Metabolic Dysfunction-Associated Fatty Liver Disease and Mortality: A Population-Based Cohort Study
- Affiliations
-
- 1Department of Internal Medicine, CHA Bundang Medical Center, CHA University School of Medicine, Seongnam, Korea
- 2Department of Internal Medicine, Hanyang University Guri Hospital, Hanyang University College of Medicine, Guri, Korea
- 3Department of Statistics, Dongguk University, Seoul, Korea
- 4Department of Internal Medicine, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2540519
- DOI: http://doi.org/10.4093/dmj.2021.0327
Abstract
- Background
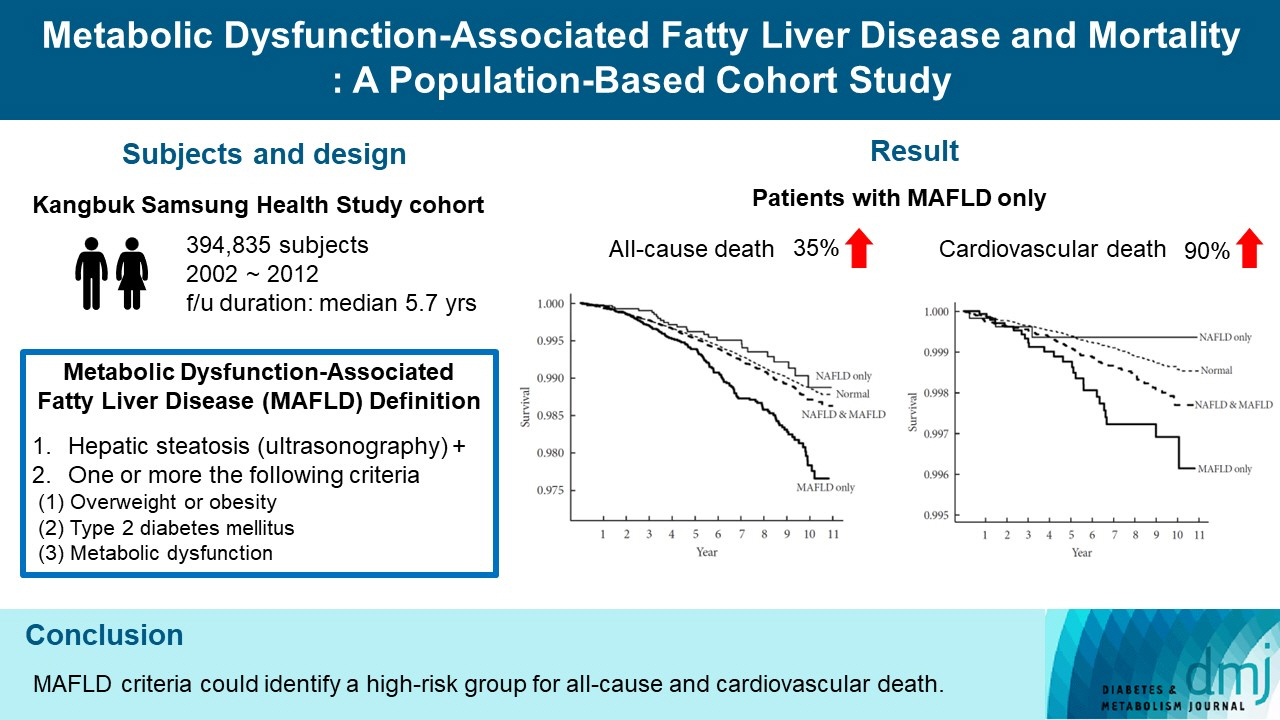
We investigated whether metabolic dysfunction-associated fatty liver disease (MAFLD) is associated with an elevated risk of all-cause and cardiovascular mortality using a large-scale health examination cohort.
