J Korean Med Sci.
2023 Mar;38(12):e98. 10.3346/jkms.2023.38.e98.
Temporal Change in the Use of Laboratory and Imaging Tests in One Week Before Death, 2006–2015
- Affiliations
-
- 1Division of Rheumatology, Hallym University Sacred Heart Hospital, Anyang, Korea
- 2Institute for Skeletal Aging, Hallym University, Chuncheon, Korea
- 3Division of Data Science, Data Science Convergence Research Center, Hallym University, Chuncheon, Korea
- KMID: 2541042
- DOI: http://doi.org/10.3346/jkms.2023.38.e98
Abstract
- Background
To analyze the trends in laboratory and imaging test use 1 week before death among decedents who died in Korean hospitals, tests used per decedents from 2006 to 2015 were examined by using the National Health Insurance Service-Elderly Sample Cohort (NHISESC) dataset.
Methods
The study population consisted of decedents aged ≥ 60 years old with a history of admission and death at a hospital, and tests recorded in the payment claims for laboratory and imaging tests according to the Healthcare Common Procedure Coding System codes were examined. Twenty-eight laboratory and 6 imaging tests were selected. For each year, crude rates of test use per decedents in each age and sex stratum were calculated. Regression analysis was used to examine the temporal changes in the test use.
Results
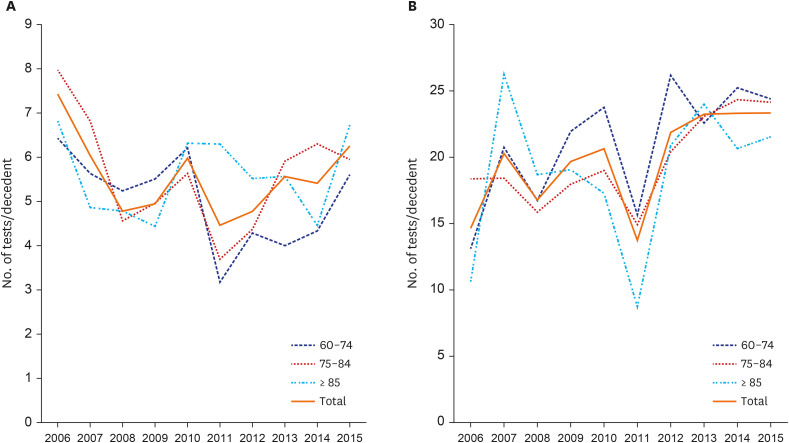
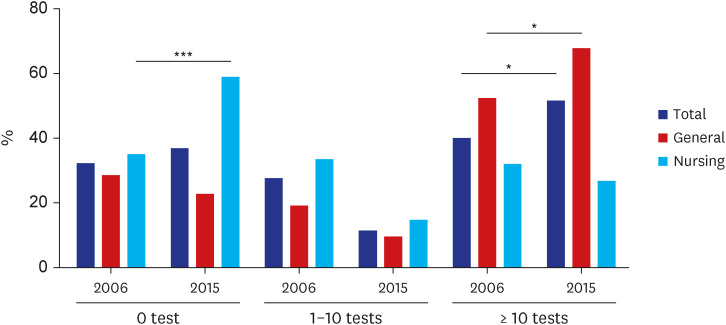
During the follow-up period, 6,638 subjects included in the sample cohort died. The number of total laboratory and imaging tests performed on the deceased increased steadily throughout the study year from 10.3 tests/deceased in 2006 to 16.6 tests/deceased in 2015. The use of tests increased significantly in general hospitals, however, not in nursing hospitals. Laboratory tests showed yearly increase, from 9.46/deceased in 2006 to 15.57/ deceased in 2015, an annual increase of 7.39%. On the other hand, the use of imaging increased from 0.86/deceased in 2006 to 1.01/deceased in 2015, which was not statistically significant.
Conclusion
The use of tests, especially laboratory tests, increased steadily over the years even among those elderly patients at imminent death. Reducing acute healthcare at the end of life would be one target not only to support the sustainability of the health care budget but also to improve the quality of dying and death.
Keyword
Figure
Cited by 1 articles
-
Comparison of factors influencing the decision to withdraw life-sustaining treatment in intensive care unit patients after implementation of the Life-Sustaining Treatment Act in Korea
Claire Junga Kim, Kyung Sook Hong, Sooyoung Cho, Jin Park
Acute Crit Care. 2024;39(2):294-303. doi: 10.4266/acc.2023.01130.
