Clin Endosc.
2023 Mar;56(2):155-163. 10.5946/ce.2022.218.
Role of radiofrequency ablation in advanced malignant hilar biliary obstruction
- Affiliations
-
- 1Department of Gastroenterology and Hepatology, Kindai University Faculty of Medicine, Osaka-Sayama, Japan
- 2Division of Gastroenterology and Hepatology, Department of Internal Medicine, Soonchunhyang University Cheonan Hospital, Soonchunhyang University School of Medicine, Cheonan, Korea
- KMID: 2540730
- DOI: http://doi.org/10.5946/ce.2022.218
Abstract
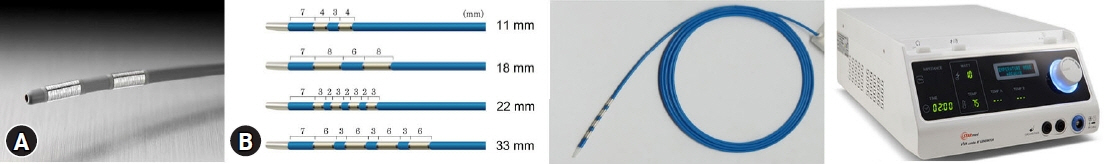
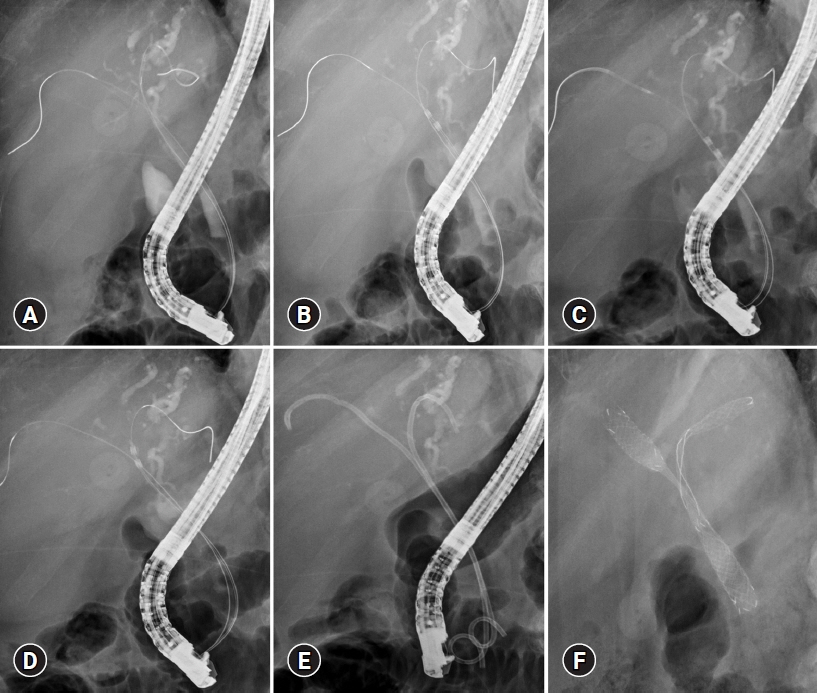
- Malignant hilar biliary obstruction (MHO), an aggressive perihilar biliary obstruction caused by cholangiocarcinoma, gallbladder cancer, or other metastatic malignancies, has a poor prognosis. Surgical resection is the only curative treatment for biliary malignancies. However, the majority of patients with MHO cannot undergo surgery on presentation because of an advanced inoperable state or a poor performance state due to old age or comorbid diseases. Therefore, palliative biliary drainage is mandatory to improve symptomatic jaundice and the quality of life. Among the drainage methods, endoscopic biliary drainage is the current standard for palliation of unresectable advanced MHO. In addition, combined with endoscopic drainage, additional local ablation therapies, such as photodynamic therapy or radiofrequency ablation (RFA), have been introduced to prolong stent patency and survival. Currently, RFA is commonly used as palliative therapy, even for advanced MHO. This literature review summarizes recent studies on RFA for advanced MHO.