Methods
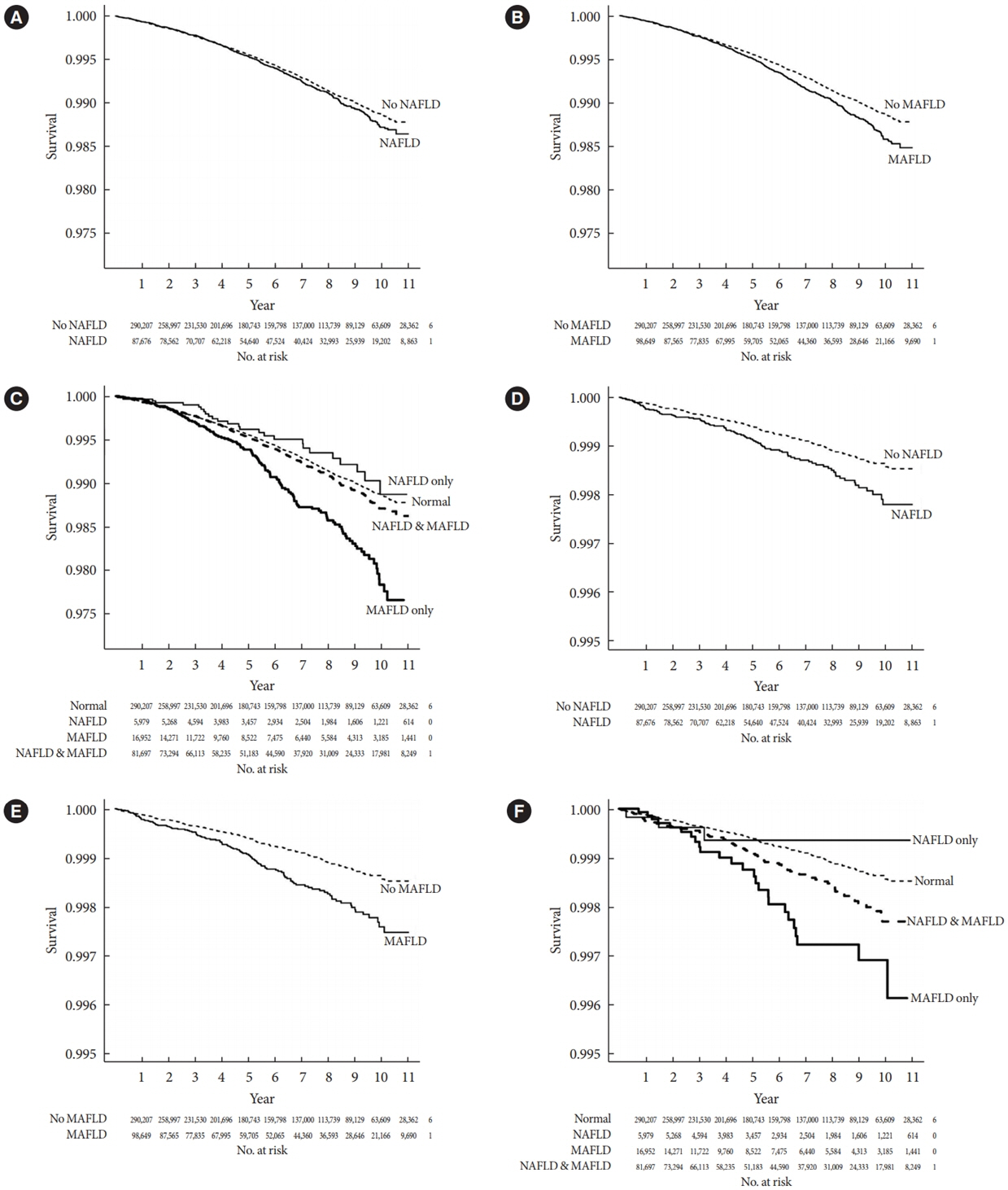
A total of 394,835 subjects in the Kangbuk Samsung Health Study cohort were enrolled from 2002 to 2012. Participants were categorized by the presence of nonalcoholic fatty liver disease (NAFLD) and MAFLD as follows: normal subjects; patients with both NAFLD and MAFLD; patients with NAFLD only; and patients with MAFLD only. Cox proportional hazards models were used to analyze the risk of mortality.
