Ann Surg Treat Res.
2023 Apr;104(4):205-213. 10.4174/astr.2023.104.4.205.
Difference in prognostic impact of lateral pelvic lymph node metastasis between pre- and post-neoadjuvant chemoradiotherapy in rectal cancer patients
- Affiliations
-
- 1Division of Colon and Rectal Surgery, Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2541146
- DOI: http://doi.org/10.4174/astr.2023.104.4.205
Abstract
- Purpose
The prognostic significance and treatment of lateral pelvic lymph node metastasis (mLPLN) in rectal cancer patients receiving neoadjuvant chemoradiotherapy (nCRT) are not well understood. In this study, we evaluated the impact of mLPLN identified in imaging modality on outcomes.
Methods
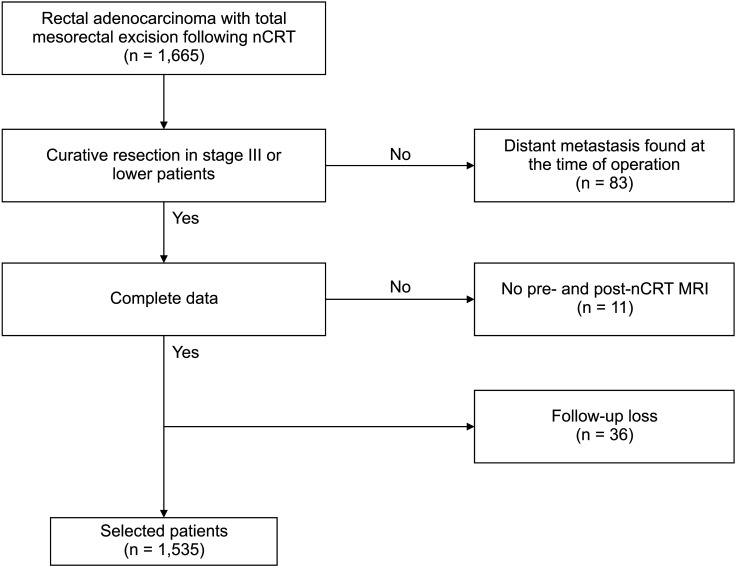
Between January 2008 and December 2016, 1,535 patients who underwent radical resection following nCRT were identified. The association between mLPLN and disease-free survival (DFS), overall survival (OS), local recurrencefree survival (LRFS), and pelvic recurrence-free survival (PRFS) was analyzed, along with risk factors associated with OS and DFS.
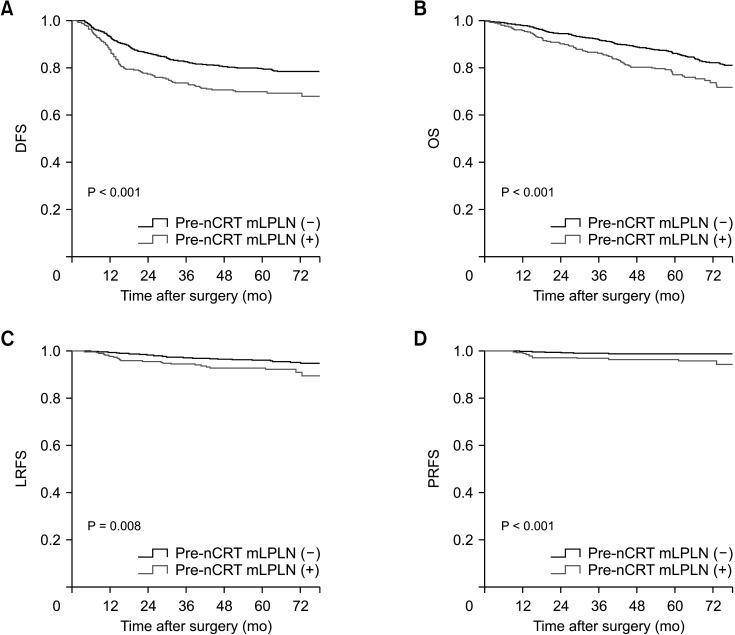
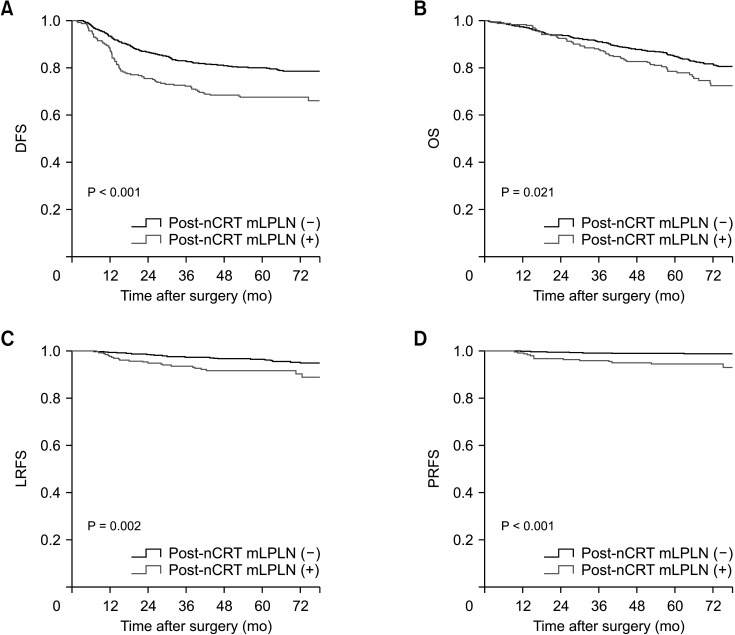
Results
