Blood Res.
2023 Mar;58(1):42-50. 10.5045/br.2023.2022218.
Acquired von willebrand syndrome in patients with Philadelphia-negative myeloproliferative neoplasm
- Affiliations
-
- 1Division of Hematology/Oncology, Department of Internal Medicine, Chungnam National University College of Medicine, Daejeon, Korea
- KMID: 2541064
- DOI: http://doi.org/10.5045/br.2023.2022218
Abstract
- Background
Acquired von Willebrand syndrome (AVWS) has not been investigated in Korean patients with Philadelphia chromosome-negative myeloproliferative neoplasm.
Methods
This study analyzed the prevalence at diagnosis and clinical features of AVWS in patients with essential thrombocythemia (ET), polycythemia vera (PV), prefibrotic/early primary myelofibrosis (pre-PMF), or overt PMF (PMF) diagnosed between January 2019 and December 2021 at Chungam National University Hospital, Daejeon, Korea. AVWS was defined as below the lower reference limit (56%) of ristocetin cofactor activity (VWF:RCo).
Results
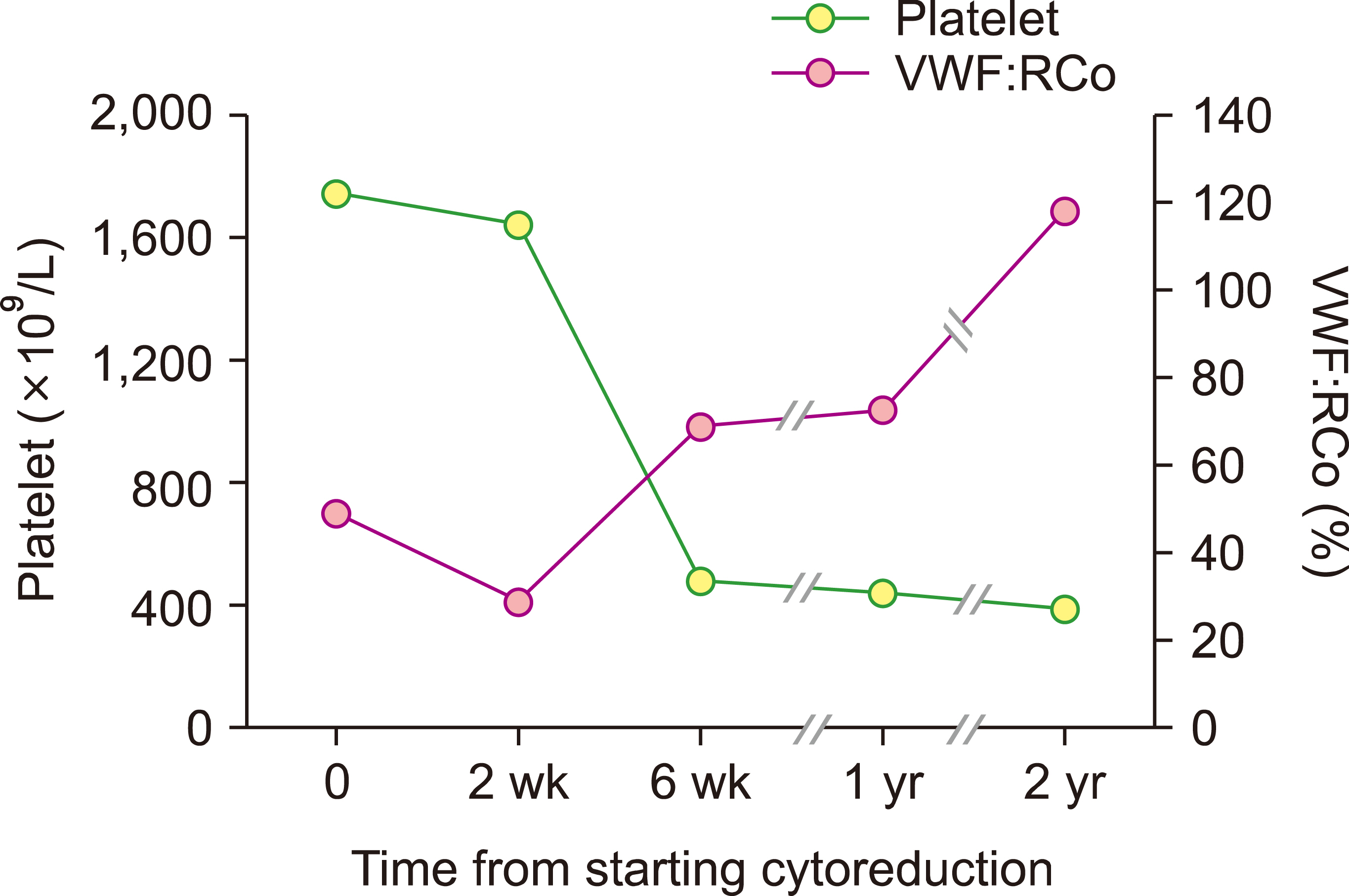
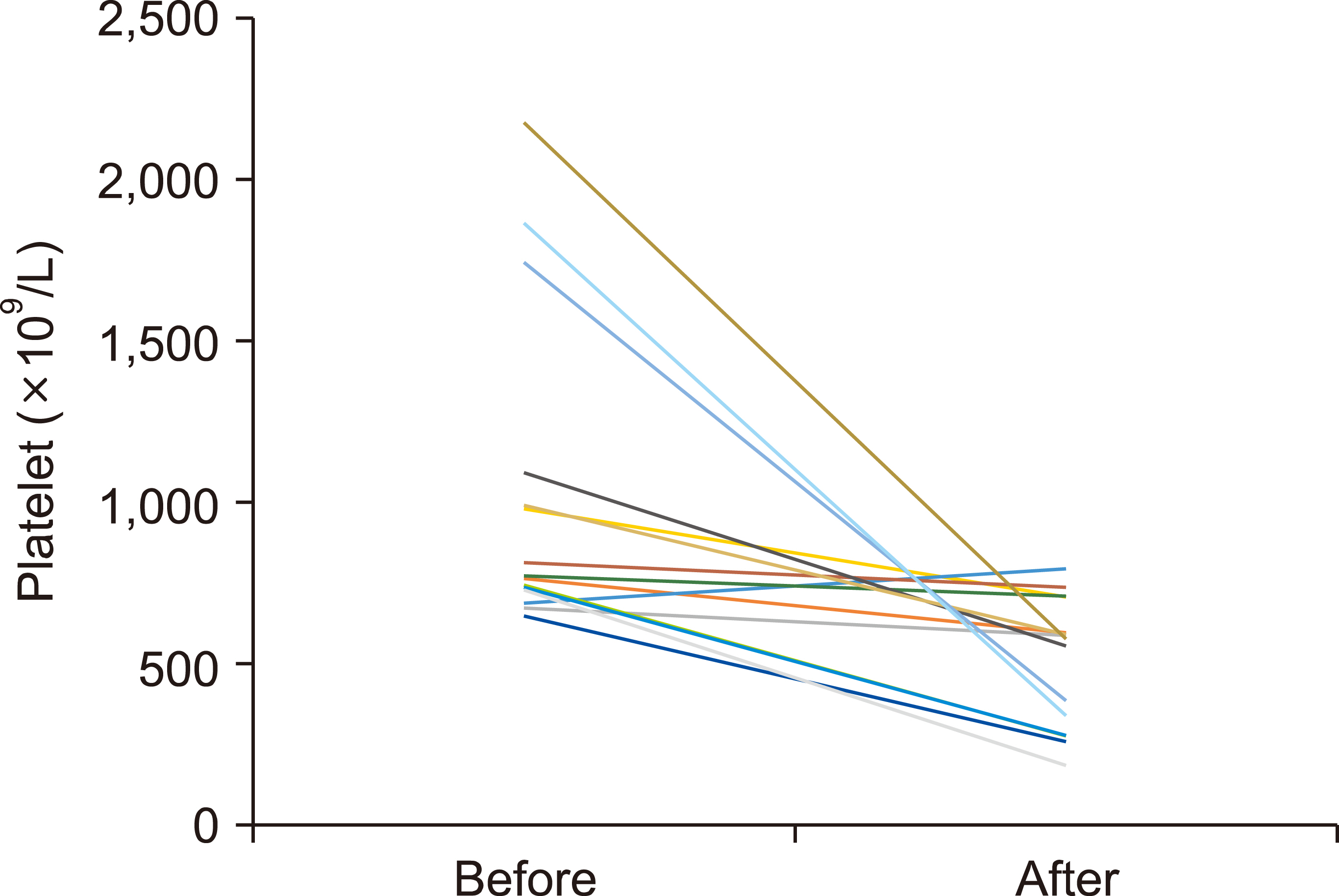
Sixty-four consecutive patients (36 with ET, 17 with PV, 6 with pre-PMF, and 5 with PMF; 30 men and 34 women) with a median age of 67 years (range, 18‒87 yr) were followed for a median of 25.1 months (range, 2.6‒46.4 mo). AVWS was detected in 20 (31.3%) patients at diagnosis and was most frequent in ET patients (41.4%), followed by patients with pre-PMF (33.3%) and PV (17.6%) patients. VWF:RCo was negatively correlated with the platelet count (r=0.937; P =0.002). Only one episode of minor bleeding occurred in a patient with ET and AVWS. Younger age (<50 yr) [odds ratio (OR), 7.08; 95% confidence interval (CI), 1.27‒39.48; P =0.026] and thrombocytosis (>600×10 9 /L) (OR, 13.70; 95% CI, 1.35‒138.17; P =0.026) were independent risk factors for developing AVWS.