Results
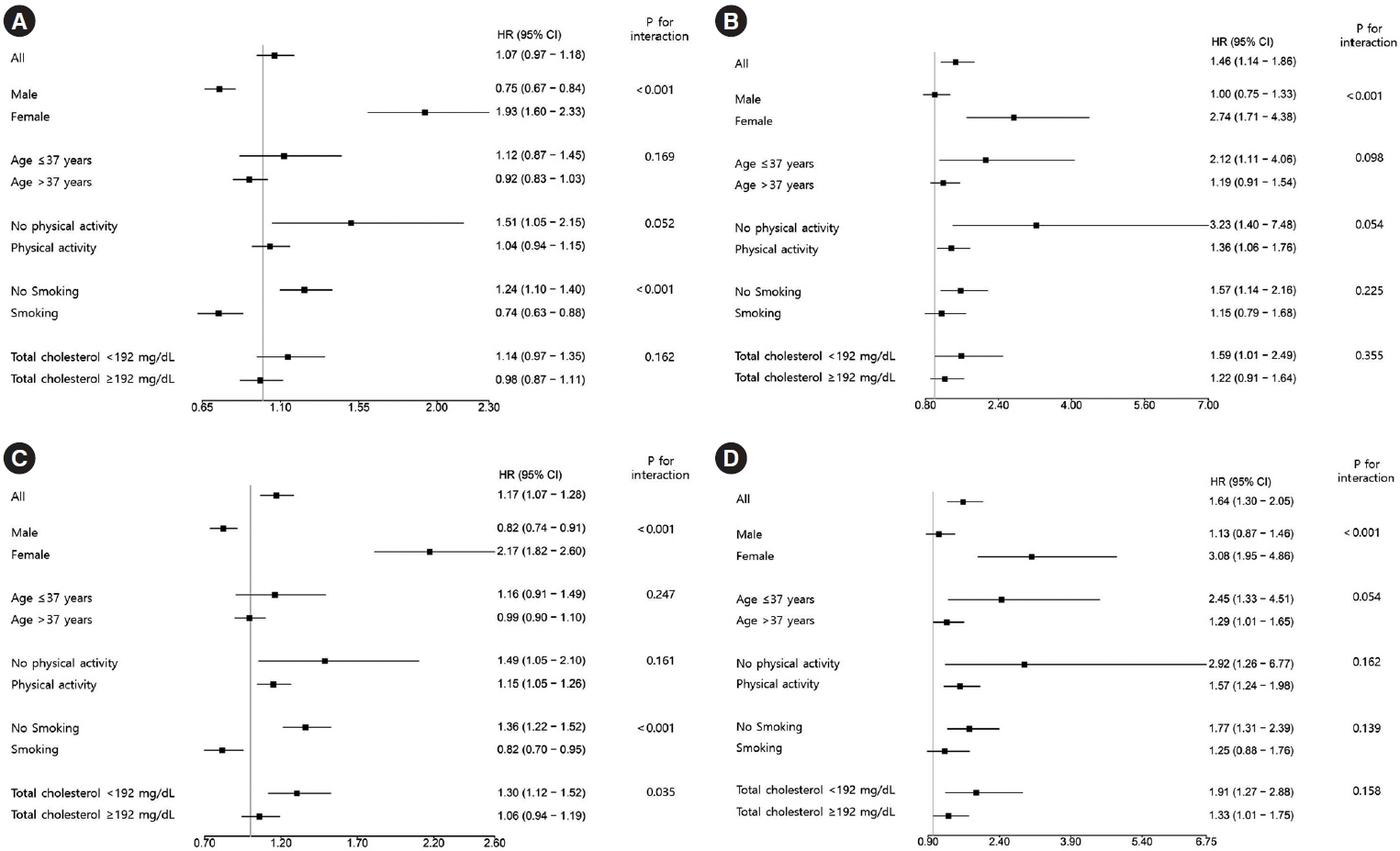
During a median 5.7 years of follow-up, 20.69% was patients with both NAFLD and MAFLD, 1.51% was patients with NAFLD only, and 4.29% was patients with MAFLD only. All-cause and cardiovascular death was higher in patients with MAFLD than those without MAFLD (P<0.001, respectively). In patients with MAFLD only, the hazard ratio (HR) of all-cause and cardiovascular death was 1.35 (95% confidence interval [CI], 1.13 to 1.60) and 1.90 (95% CI, 1.26 to 2.88) after adjusting for age, which lost its statistical significance by multivariable adjustments. Compared to patients with less than two components of metabolic dysfunction, patients with more than two components of metabolic dysfunction were a higher risk of cardiovascular death (HR, 2.05; 95% CI, 1.25 to 3.38) and only women with more than two components of metabolic dysfunction were a higher risk of all-cause death (HR, 1.44; 95% CI, 1.02 to 2.03).
