose
The incidence of early-onset colorectal cancer (CRC) and associated mortality have been increasing. However, the potential benefits of CRC screening are largely unknown in young individuals. We aimed to evaluate the effect of CRC screening with colonoscopy on all-cause and CRC mortality among young (aged < 45 years) and older (aged ≥ 45 years) individuals.
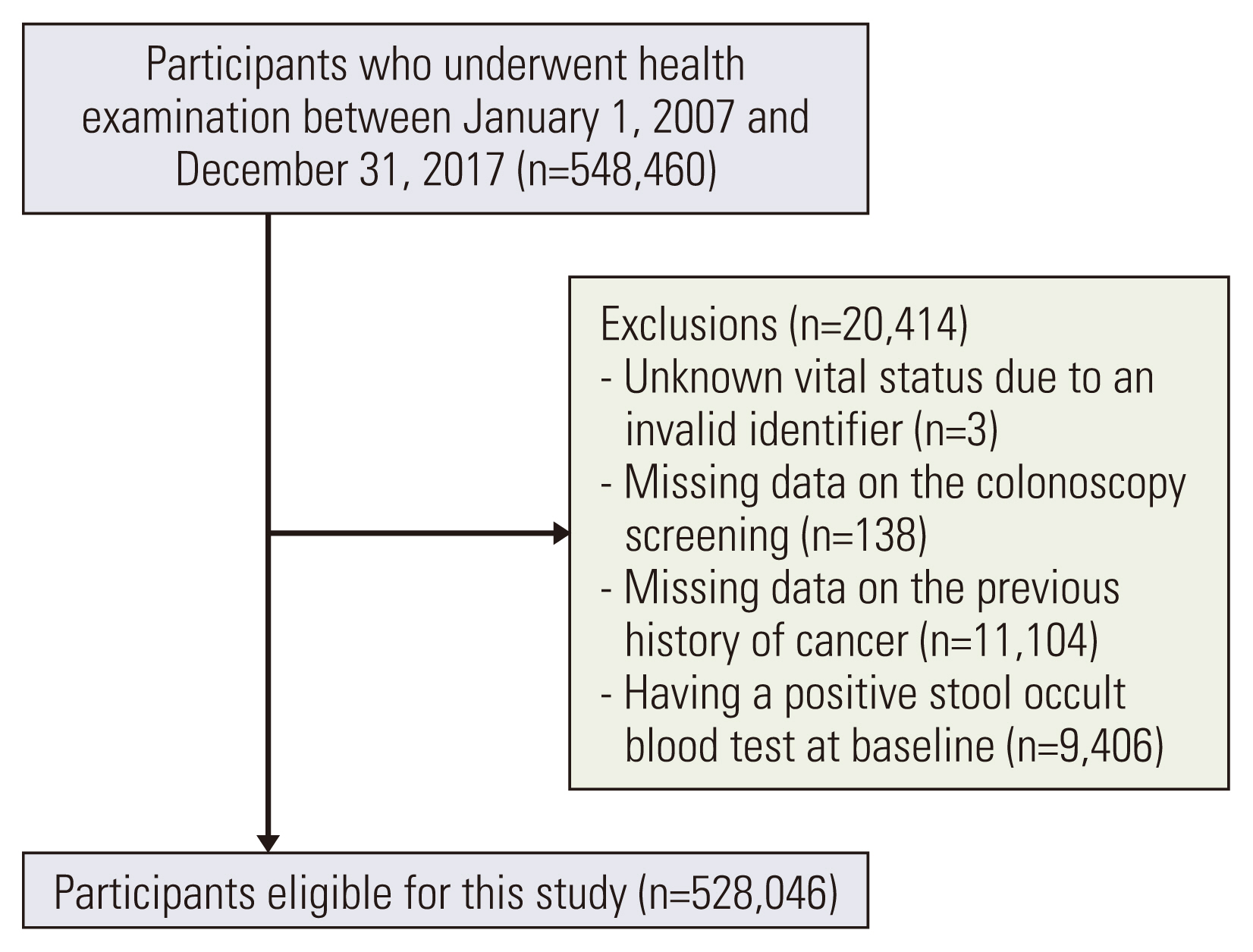
Materials and Methods
This cohort study included 528,046 Korean adults free of cancer at baseline who underwent a comprehensive health examination. The colonoscopic screening group was defined as those who reported undergoing colonoscopy for CRC screening. Mortality follow-up until December 31, 2019 was ascertained based on nationwide death certificate data from the Korea National Statistical Office.