Conclusion
AVWS based on VWF:RCo was common in patients with ET and pre-PMF, but less common in patients with PV in the Korean population. Clinically significant bleeding is rare in these patients.
Keyword
Figure
Reference
-
1. Song IC, Yeon SH, Lee MW, et al. 2021; Thrombotic and hemorrhagic events in 2016 World Health Organization-defined Philadelphia- negative myeloproliferative neoplasm. Korean J Intern Med. 36:1190–203. DOI: 10.3904/kjim.2020.634. PMID: 34289585. PMCID: PMC8435504. PMID: 1171ae3cdf6c42e4a204252610a84058.
Article2. Song IC, Yeon SH, Lee MW, et al. 2022; Myelofibrotic and leukemic transformation in 2016 WHO-defined Philadelphia-negative myeloproliferative neoplasm. Blood Res. 57:59–68. DOI: 10.5045/br.2021.2021209. PMID: 35256550. PMCID: PMC8958372.
Article3. van Genderen PJ, Leenknegt H, Michiels JJ, Budde U. 1996; Acquired von Willebrand disease in myeloproliferative disorders. Leuk Lymphoma. 22(Suppl 1):79–82. DOI: 10.3109/10428199609074364. PMID: 8951776.
Article4. Weyand AC, Flood VH. 2021; Von Willebrand disease: current status of diagnosis and management. Hematol Oncol Clin North Am. 35:1085–101. DOI: 10.1016/j.hoc.2021.07.004. PMID: 34400042. PMCID: PMC8919990.5. Langer AL, Connell NT. 2021; Acquired von Willebrand syndrome. Hematol Oncol Clin North Am. 35:1103–16. DOI: 10.1016/j.hoc.2021.07.005. PMID: 34391604.
Article6. Biguzzi E, Siboni SM, Peyvandi F. 2020; How I treat gastrointestinal bleeding in congenital and acquired von Willebrand disease. Blood. 136:1125–33. DOI: 10.1182/blood.2019003702. PMID: 32584960.
Article7. Awada H, Voso MT, Guglielmelli P, Gurnari C. 2020; Essential thrombocythemia and acquired von Willebrand syndrome: the shadowlands between thrombosis and bleeding. Cancers (Basel). 12:1746. DOI: 10.3390/cancers12071746. PMID: 32629973. PMCID: PMC7407619. PMID: f848ec192cf64638bc5639cee75ebecb.
Article8. Koren-Michowitz M, Lavi N, Ellis MH, Vannucchi AM, Mesa R, Harrison CN. 2017; Management of extreme thrombocytosis in myeloproliferative neoplasms: an international physician survey. Ann Hematol. 96:87–92. DOI: 10.1007/s00277-016-2826-4. PMID: 27734130.
Article9. Choi KS, Kim JM, Ryu JI, Oh YH. 2015; Concurrent ruptured pseudoaneurysm of the internal carotid artery and cerebral infarction as an initial manifestation of polycythemia vera. J Korean Neurosurg Soc. 58:137–40. DOI: 10.3340/jkns.2015.58.2.137. PMID: 26361530. PMCID: PMC4564746.