Conclusion
MAFLD criteria could identify a high-risk group for all-cause and cardiovascular death.
Figure
Cited by 2 articles
-
Metabolic Dysfunction-Associated Steatotic Liver Disease in Type 2 Diabetes Mellitus: A Review and Position Statement of the Fatty Liver Research Group of the Korean Diabetes Association
Jaehyun Bae, Eugene Han, Hye Won Lee, Cheol-Young Park, Choon Hee Chung, Dae Ho Lee, Eun-Hee Cho, Eun-Jung Rhee, Ji Hee Yu, Ji Hyun Park, Ji-Cheol Bae, Jung Hwan Park, Kyung Mook Choi, Kyung-Soo Kim, Mi Hae Seo, Minyoung Lee, Nan-Hee Kim, So Hun Kim, Won-Young Lee, Woo Je Lee, Yeon-Kyung Choi, Yong-ho Lee, You-Cheol Hwang, Young Sang Lyu, Byung-Wan Lee, Bong-Soo Cha
Diabetes Metab J. 2024;48(6):1015-1028. doi: 10.4093/dmj.2024.0541.Extracellular Vesicle-Mediated Network in the Pathogenesis of Obesity, Diabetes, Steatotic Liver Disease, and Cardiovascular Disease
Joonyub Lee, Won Gun Choi, Marie Rhee, Seung-Hwan Lee
Diabetes Metab J. 2025;49(3):348-367. doi: 10.4093/dmj.2025.0184.
Reference
-
1. Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease: meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016; 64:73–84.2. Lee YH, Cho Y, Lee BW, Park CY, Lee DH, Cha BS, et al. Non-alcoholic fatty liver disease in diabetes. Part I: epidemiology and diagnosis. Diabetes Metab J. 2019; 43:31–45.3. Rhee EJ. Nonalcoholic fatty liver disease and diabetes: an epidemiological perspective. Endocrinol Metab (Seoul). 2019; 34:226–33.4. Targher G, Byrne CD, Lonardo A, Zoppini G, Barbui C. Nonalcoholic fatty liver disease and risk of incident cardiovascular disease: a meta-analysis. J Hepatol. 2016; 65:589–600.5. Anstee QM, Mantovani A, Tilg H, Targher G. Risk of cardiomyopathy and cardiac arrhythmias in patients with nonalcoholic fatty liver disease. Nat Rev Gastroenterol Hepatol. 2018; 15:425–39.6. Han JM, Kim HI, Lee YJ, Lee JW, Kim KM, Bae JC. Differing associations between fatty liver and dyslipidemia according to the degree of hepatic steatosis in Korea. J Lipid Atheroscler. 2019; 8:258–66.7. Chung GE, Kim MJ, Yim JY, Kim JS, Yoon JW. Sarcopenia is significantly associated with presence and severity of nonalcoholic fatty liver disease. J Obes Metab Syndr. 2019; 28:129–38.8. Li F, Ye J, Sun Y, Lin Y, Wu T, Shao C, et al. Distinct dose-dependent association of free fatty acids with diabetes development in nonalcoholic fatty liver disease patients. Diabetes Metab J. 2021; 45:417–29.9. Kim KS, Lee BW, Kim YJ, Lee DH, Cha BS, Park CY. Nonalcoholic fatty liver disease and diabetes. Part II: treatment. Diabetes Metab J. 2019; 43:127–43.10. Lee H, Kim G, Choi YJ, Huh BW, Lee BW, Kang ES, et al. Association between non-alcoholic steatohepatitis and left ventricular diastolic dysfunction in type 2 diabetes mellitus. Diabetes Metab J. 2020; 44:267–76.11. Lee YH, Kim KJ, Yoo ME, Kim G, Yoon HJ, Jo K, et al. Association of non-alcoholic steatohepatitis with subclinical myocardial dysfunction in non-cirrhotic patients. J Hepatol. 