Reference
-
1. Clark D. Between hope and acceptance: the medicalisation of dying. BMJ. 2002; 324(7342):905–907. PMID: 11950744.2. Lehnert T, Heider D, Leicht H, Heinrich S, Corrieri S, Luppa M, et al. Review: health care utilization and costs of elderly persons with multiple chronic conditions. Med Care Res Rev. 2011; 68(4):387–420. PMID: 21813576.3. Canova C, Anello P, Barbiellini Amidei C, Parolin V, Zanier L, Simonato L. Use of healthcare services at the end of life in decedents compared to their surviving counterparts: a case-control study among adults born before 1946 in Friuli Venezia Giulia. PLoS One. 2019; 14(2):e0212086. PMID: 30730965.4. Zweifel P, Felder S, Meiers M. Ageing of population and health care expenditure: a red herring? Health Econ. 1999; 8(6):485–496. PMID: 10544314.5. Brownlee S, Chalkidou K, Doust J, Elshaug AG, Glasziou P, Heath I, et al. Evidence for overuse of medical services around the world. Lancet. 2017; 390(10090):156–168. PMID: 28077234.6. Riley GF, Lubitz JD. Long-term trends in Medicare payments in the last year of life. Health Serv Res. 2010; 45(2):565–576. PMID: 20148984.7. Tanuseputro P, Wodchis WP, Fowler R, Walker P, Bai YQ, Bronskill SE, et al. The health care cost of dying: a population-based retrospective cohort study of the last year of life in Ontario, Canada. PLoS One. 2015; 10(3):e0121759. PMID: 25811195.8. Ha YS, Kim SY, Chung JI, Choi H, Kim JH, Yu HS, et al. Trends in end-of-life resource utilization and costs among prostate cancer patients from 2006 to 2015: a nationwide population-based study. World J Mens Health. 2021; 39(1):158–167. PMID: 33350174.9. Kang DW, Shim YB, Lee EK, Park MH. Healthcare resource utilization and medical costs in patients with terminal cancer during best supportive care. PLoS One. 2022; 17(6):e0269565. PMID: 35657991.10. McNeil MJ, Kamal AH, Kutner JS, Ritchie CS, Abernethy AP. The burden of polypharmacy in patients near the end of life. J Pain Symptom Manage. 2016; 51(2):178–83.e2. PMID: 26432571.11. Currow DC, Stevenson JP, Abernethy AP, Plummer J, Shelby-James TM. Prescribing in palliative care as death approaches. J Am Geriatr Soc. 2007; 55(4):590–595. PMID: 17397439.12. Nauck F, Ostgathe C, Klaschik E, Bausewein C, Fuchs M, Lindena G, et al. Drugs in palliative care: results from a representative survey in Germany. Palliat Med. 2004; 18(2):100–107. PMID: 15046406.13. Cadamuro J, Ibarz M, Cornes M, Nybo M, Haschke-Becher E, von Meyer A, et al. Managing inappropriate utilization of laboratory resources. Diagnosis (Berl). 2019; 6(1):5–13. PMID: 30096052.14. Kang SH, Seo YI, Lee MH, Kim HA. Diagnostic value of anti-nuclear antibodies: results from Korean university-affiliated hospitals. J Korean Med Sci. 2022; 37(19):e159. PMID: 35578590.15. O’Sullivan JW, Stevens S, Hobbs FD, Salisbury C, Little P, Goldacre B, et al. Temporal trends in use of tests in UK primary care, 2000–15: retrospective analysis of 250 million tests. BMJ. 2018; 363:k4666. PMID: 30487169.16. Jang BS, Chang JH. Socioeconomic status and survival outcomes in elderly cancer patients: A national health insurance service-elderly sample cohort study. Cancer Med. 2019; 8(7):3604–3613. PMID: 31066516.17. Koo BK, Lee CH, Yang BR, Hwang SS, Choi NK. The incidence and prevalence of diabetes mellitus and related atherosclerotic complications in Korea: a National Health Insurance Database Study. PLoS One. 2014; 9(10):e110650. PMID: 25329714.18. Lord Carter of Coles. Report of the review of NHS pathology services in England. Updated 2006. Accessed June 21, 2022. https://www.networks.nhs.uk/nhs-networks/peninsula-pathology-network/documents/CarterReviewPathologyReport.pdf .19. Koch H, van Bokhoven MA, ter Riet G, Hessels KM, van der Weijden T, Dinant GJ, et al. What makes general practitioners order blood tests for patients with unexplained complaints? A cross-sectional study. Eur J Gen Pract. 2009; 15(1):22–28. PMID: 19363746.20. Johnson PC, Markovitz NH, Yi A, Newcomb RA, Amonoo HL, Nelson AM, et al. End-of-life care for older adults with aggressive non-Hodgkin lymphoma. J Palliat Med. 2022; 25(5):728–733. PMID: 34724798.21. Khaki AR, Xu Y, Cheung WY, Li L, Fedorenko C, Grivas P, et al. Comparison of health care utilization at the end of life among patients with cancer in Alberta, Canada, versus Washington State. JCO Oncol Pract. 2020; 16(12):e1543–e1552. PMID: 32804586.22. Hoffmann TC, Del Mar C. Patients’ expectations of the benefits and harms of treatments, screening, and tests: a systematic review. JAMA Intern Med. 2015; 175(2):274–286. PMID: 25531451.23. Hoffmann TC, Del Mar C. Clinicians’ expectations of the benefits and harms of treatments, screening, and tests: a systematic review. JAMA Intern Med. 2017; 177(3):407–419. PMID: 28097303.24. Kim JR, Byun SJ, Son DS, Kim HA. Correlation between the ratio of physician consultation fees to hourly minimum wage and consultation length: a cross-sectional study of nine countries. BMJ Open. 2022; 12(12):e064369.25. Kim HA, Kim MG. A survey study on rheumatologist consultation time in Korean hospitals. J Rheum Dis. 2020; 27(1):45–50.26. Carrier ER, Reschovsky JD, Katz DA, Mello MM. High physician concern about malpractice risk predicts more aggressive diagnostic testing in office-based practice. Health Aff (Millwood). 2013; 32(8):1383–1391. PMID: 23918482.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Malignant Melanoma of the Temporal Bone Initially Presenting with Dizziness
- Comparison of Corneal Astigmatism According to the Distance between Limbus and Internal Lip after Temporal Incision Cataract Surgery
- Temporal Lobe Volume in Geriatric Depressive Patients: A Magnetic Resonance Imaging Study
- Hemorrhagic Fever with Renal Syndrome Complicated by Cochlear Hemorrhage and Abducens Nerve Palsy
- Determining Brain Death