J Cerebrovasc Endovasc Neurosurg.
2023 Mar;25(1):81-86. 10.7461/jcen.2022.E2022.03.005.
Stent-assisted coiling of a ruptured basilar artery perforator aneurysm: A case report
- Affiliations
-
- 1Department of Neurosurgery, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- 2Department of Radiology, Gangnam Severance Hospitla, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2540811
- DOI: http://doi.org/10.7461/jcen.2022.E2022.03.005
Abstract
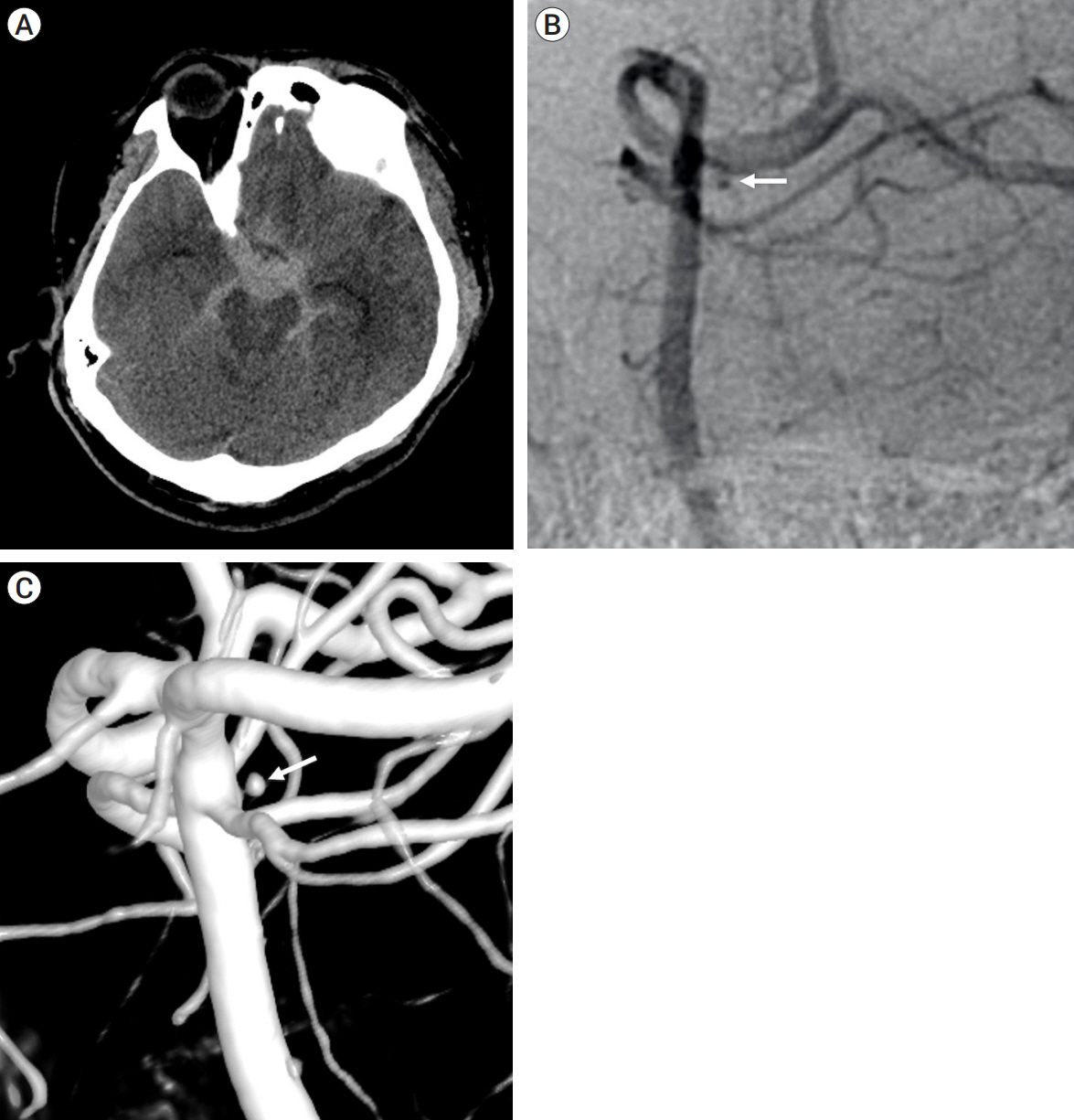
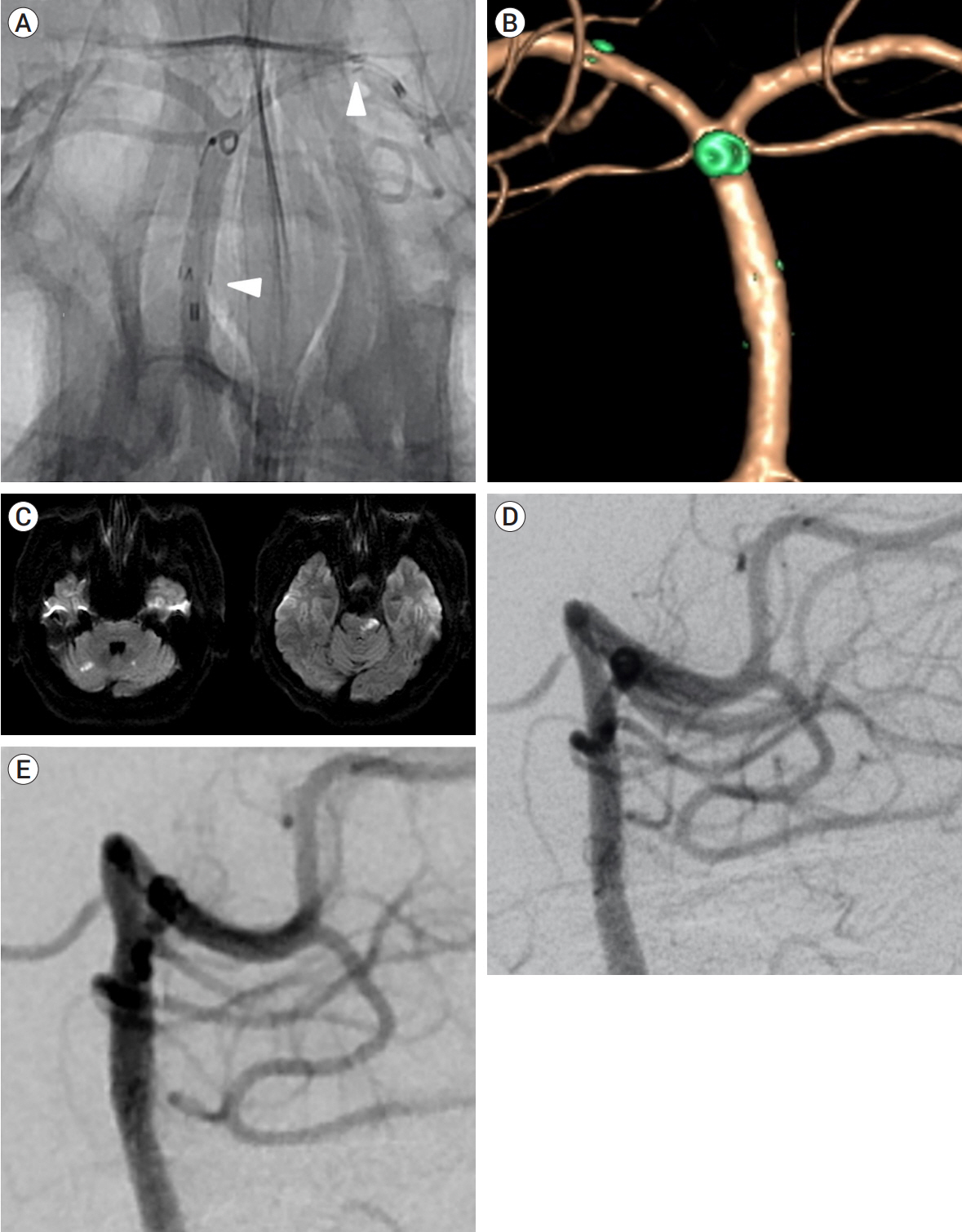
- Basilar artery (BA) perforator aneurysms are exceedingly rare causes of subarachnoid hemorrhage. Therefore, the natural history and optimal treatment have not been established, and surgical, endovascular, and conservative management have been used. However, there is no consensus on the optimal treatment strategy. Herein, we report the case of a 52-year-old man presenting with a ruptured BA perforator aneurysm. First, we deployed an Enterprise stent from the left P1 segment to the BA because the microcatheter could not enter the aneurysm. Then, we deployed a helical coil on the orifice of the BA perforator. Finally, we deployed another Enterprise stent, sandwiching the helical coil between the two Enterprise stents. The aneurysm was completely obliterated without recurrence on the follow-up angiography. Our technique of sandwiching the small helical coil between two Enterprise stents might help other surgeons by offering another feasible treatment option for ruptured BA perforator aneurysms.