2018; 68:764–72.12. Lin S, Huang J, Wang M, Kumar R, Liu Y, Liu S, et al. Comparison of MAFLD and NAFLD diagnostic criteria in real world. Liver Int. 2020; 40:2082–9.13. Eslam M, Newsome PN, Sarin SK, Anstee QM, Targher G, Romero-Gomez M, et al. A new definition for metabolic dysfunction-associated fatty liver disease: an international expert consensus statement. J Hepatol. 2020; 73:202–9.14. Eslam M, Sanyal AJ, George J; International Consensus Panel. MAFLD: a consensus-driven proposed nomenclature for metabolic associated fatty liver disease. Gastroenterology. 2020; 158:1999–2014.15. Eslam M, Sarin SK, Wong VW, Fan JG, Kawaguchi T, Ahn SH, et al. The Asian Pacific Association for the Study of the Liver clinical practice guidelines for the diagnosis and management of metabolic associated fatty liver disease. Hepatol Int. 2020; 14:889–919.16. Kim D, Konyn P, Sandhu KK, Dennis BB, Cheung AC, Ahmed A. Metabolic dysfunction-associated fatty liver disease is associated with increased all-cause mortality in the United States. J Hepatol. 2021; 75:1284–91.17. Wang X, Wu S, Yuan X, Chen S, Fu Q, Sun Y, et al. Metabolic dysfunction-associated fatty liver disease and mortality among Chinese adults: a prospective cohort study. J Clin Endocrinol Metab. 2022; 107:e745–55.18. Angulo P, Kleiner DE, Dam-Larsen S, Adams LA, Bjornsson ES, Charatcharoenwitthaya P, et al. Liver fibrosis, but no other histologic features, is associated with long-term outcomes of patients with nonalcoholic fatty liver disease. Gastroenterology. 2015; 149:389–97.19. Ekstedt M, Hagstrom H, Nasr P, Fredrikson M, Stal P, Kechagias S, et al. Fibrosis stage is the strongest predictor for disease-specific mortality in NAFLD after up to 33 years of follow-up. Hepatology. 2015; 61:1547–54.20. Hwang YC, Ahn HY, Park SW, Park CY. Nonalcoholic fatty liver disease associates with increased overall mortality and death from cancer, cardiovascular disease, and liver disease in women but not men. Clin Gastroenterol Hepatol. 2018; 16:1131–7.21. Lee H, Lee YH, Kim SU, Kim HC. Metabolic dysfunction-associated fatty liver disease and incident cardiovascular disease risk: a nationwide cohort study. Clin Gastroenterol Hepatol. 2021; 19:2138–47.22. Yamamura S, Eslam M, Kawaguchi T, Tsutsumi T, Nakano D, Yoshinaga S, et al. MAFLD identifies patients with significant hepatic fibrosis better than NAFLD. Liver Int. 2020; 40:3018–30.23. Chiang DJ, McCullough AJ. The impact of obesity and metabolic syndrome on alcoholic liver disease. Clin Liver Dis. 2014; 18:157–63.24. Choi HS, Brouwer WP, Zanjir WM, de Man RA, Feld JJ, Hansen BE, et al. Nonalcoholic steatohepatitis is associated with liver-related outcomes and all-cause mortality in chronic hepatitis B. Hepatology. 2020; 71:539–48.25. Nguyen VH, Le MH, Cheung RC, Nguyen MH. Differential clinical characteristics and mortality outcomes in persons with NAFLD and/or MAFLD. Clin Gastroenterol Hepatol. 