Results
Colonoscopic screening was associated with a lower risk of all-cause mortality in both young and older individuals. Multivariable-adjusted time-dependent hazard ratios (95% confidence intervals) for all-cause mortality comparing ever- to never-screening were 0.86 (0.75-0.99) for young individuals and 0.71 (0.65-0.78) for older individuals. Colonoscopic screenings were also associated with a reduced risk of CRC mortality without significant interaction by age, although this association was significant only among participants aged ≥ 45 years, with corresponding time-dependent hazard ratios of 0.47 (0.15-1.44) for young individuals and 0.52 (0.31-0.87) for those aged ≥ 45 years.
Conclusion
Colonoscopic CRC screening decreased all-cause mortality among both young and older individuals, while significantly decreased CRC mortality was observed only in those aged ≥ 45 years. Screening initiation at an earlier age warrants more rigorous confirmatory studies.
Figure
Reference
-
References
1. Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015; 65:87–108.
Article2. National Cancer Information Center. National cancer statistics [Internet]. Goyang: National Cancer Information Center;[cited 2021 Feb 9]. Available from: https://www.cancer.go.kr/lay1/S1T639C640/contents.do .3. Siegel RL, Torre LA, Soerjomataram I, Hayes RB, Bray F, Weber TK, et al. Global patterns and trends in colorectal cancer incidence in young adults. Gut. 2019; 68:2179–85.
Article4. Sung JJY, Chiu HM, Jung KW, Jun JK, Sekiguchi M, Matsuda T, et al. Increasing trend in young-onset colorectal cancer in Asia: more cancers in men and more rectal cancers. Am J Gastroenterol. 2019; 114:322–9.
Article5. Akimoto N, Ugai T, Zhong R, Hamada T, Fujiyoshi K, Giannakis M, et al. Rising incidence of early-onset colorectal cancer: a call to action. Nat Rev Clin Oncol. 2021; 18:230–43.
Article6. Loberg M, Kalager M, Holme O, Hoff G, Adami HO, Bretthauer M. Long-term colorectal-cancer mortality after adenoma removal. N Engl J Med. 2014; 371:799–807.
Article7. Atkin WS, Edwards R, Kralj-Hans I, Wooldrage K, Hart AR, Northover JM, et al. Once-only flexible sigmoidoscopy screening in prevention of colorectal cancer: a multicentre randomised controlled trial. Lancet. 2010; 375:1624–33.
Article8. Zorzi M, Fedeli U, Schievano E, Bovo E, Guzzinati S, Baracco S, et al. Impact on colorectal cancer mortality of screening programmes based on the faecal immunochemical test. Gut. 2015; 64:784–90.
Article9. US Preventive Services Task Force, Bibbins-Domingo K, Gro-ssman DC, Curry SJ, Davidson KW, Epling JW Jr, et al. Screening for colorectal cancer: US Preventive Services Task Force recommendation statement. JAMA. 2016; 315:2564–75.10. US Preventive Services Task Force, Davidson KW, Barry MJ, Mangione CM, Cabana M, Caughey AB, et al. Screening for colorectal cancer: US Preventive Services Task Force recommendation Statement. JAMA. 2021; 325:1965–77.11. Ho SB, Zaher S. Inverted yield curve: the alarming rising incidence of CRC in young people. Dig Dis Sci. 2020; 65:1590–2.
Article12. Shaukat A, Mongin SJ, Geisser MS, Lederle FA, Bond JH, Mandel JS, et al. Long-term mortality after screening for colorectal cancer. N Engl J Med. 2013; 369:1106–14.
Article13. Wang K, Ma W, Wu K, Ogino S, Giovannucci EL, Chan AT, et al. Long-term colorectal cancer incidence and mortality after colonoscopy screening according to individuals’ risk profiles. J Natl Cancer Inst. 2021; 113:1177–85.
Article14. Buskermolen M, Cenin DR, Helsingen LM, Guyatt G, Vandvik PO, Haug U, et al. Colorectal cancer screening with faecal immunochemical testing, sigmoidoscopy or colonoscopy: a microsimulation modelling study. BMJ. 2019; 367:l5383.
Article15. Jodal HC, Helsingen LM, Anderson JC, Lytvyn L, Vandvik PO, Emilsson L. Colorectal cancer screening with faecal testing, sigmoidoscopy or colonoscopy: a systematic review and network meta-analysis. BMJ Open. 2019; 9:e032773.