Overall, 329 (21.4%) of the 1,535 patients experienced disease recurrence; 71 (4.6%) had local recurrence, 25 (1.6%) had pelvic recurrence, and 312 (20.3%) had distant recurrence. The pre- and post-nCRT mLPLN (–) groups had better DFS, LRFS, PRFS, and OS than the (+) groups. LPLN sampling (LPLNs) was implemented in 24.0% of the pre-nCRT mLPLN (+) group and in 28.8% of the post-nCRT mLPLN (+) group. There was no significant difference in OS and LRFS between LPLNs group and no LPLNs group in pre- and post-nCRT mLPLN (+) groups. Pre-nCRT mLPLN was associated with poor OS (hazard ratio [HR], 1.43; P = 0.009) and post-nCRT mLPLN was associated with poor DFS (HR, 1.49; P = 0.002).
Conclusion
Pre- and post-nCRT mLPLN (+) have different prognostic effects. Post-nCRT mLPLN appears to be more important for disease control. However, pre-nCRT mLPLN should not be disregarded when devising a treatment strategy since it is an independent risk factor for OS.
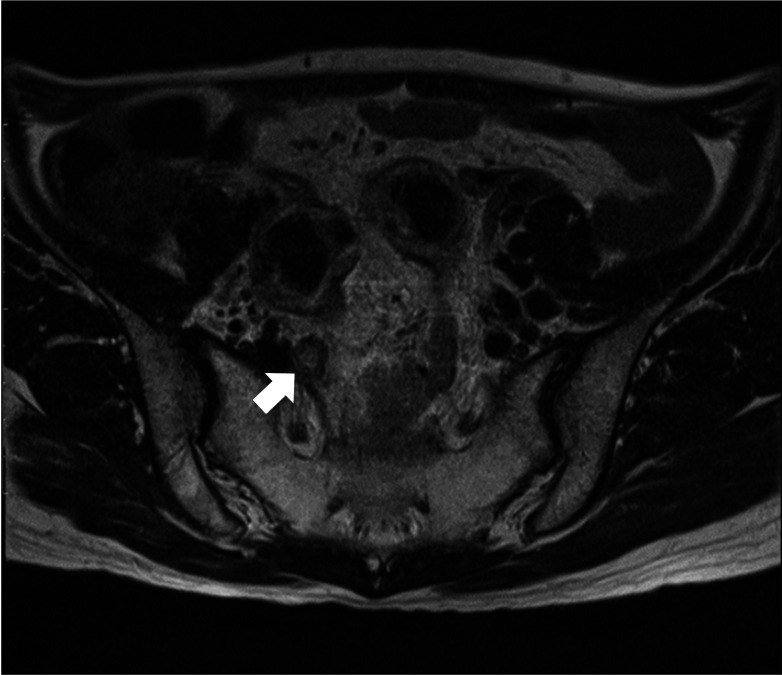
Figure
Cited by 2 articles
-
Multicenter study of prognostic factors in paraaortic lymph node dissection for metastatic colorectal cancer
Jun Woo Bong, Sanghee Kang, Pyoungjae Park
Ann Surg Treat Res. 2023;105(5):271-280. doi: 10.4174/astr.2023.105.5.271.Fluorescence-guided colorectal surgery: applications, clinical results, and protocols
Jin-Min Jung, In Ja Park, Eun Jung Park, Gyung Mo Son,
Ann Surg Treat Res. 2023;105(5):252-263. doi: 10.4174/astr.2023.105.5.252.