Figure
Reference
-
1. Apok V, Tarnaris A, Brydon HL. An unusual aneurysm of a basilar perforating artery presenting with a subarachnoid haemorrhage. Br J Neurosurg. 2013; Feb. 27(1):105–7.2. Bhogal P, AlMatter M, Hellstern V, Perez MA, Lehmberg J, Ganslandt O, et al. Basilar artery perforator aneurysms: report of 9 cases and review of the literature. J Clin Neurosci. 2019; May. 63:122–9.3. Brinjikji W, Lanzino G, Cloft HJ, Rabinstein A, Kallmes DF. Endovascular treatment of very small (3 mm or smaller) intracranial aneurysms: report of a consecutive series and a meta-analysis. Stroke. 2010; Jan. 41(1):116–21.4. Caruso G, Vincentelli F, Giudicelli G, Grisoli F, Xu T, Gouaze A. Perforating branches of the basilar bifurcation. J Neurosurg. 1990; Aug. 73(2):259–65.5. Chalouhi N, Jabbour P, Starke RM, Zanaty M, Tjoumakaris S, Rosenwasser RH, et al. Treatment of a basilar trunk perforator aneurysm with the pipeline embolization device: case report. Neurosurgery. 2014; Jun. 74(6):E697–701. discussion 701.6. Chau Y, Sachet M, Sedat J. Should we treat aneurysms in perforator arteries from the basilar trunk? Review of 49 cases published in the literature and presentation of three personal cases. Interv Neuroradiol. 2018; Feb. 24(1):22–8.7. Chen L, Chen E, Chotai S, Tian X. An endovascular approach to ruptured aneurysms of the circumferential branch of the basilar artery. J Clin Neurosci. 2012; Apr. 19(4):527–31.8. Ding D, Starke RM, Jensen ME, Evans AJ, Kassell NF, Liu KC. Perforator aneurysms of the posterior circulation: case series and review of the literature. J Neurointerv Surg. 2013; Nov. 5(6):546–51.9. Finitsis S, Derelle AL, Tonnelet R, Anxionnat R, Bracard S. Basilar perforator aneurysms: presentation of 4 cases and review of the literature. World Neurosurg. 2017; Jan. 97:366–73.10. Fiorella D, Albuquerque FC, Deshmukh VR, Woo HH, Rasmussen PA, Masaryk TJ, et al. Endovascular reconstruction with the Neuroform stent as monotherapy for the treatment of uncoilable intradural pseudoaneurysms. Neurosurgery. 2006; Aug. 59(2):291–300. discussion 291.11. Forbrig R, Eckert B, Ertl L, Patzig M, Brem C, Vollmar C, et al. Ruptured basilar artery perforator aneurysms--treatment regimen and long-term follow-up in eight cases. Neuroradiology. 2016; Mar. 58(3):285–91.12. Ghogawala Z, Shumacher JM, Ogilvy CS. Distal basilar perforator artery aneurysm: case report. Neurosurgery. 1996; Aug. 39(2):393–6.13. Granja MF, Monteiro A, Agnoletto GJ, Jamal S, Sauvageau E, Aghaebrahim A, et al. A systematic review of non-trunk basilar perforator aneurysms: is it worth chasing the small fish? J Neurointerv Surg. 2020; Apr. 12(4):412–6.14. Maeoka R, Nakagawa I, Ohnishi H, Nakase H. Overlapping stetns with coil sandwich for ruptured blood-blister aneurysm in a patient with ipsilateral persistent primitive trigeminal artery: a case report and review of literature. Asian J Neurosurg. 2019; Nov. 14(4):1236–9.15. Mathieson CS, Barlow P, Jenkins S, Hanzely Z. An unusual case of spontaneous subarachnoid haemorrhage - a ruptured aneurysm of a basilar perforator artery. Br J Neurosurg. 2010; Jun. 24(3):291–3.16. Peschillo S, Caporlingua A, Cannizzaro D, Resta M, Burdi N, Valvassori L, et al. Flow diverter stent treatment for ruptured basilar trunk perforator aneurysms. J Neurointerv Surg. 2016; Feb. 8(2):190–6.17. Satti SR, Vance AZ, Fowler D, Farmah AV, Sivapatham T. Basilar artery perforator aneurysms (BAPAs): review of the literature and classification. J Neurointerv Surg. 2017; Jul. 9(7):669–73.18. Shlobin NA, Cantrell DR, Ansari SA, Hurley MC, Shaibani A, Jahromi BS, et al. Conservative management and natural history of ruptured basilar perforator artery aneurysms: two cases and literature review. World Neurosurg. 2020; Jun. 138:218–22.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Kissing Aneurysms at Fenestrated Proximal Basilar Artery: Double-barrel Stent-assisted Coiling Using Dual Closed-cell Stents
- Fusiform “True” Posterior Communicating Artery Aneurysm with Basilar Artery Occlusion: A Case Report
- Double Microcatheter-Assisted Coiling of a Basilar Artery Fenestration Aneurysm
- Double Stent Assist Coiling of Ruptured Large Saccular Aneurysm in Proximal Basilar Artery Fenestration
- Delayed Self-expansion Phenomenon as a Complication of Neuroform Stent Assisted Coiling for Ruptured Intracranial Aneurysm