Article16. Mayer D. All-cause mortality in colorectal cancer screening. Clin Colorectal Cancer. 2018; 17:e127.
Article17. Shaukat A, Kaalby L, Baatrup G, Kronborg O, Duval S, Shyne M, et al. Effects of screening compliance on long-term reductions in all-cause and colorectal cancer mortality. Clin Gastroenterol Hepatol. 2021; 19:967–75.
Article18. Moayyedi P, Achkar E. Does fecal occult blood testing really reduce mortality? A reanalysis of systematic review data. Am J Gastroenterol. 2006; 101:380–4.
Article19. Chang Y, Jung HS, Cho J, Zhang Y, Yun KE, Lazo M, et al. Metabolically healthy obesity and the development of nonalcoholic fatty liver disease. Am J Gastroenterol. 2016; 111:1133–40.
Article20. Devaux M, Sassi F. Alcohol consumption and harmful drinking: trends and social disparities across OECD countries. Paris: Organisation for Economic Cooperation and Development;2015.21. World Health Organization. The Asia-Pacific perspective: redefining obesity and its treatment. Sydney: Health Communications Australia;2000.22. Won TY, Kang BS, Im TH, Choi HJ. The study of accuracy of death statistics. J Korean Soc Emerg Med. 2007; 18:256–62.23. Song YM, Sung J. Body mass index and mortality: a twelve-year prospective study in Korea. Epidemiology. 2001; 12:173–9.24. Berstad P, Loberg M, Larsen IK, Kalager M, Holme O, Botteri E, et al. Long-term lifestyle changes after colorectal cancer screening: randomised controlled trial. Gut. 2015; 64:1268–76.
Article25. Larsen IK, Grotmol T, Almendingen K, Hoff G. Impact of colorectal cancer screening on future lifestyle choices: a three-year randomized controlled trial. Clin Gastroenterol Hepatol. 2007; 5:477–83.
Article26. Schultz WM, Kelli HM, Lisko JC, Varghese T, Shen J, Sandesara P, et al. Socioeconomic status and cardiovascular outcomes: challenges and interventions. Circulation. 2018; 137:2166–78.27. Cho HJ. Equity in health care: current situation in South Korea. J Korean Med Assoc. 2013; 56:184–94.
Article28. Benazzato L, Zorzi M, Antonelli G, Guzzinati S, Hassan C, Fantin A, et al. Colonoscopy-related adverse events and mortality in an Italian organized colorectal cancer screening program. Endoscopy. 2021; 53:501–8.
Article29. Bielawska B, Day AG, Lieberman DA, Hookey LC. Risk factors for early colonoscopic perforation include non-gastroenterologist endoscopists: a multivariable analysis. Clin Gastroenterol Hepatol. 2014; 12:85–92.
Article30. Kim SY, Kim HS, Park HJ. Adverse events related to colonoscopy: global trends and future challenges. World J Gastroenterol. 2019; 25:190–204.
Article31. Wiegering A, Ackermann S, Riegel J, Dietz UA, Gotze O, Germer CT, et al. Improved survival of patients with colon cancer detected by screening colonoscopy. Int J Colorectal Dis. 2016; 31:1039–45.
Article32. Lau J, Lim TZ, Jianlin Wong G, Tan KK. The health belief model and colorectal cancer screening in the general population: a systematic review. Prev Med Rep. 2020; 20:101223.
Article33. You YN, Lee LD, Deschner BW, Shibata D. Colorectal cancer in the adolescent and young adult population. JCO Oncol Pract. 2020; 16:19–27.
Article34. Wolf AM, Fontham ET, Church TR, Flowers CR, Guerra CE, LaMonte SJ, et al. Colorectal cancer screening for average-risk adults: 2018 guideline update from the American Cancer Society. CA Cancer J Clin. 2018; 68:250–81.
Article35. Rauscher GH, Johnson TP, Cho YI, Walk JA. Accuracy of self-reported cancer-screening histories: a meta-analysis. Cancer Epidemiol Biomarkers Prev. 2008; 17:748–57.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Colon Cancer Screening—Is It Necessary to Start under the Age of 50?
- Strategies for colorectal cancer screening and post-polypectomy surveillance for young adults under age 50
- Screening and surveillance for hereditary colorectal cancer
- Anatomical distribution and detection rate of colorectal neoplasms according to age in the colonoscopic screening of a Korean population
- Comparison of Colonoscopy Surveillance Outcomes Between Young and Older Colorectal Cancer Patients