Reference
-
1. Enker WE, Thaler HT, Cranor ML, Polyak T. Total mesorectal excision in the operative treatment of carcinoma of the rectum. J Am Coll Surg. 1995; 181:335–346. PMID: 7551328.2. Heald RJ, Moran BJ, Ryall RD, Sexton R, MacFarlane JK. Rectal cancer: the Basingstoke experience of total mesorectal excision, 1978-1997. Arch Surg. 1998; 133:894–899. PMID: 9711965.3. Heald RJ, Ryall RD. Recurrence and survival after total mesorectal excision for rectal cancer. Lancet. 1986; 1:1479–1482. PMID: 2425199.4. Havenga K, Enker WE, Norstein J, Moriya Y, Heald RJ, van Houwelingen HC, et al. Improved survival and local control after total mesorectal excision or D3 lymphadenectomy in the treatment of primary rectal cancer: an international analysis of 1411 patients. Eur J Surg Oncol. 1999; 25:368–374. PMID: 10419706.5. Kapiteijn E, Marijnen CA, Nagtegaal ID, Putter H, Steup WH, Wiggers T, et al. Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer. N Engl J Med. 2001; 345:638–646. PMID: 11547717.6. Sauer R, Becker H, Hohenberger W, Rödel C, Wittekind C, Fietkau R, et al. Preoperative versus postoperative chemoradiotherapy for rectal cancer. N Engl J Med. 2004; 351:1731–1740. PMID: 15496622.7. Das P, Skibber JM, Rodriguez-Bigas MA, Feig BW, Chang GJ, Hoff PM, et al. Clinical and pathologic predictors of locoregional recurrence, distant metastasis, and overall survival in patients treated with chemoradiation and mesorectal excision for rectal cancer. Am J Clin Oncol. 2006; 29:219–224. PMID: 16755173.8. Ueno H, Mochizuki H, Hashiguchi Y, Hase K. Prognostic determinants of patients with lateral nodal involvement by rectal cancer. Ann Surg. 2001; 234:190–197. PMID: 11505064.9. Ueno H, Yamauchi C, Hase K, Ichikura T, Mochizuki H. Clinicopathological study of intrapelvic cancer spread to the iliac area in lower rectal adenocarcinoma by serial sectioning. Br J Surg. 1999; 86:1532–1537. PMID: 10594501.10. Ueno H, Mochizuki H, Hashiguchi Y, Ishiguro M, Miyoshi M, Kajiwara Y, et al. Potential prognostic benefit of lateral pelvic node dissection for rectal cancer located below the peritoneal reflection. Ann Surg. 2007; 245:80–87. PMID: 17197969.11. Ogura A, Konishi T, Cunningham C, Garcia-Aguilar J, Iversen H, Toda S, et al. Neoadjuvant (chemo)radiotherapy with total mesorectal excision only is not sufficient to prevent lateral local recurrence in enlarged nodes: results of the multicenter lateral node study of patients with low cT3/4 rectal cancer. J Clin Oncol. 2019; 37:33–43. PMID: 30403572.12. Kim TG, Park W, Choi DH, Park HC, Kim SH, Cho YB, et al. Factors associated with lateral pelvic recurrence after curative resection following neoadjuvant chemoradiotherapy in rectal cancer patients. Int J Colorectal Dis. 2014; 29:193–200. PMID: 24322736.13. Kim MJ, Kim TH, Kim DY, Kim SY, Baek JY, Chang HJ, et al. Can chemoradiation allow for omission of lateral pelvic node dissection for locally advanced rectal cancer? J Surg Oncol. 2015; 111:459–464. PMID: 25559888.14. Kim TH, Jeong SY, Choi DH, Kim DY, Jung KH, Moon SH, et al. Lateral lymph node metastasis is a major cause of locoregional recurrence in rectal cancer treated with preoperative chemoradiotherapy and curative resection. Ann Surg Oncol. 2008; 15:729–737. PMID: 18057989.15. Georgiou P, Tan E, Gouvas N, Antoniou A, Brown G, Nicholls RJ, et al. Extended lymphadenectomy versus conventional surgery for rectal cancer: a meta-analysis. Lancet Oncol. 2009; 10:1053–1062. PMID: 19767239.16. Malakorn S, Chang GJ. Treatment of rectal cancer in the East and West: should it be different? Surgery. 