Article10. Kim SY, Bae SH, Bang SM, et al. 2021; The 2020 revision of the guidelines for the management of myeloproliferative neoplasms. Korean J Intern Med. 36:45–62. DOI: 10.3904/kjim.2020.319. PMID: 33147902. PMCID: PMC7820646. PMID: 9e4b5446bcec4caa9c9db822e52ba48a.
Article11. Choi CW, Bang SM, Jang S, et al. 2015; Guidelines for the management of myeloproliferative neoplasms. Korean J Intern Med. 30:771–88. DOI: 10.3904/kjim.2015.30.6.771. PMID: 26552452. PMCID: PMC4642006.
Article12. Lim Y, Lee JO, Bang SM. 2016; Incidence, survival and prevalence statistics of classical myeloproliferative neoplasm in Korea. J Korean Med Sci. 31:1579–85. DOI: 10.3346/jkms.2016.31.10.1579. PMID: 27550486. PMCID: PMC4999400.
Article13. Byun JM, Kim YJ, Youk T, Yang JJ, Yoo J, Park TS. 2017; Real world epidemiology of myeloproliferative neoplasms: a population based study in Korea 2004-2013. Ann Hematol. 96:373–81. DOI: 10.1007/s00277-016-2902-9. PMID: 28028559.
Article14. Passamonti F, Thiele J, Girodon F, et al. 2012; A prognostic model to predict survival in 867 World Health Organization-defined essential thrombocythemia at diagnosis: a study by the International Working Group on Myelofibrosis Research and Treatment. Blood. 120:1197–201. DOI: 10.1182/blood-2012-01-403279. PMID: 22740446.
Article15. Cervantes F, Dupriez B, Pereira A, et al. 2009; New prognostic scoring system for primary myelofibrosis based on a study of the International Working Group for Myelofibrosis Research and Treatment. Blood. 113:2895–901. DOI: 10.1182/blood-2008-07-170449. PMID: 18988864.
Article16. Mital A, Prejzner W, Świątkowska-Stodulska R, Hellmann A. 2015; Factors predisposing to acquired von Willebrand syndrome during the course of polycythemia vera - retrospective analysis of 142 consecutive cases. Thromb Res. 136:754–7. DOI: 10.1016/j.thromres.2015.07.029. PMID: 26269222.
Article17. Rottenstreich A, Kleinstern G, Krichevsky S, Varon D, Lavie D, Kalish Y. 2017; Factors related to the development of acquired von Willebrand syndrome in patients with essential thrombocythemia and polycythemia vera. Eur J Intern Med. 41:49–54. DOI: 10.1016/j.ejim.2016.11.011. PMID: 27919526.
Article18. Lee MW, Yeon SH, Ryu H, et al. 2021; Volumetric splenomegaly in patients with essential thrombocythemia and prefibrotic/early primary myelofibrosis. Int J Hematol. 114:35–43. DOI: 10.1007/s12185-021-03121-x. PMID: 33704663.
Article19. Connell NT, James PD, Brignardello-Petersen R, et al. 2021; von Willebrand disease: proposing definitions for future research. Blood Adv. 5:565–9. DOI: 10.1182/bloodadvances.2020003620. PMID: 33496750. PMCID: PMC7839375.20. Kander EM, Raza S, Zhou Z, et al. 2015; Bleeding complications in BCR-ABL negative myeloproliferative neoplasms: prevalence, type, and risk factors in a single-center cohort. Int J Hematol. 102:587–93. DOI: 10.1007/s12185-015-1871-4. PMID: 26440973.
Article21. Lancellotti S, Dragani A, Ranalli P, et al. 2015; Qualitative and quantitative modifications of von Willebrand factor in patients with essential thrombocythemia and controlled platelet count. J Thromb Haemost. 13:1226–37. DOI: 10.1111/jth.12967. PMID: 25876231.
Article22. Nitu-Whalley IC, Lee CA, Griffioen A, Jenkins PV, Pasi KJ. 2000; Type 1 von Willebrand disease - a clinical retrospective study of the diagnosis, the influence of the ABO blood group and the role of the bleeding history. Br J Haematol. 108:259–64. DOI: 10.1046/j.1365-2141.2000.01830.x. PMID: 10691852.