2021; 19:2172–81.26. Jeong SW. Nonalcoholic fatty liver disease: a drug revolution is coming. Diabetes Metab J. 2020; 44:640–57.27. Lee DH. Noninvasive evaluation of nonalcoholic fatty liver disease. Endocrinol Metab (Seoul). 2020; 35:243–59.28. Lonardo A, Nascimbeni F, Ballestri S, Fairweather D, Win S, Than TA, et al. Sex differences in nonalcoholic fatty liver disease: state of the art and identification of research gaps. Hepatology. 2019; 70:1457–69.29. Maas AH, Rosano G, Cifkova R, Chieffo A, van Dijken D, Hamoda H, et al. Cardiovascular health after menopause transition, pregnancy disorders, and other gynaecologic conditions: a consensus document from European cardiologists, gynaecologists, and endocrinologists. Eur Heart J. 2021; 42:967–84.30. Eslam M, Sanyal AJ, George J. Toward more accurate nomenclature for fatty liver diseases. Gastroenterology. 2019; 157:590–3.31. Jung CH, Rhee EJ, Kwon H, Chang Y, Ryu S, Lee WY. Visceral-to-subcutaneous abdominal fat ratio is associated with nonalcoholic fatty liver disease and liver fibrosis. Endocrinol Metab (Seoul). 2020; 35:165–76.32. Lee SB, Kim MK, Kang S, Park K, Kim JH, Baik SJ, et al. Triglyceride glucose index is superior to the homeostasis model assessment of insulin resistance for predicting nonalcoholic fatty liver disease in Korean adults. Endocrinol Metab (Seoul). 2019; 34:179–86.33. Byrne CD, Targher G. NAFLD: a multisystem disease. J Hepatol. 2015; 62(1 Suppl):S47–64.34. Vilar-Gomez E, Calzadilla-Bertot L, Wai-Sun Wong V, Castellanos M, Aller-de la Fuente R, Metwally M, et al. Fibrosis severity as a determinant of cause-specific mortality in patients with advanced nonalcoholic fatty liver disease: a multi-national cohort study. Gastroenterology. 2018; 155:443–57.35. Pelusi S, Cespiati A, Rametta R, Pennisi G, Mannisto V, Rosso C, et al. Prevalence and risk factors of significant fibrosis in patients with nonalcoholic fatty liver without steatohepatitis. Clin Gastroenterol Hepatol. 2019; 17:2310–9.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The crosstalk between insulin resistance and nonalcoholic fatty liver disease/metabolic dysfunction-associated fatty liver disease: a culprit or a consequence?
- Metabolic dysfunction-associated fatty liver disease is a ubiquitous latent cofactor in viral- and alcoholic-related hepatocellular carcinoma: Editorial on “Global prevalence of metabolic dysfunction-associated fatty liver disease-related hepatocellular carcinoma: A systematic review and meta-analysis”
- Metabolic-associated fatty liver disease is less effective in predicting mortality than non-alcoholic fatty liver disease and metabolic dysfunction-associated steatotic liver disease: Letter to the editor on “Prognosis of biopsy-confirmed metabolic dysfunction-associated steatotic liver disease: A sub-analysis of the CLIONE study”
- Metabolic Dysfunction-Associated Fatty Liver Disease Predicts Long-term Mortality and Cardiovascular Disease
- The new definition of metabolic dysfunction-associated steatotic liver disease: the role of ultrasound and elastography