2017; 162:315–316. PMID: 28619666.17. Sammour T, Chang GJ. Lateral pelvic lymph node dissection and radiation treatment for rectal cancer: mutually exclusive or mutually beneficial? Ann Gastroenterol Surg. 2018; 2:348–350. PMID: 30238075.18. Sammour T, Chang GJ. Lateral node dissection in low rectal cancer: time for a global approach? Ann Surg. 2017; 266:208–209. PMID: 28437315.19. Malakorn S, Yang Y, Bednarski BK, Kaur H, You YN, Holliday EB, et al. Who should get lateral pelvic lymph node dissection after neoadjuvant chemoradiation? Dis Colon Rectum. 2019; 62:1158–1166. PMID: 31490825.20. Otero de Pablos J, Mayol J. Controversies in the management of lateral pelvic lymph nodes in patients with advanced rectal cancer: East or West? Front Surg. 2020; 6:79. PMID: 32010707.21. Garcia-Aguilar J, Cromwell JW, Marra C, Lee SH, Madoff RD, Rothenberger DA. Treatment of locally recurrent rectal cancer. Dis Colon Rectum. 2001; 44:1743–1748. PMID: 11742153.22. Lee KH, Kim JS, Kim JY. Long-term oncologic outcomes of neoadjuvant concurrent chemoradiotherapy with capecitabine and radical surgery in locally advanced rectal cancer: 10-year experiences at a single institution. Ann Surg Treat Res. 2016; 91:178–186. PMID: 27757395.23. Hojo K, Koyama Y, Moriya Y. Lymphatic spread and its prognostic value in patients with rectal cancer. Am J Surg. 1982; 144:350–354. PMID: 7114377.24. Morikawa E, Yasutomi M, Shindou K, Matsuda T, Mori N, Hida J, et al. Distribution of metastatic lymph nodes in colorectal cancer by the modified clearing method. Dis Colon Rectum. 1994; 37:219–223. PMID: 8137667.25. Kim YI, Jang JK, Park IJ, Park SH, Kim JB, Park JH, et al. Lateral lymph node and its association with distant recurrence in rectal cancer: a clue of systemic disease. Surg Oncol. 2020; 35:174–181. PMID: 32889250.26. Zhou S, Jiang Y, Pei W, Liang J, Zhou Z. Prognostic significance of lateral pelvic lymph node dissection for middle-low rectal cancer patients with lateral pelvic lymph node metastasis: a propensity score matching study. BMC Cancer. 2022; 22:136. PMID: 35109810.27. Kim JH, Beets GL, Kim MJ, Kessels AG, Beets-Tan RG. High-resolution MR imaging for nodal staging in rectal cancer: are there any criteria in addition to the size? Eur J Radiol. 2004; 52:78–83. PMID: 15380850.28. Lee D, Matsuda T, Yamashita K, Hasegawa H, Yamamoto M, Kanaji S, et al. Significance of lateral pelvic lymph node size in predicting metastasis and prognosis in rectal cancer. Anticancer Res. 2019; 39:993–998. PMID: 30711986.29. Fujita S, Akasu T, Mizusawa J, Saito N, Kinugasa Y, Kanemitsu Y, et al. Postoperative morbidity and mortality after mesorectal excision with and without lateral lymph node dissection for clinical stage II or stage III lower rectal cancer (JCOG0212): results from a multicentre, randomised controlled, non-inferiority trial. Lancet Oncol. 2012; 13:616–621. PMID: 22591948.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Implication of Lateral Pelvic Lymph Node Metastasis in Rectal Cancer Treated with Neoadjuvant Chemoradiotherapy
- ERRATUM: Difference in prognostic impact of lateral pelvic lymph node metastasis between pre- and post-neoadjuvant chemoradiotherapy in rectal cancer patients
- Lateral Pelvic Lymph Node Dissection After Neoadjuvant Chemoradiotherapy in Patients With Rectal Cancer: A Single-Center Experience and Literature Review
- Lateral Lymph Node Dissection With the Focus on Indications, Functional Outcomes, and Minimally Invasive Surgery
- Effect on the Local Recurrence and the Survival of Total Mesorectal Excision and Lateral Pelvic Lymph Node Dissection in Rectal Cancer