Keyword
Figure
Reference
-
1. Shin HR, Oh JK, Masuyer E, et al. Epidemiology of cholangiocarcinoma: an update focusing on risk factors. Cancer Sci. 2010; 101:579–585.2. Blechacz B, Komuta M, Roskams T, et al. Clinical diagnosis and staging of cholangiocarcinoma. Nat Rev Gastroenterol Hepatol. 2011; 8:512–522.3. Deoliveira ML, Schulick RD, Nimura Y, et al. New staging system and a registry for perihilar cholangiocarcinoma. Hepatology. 2011; 53:1363–1371.4. Yusoff AR, Siti ZM, Muzammil AR, et al. Cholangiocarcinoma: a 10-year experience of a single tertiary centre in the multi ethnicity-Malaysia. Med J Malaysia. 2012; 67:45–51.5. Rerknimitr R, Angsuwatcharakon P, Ratanachu-ek T, et al. Asia-Pacific consensus recommendations for endoscopic and interventional management of hilar cholangiocarcinoma. J Gastroenterol Hepatol. 2013; 28:593–607.6. Rizvi S, Khan SA, Hallemeier CL, et al. Cholangiocarcinoma: evolving concepts and therapeutic strategies. Nat Rev Clin Oncol. 2018; 15:95–111.7. Sharaiha RZ, Natov N, Glockenberg KS, et al. Comparison of metal stenting with radiofrequency ablation versus stenting alone for treating malignant biliary strictures: is there an added benefit? Dig Dis Sci. 2014; 59:3099–3102.8. Yang J, Wang J, Zhou H, et al. Efficacy and safety of endoscopic radiofrequency ablation for unresectable extrahepatic cholangiocarcinoma: a randomized trial. Endoscopy. 2018; 50:751–760.9. Hong MJ, Cheon YK, Lee EJ, et al. Long-term outcome of photodynamic therapy with systemic chemotherapy compared to photodynamic therapy alone in patients with advanced hilar cholangiocarcinoma. Gut Liver. 2014; 8:318–323.10. Han SY, Kim DU, Kang DH, et al. Usefulness of intraductal RFA in patients with malignant biliary obstruction. Medicine (Baltimore). 2020; 99:e21724.11. Mohammad T, Kahaleh M. Comparing palliative treatment options for cholangiocarcinoma: photodynamic therapy vs. radiofrequency ablation. Clin Endosc. 2022; 55:347–354.12. Aghaie Meybodi M, Shakoor D, Nanavati J, et al. Unilateral versus bilateral endoscopic stenting in patients with unresectable malignant hilar obstruction: a systematic review and meta-analysis. Endosc Int Open. 2020; 8:E281–E290.13. Vienne A, Hobeika E, Gouya H, et al. Prediction of drainage effectiveness during endoscopic stenting of malignant hilar strictures: the role of liver volume assessment. Gastrointest Endosc. 2010; 72:728–735.14. Qumseya BJ, Jamil LH, Elmunzer BJ, et al. ASGE guideline on the role of endoscopy in the management of malignant hilar obstruction. Gastrointest Endosc. 2021; 94:222–234.15. Takenaka M, Kudo M. Endoscopic reintervention for recurrence of malignant biliary obstruction: developing the best strategy. Gut Liver. 2022; 16:525–534.16. Nakai Y, Kogure H, Isayama H, et al. Endoscopic ultrasound-guided biliary drainage for unresectable hilar malignant biliary obstruction. Clin Endosc. 2019; 52:220–225.17. Kongkam P, Orprayoon T, Boonmee C, et al. ERCP plus endoscopic ultrasound-guided biliary drainage versus percutaneous transhepatic biliary drainage for malignant hilar biliary obstruction: a multicenter observational open-label study. Endoscopy. 2021; 53:55–62.18. Takenaka M, Hosono M, Rehani MM, et al. Comparison of radiation exposure between endoscopic ultrasound-guided drainage and transpapillary drainage by endoscopic retrograde cholangiopancreatography for pancreatobiliary diseases. Dig Endosc. 2022; 34:579–586.19. Lee TH, Moon JH, Stuart S. Role of ERCP in malignant hilar biliary obstruction. Gastrointest Endosc Clin N Am. 2022; 32:427–453.20. Kim JH. Endoscopic stent placement in the palliation of malignant biliary obstruction. Clin Endosc. 2011; 44:76–86.21. Lee TH. Technical tips and issues of biliary stenting, focusing on malignant hilar obstruction. Clin Endosc. 2013; 46:260–266.22. Lee TH, Lee SJ, Moon JH, et al. Technical tips and issues of biliary stenting, focusing on malignant hilar obstruction. Minerva Gastroenterol Dietol. 2014; 60:135–149.23. Kawakami H, Itoi T, Kuwatani M, et al. Technical tips and troubleshooting of endoscopic biliary drainage for unresectable malignant hilar biliary obstruction. J Hepatobiliary Pancreat Sci. 2015; 22:E12–E21.24. Liberato MJ, Canena JM. Endoscopic stenting for hilar cholangiocarcinoma: efficacy of unilateral and bilateral placement of plastic and metal stents in a retrospective review of 480 patients. BMC Gastroenterol. 