Article23. Goyal J, Reddy VV, Marques MB. 2013; Acquired von Willebrand's disease in myelofibrosis and essential thrombocythemia. Haemophilia. 19:e256–7. DOI: 10.1111/hae.12152. PMID: 23590694.
Article24. Adam R, Priglinger M, Harrington T, Gottlieb D, Krause M. 2014; An unusual cause of cerebellar hemorrhage in a young patient: essential thrombocythemia. J Stroke Cerebrovasc Dis. 23:e373–4. DOI: 10.1016/j.jstrokecerebrovasdis.2013.12.013. PMID: 24582788.
Article25. Rupa-Matysek J, Lewandowski K, Lewandowska M, et al. 2015; Bleeding complications after arthroscopy in a JAK2V617F- positive patient with essential thrombocythemia and acquired von Willebrand syndrome (AVWS). Int J Hematol. 101:405–10. DOI: 10.1007/s12185-014-1707-7. PMID: 25432436.
Article26. Kanderi T, Puthenpura M, Shrimanker I, Sapna F, Felter SC. 2020; Triple-negative essential thrombocythemia complicated by thrombosis and acquired von Willebrand disease in a young man. Am J Case Rep. 21:e924560. DOI: 10.12659/AJCR.924560.
Article27. Tefferi A, Szuber N, Pardanani A, et al. 2021; Extreme thrombocytosis in low-risk essential thrombocythemia: retrospective review of vascular events and treatment strategies. Am J Hematol. 96:E182–4. DOI: 10.1002/ajh.26137. PMID: 33617676.
Article28. Budde U, van Genderen PJ. 1997; Acquired von Willebrand disease in patients with high platelet counts. Semin Thromb Hemost. 23:425–31. DOI: 10.1055/s-2007-996119. PMID: 9387201.
Article29. Tefferi A, Barbui T. 2020; Polycythemia vera and essential thrombo-cythemia: 2021 update on diagnosis, risk-stratification and management. Am J Hematol. 95:1599–613. DOI: 10.1002/ajh.26008. PMID: 32974939.
Article30. Tatewaki W, Takahashi H, Shibata A. 1988; Multimeric composition of plasma von Willebrand factor in chronic myeloproliferative disorders. Clin Lab Haematol. 10:417–25. DOI: 10.1111/j.1365-2257.1988.tb01190.x. PMID: 3150698.
Article31. Tatewaki W, Shibata A. 1989; Acquired von Willebrand disease in patients with chronic myeloproliferative disorders. Leuk Lymphoma. 1:51–7. DOI: 10.3109/10428198909042459. PMID: 27456408.
Article32. Kubo M, Sakai K, Hayakawa M, et al. 2022; Increased cleavage of von Willebrand factor by ADAMTS13 may contribute strongly to acquired von Willebrand syndrome development in patients with essential thrombocythemia. J Thromb Haemost. 20:1589–98. DOI: 10.1111/jth.15717. PMID: 35352474.
Article33. Barbui T, Tefferi A, Vannucchi AM, et al. 2018; Philadelphia chromosome-negative classical myeloproliferative neoplasms: revised management recommendations from European LeukemiaNet. Leukemia. 32:1057–69. DOI: 10.1038/s41375-018-0077-1. PMID: 29515238. PMCID: PMC5986069.
Article34. Tefferi A, Smock KJ, Divgi AB. 2010; Polycythemia vera-associated acquired von Willebrand syndrome despite near-normal platelet count. Am J Hematol. 85:545. DOI: 10.1002/ajh.21730. PMID: 20575028.
Article35. Michiels JJ, Berneman Z, Schroyens W, Finazzi G, Budde U, van Vliet HH. 2006; The paradox of platelet activation and impaired function: platelet-von Willebrand factor interactions, and the etiology of thrombotic and hemorrhagic manifestations in essential thrombocythemia and polycythemia vera. Semin Thromb Hemost. 32:589–604. DOI: 10.1055/s-2006-949664. PMID: 16977569.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Laboratory assessment of von Willebrand factor for classification of von Willebrand disease
- Erythromelalgia and Livedo Reticularis in a Patient with Essential Thrombocythemia, Acquired von Willebrand Disease, and Elevated Anti-Phospholipid Antibodies
- Three cases of type I von Willebrand disease in a family
- Acquired von Willebrand Syndrome Associated with Amyloidosis
- von Willebrand Disease