2012; 12:103.25. Mukai T, Yasuda I, Nakashima M, et al. Metallic stents are more efficacious than plastic stents in unresectable malignant hilar biliary strictures: a randomized controlled trial. J Hepatobiliary Pancreat Sci. 2013; 20:214–222.26. Aljiffry M, Abdulelah A, Walsh M, et al. Evidence-based approach to cholangiocarcinoma: a systematic review of the current literature. J Am Coll Surg. 2009; 208:134–147.27. Sangchan A, Kongkasame W, Pugkhem A, et al. Efficacy of metal and plastic stents in unresectable complex hilar cholangiocarcinoma: a randomized controlled trial. Gastrointest Endosc. 2012; 76:93–99.28. Dumonceau JM, Tringali A, Papanikolaou IS, et al. Endoscopic biliary stenting: indications, choice of stents, and results: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline: updated October 2017. Endoscopy. 2018; 50:910–930.29. Cho JH, Lee KH, Kim JM, et al. Safety and effectiveness of endobiliary radiofrequency ablation according to the different power and target temperature in a swine model. J Gastroenterol Hepatol. 2017; 32:521–526.30. Rustagi T, Jamidar PA. Intraductal radiofrequency ablation for management of malignant biliary obstruction. Dig Dis Sci. 2014; 59:2635–2641.31. Larghi A, Rimbaș M, Tringali A, et al. Endoscopic radiofrequency biliary ablation treatment: a comprehensive review. Dig Endosc. 2019; 31:245–255.32. Itoi T, Isayama H, Sofuni A, et al. Evaluation of effects of a novel endoscopically applied radiofrequency ablation biliary catheter using an ex-vivo pig liver. J Hepatobiliary Pancreat Sci. 2012; 19:543–547.33. Zacharoulis D, Lazoura O, Sioka E, et al. Habib EndoHPB: a novel endobiliary radiofrequency ablation device: an experimental study. J Invest Surg. 2013; 26:6–10.34. Kang H, Han SY, Cho JH, et al. Efficacy and safety of temperature-controlled intraductal radiofrequency ablation in advanced malignant hilar biliary obstruction: a pilot multicenter randomized comparative trial. J Hepatobiliary Pancreat Sci. 2022; 29:469–478.35. Wadsworth CA, Westaby D, Khan SA. Endoscopic radiofrequency ablation for cholangiocarcinoma. Curr Opin Gastroenterol. 2013; 29:305–311.36. Ortner ME, Caca K, Berr F, et al. Successful photodynamic therapy for nonresectable cholangiocarcinoma: a randomized prospective study. Gastroenterology. 2003; 125:1355–1363.37. Zoepf T, Jakobs R, Arnold JC, et al. Palliation of nonresectable bile duct cancer: improved survival after photodynamic therapy. Am J Gastroenterol. 2005; 100:2426–2430.38. Gerhardt T, Rings D, Höblinger A, et al. Combination of bilateral metal stenting and trans-stent photodynamic therapy for palliative treatment of hilar cholangiocarcinoma. Z Gastroenterol. 2010; 48:28–32.39. Cheon YK, Lee TY, Lee SM, et al. Longterm outcome of photodynamic therapy compared with biliary stenting alone in patients with advanced hilar cholangiocarcinoma. HPB (Oxford). 2012; 14:185–193.40. Mohan BP, Chandan S, Khan SR, et al. Photodynamic therapy (PDT), radiofrequency ablation (RFA) with biliary stents in palliative treatment of unresectable extrahepatic cholangiocarcinoma: a systematic review and meta-analysis. J Clin Gastroenterol. 2022; 56:e153–e160.41. Schmidt A, Bloechinger M, Weber A, et al. Short-term effects and adverse events of endoscopically applied radiofrequency ablation appear to be comparable with photodynamic therapy in hilar cholangiocarcinoma. United European Gastroenterol J. 2016; 4:570–579.42. Inoue T, Ibusuki M, Kitano R, et al. Endobiliary radiofrequency ablation combined with bilateral metal stent placement for malignant hilar biliary obstruction. Endoscopy. 2020; 52:595–599.43. Bokemeyer A, Matern P, Bettenworth D, et al. Endoscopic radiofrequency ablation prolongs survival of patients with unresectable hilar cholangiocellular carcinoma: a case-control study. Sci Rep. 2019; 9:13685.44. Tal AO, Vermehren J, Friedrich-Rust M, et al. Intraductal endoscopic radiofrequency ablation for the treatment of hilar non-resectable malignant bile duct obstruction. World J Gastrointest Endosc. 2014; 6:13–19.45. Kim EJ, Cho JH, Kim YJ, et al. Intraductal temperature-controlled radiofrequency ablation in malignant hilar obstruction: a preliminary study in animals and initial human experience. Endosc Int Open. 2019; 7:E1293–E1300.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intraductal Radiofrequency Ablation as a Palliative Treatment for Advanced Malignant Hilar Biliary Obstruction
- Safety and Efficacy of Percutaneous Intraductal Radiofrequency Ablation Followed by Dual Stent Placement for Malignant Biliary Hilar Obstruction
- Efficacy of Endobiliary Radiofrequency Ablation for Malignant Biliary Obstruction
- Bilateral Metallic Stenting in Malignant Hilar Obstruction
- Endoscopic Stent Placement in the Palliation of Malignant Biliary Obstruction