Acute Crit Care.
2023 Feb;38(1):122-133. 10.4266/acc.2022.00584.
Alcohol use disorder in the intensive care unit a highly morbid condition, but chemical dependency discussion improves outcomes
- Affiliations
-
- 1Department of Trauma Surgery, Saint Mary’s Medical Center-Essentia Health, Duluth, MN, USA
- 2University of Minnesota Medical School, Minneapolis MN, USA
- 3Essentia Institute of Rural Health, Duluth, MN, USA
- KMID: 2540322
- DOI: http://doi.org/10.4266/acc.2022.00584
Abstract
- Background
Alcohol use disorders (AUD) are common in patients admitted to intensive care units (ICU) and increase the risk for worse outcomes. In this study, we describe factors associated with patient mortality after ICU admission and the effect of chemical dependency (CD) counseling on outcomes in the year following ICU admission.
Methods
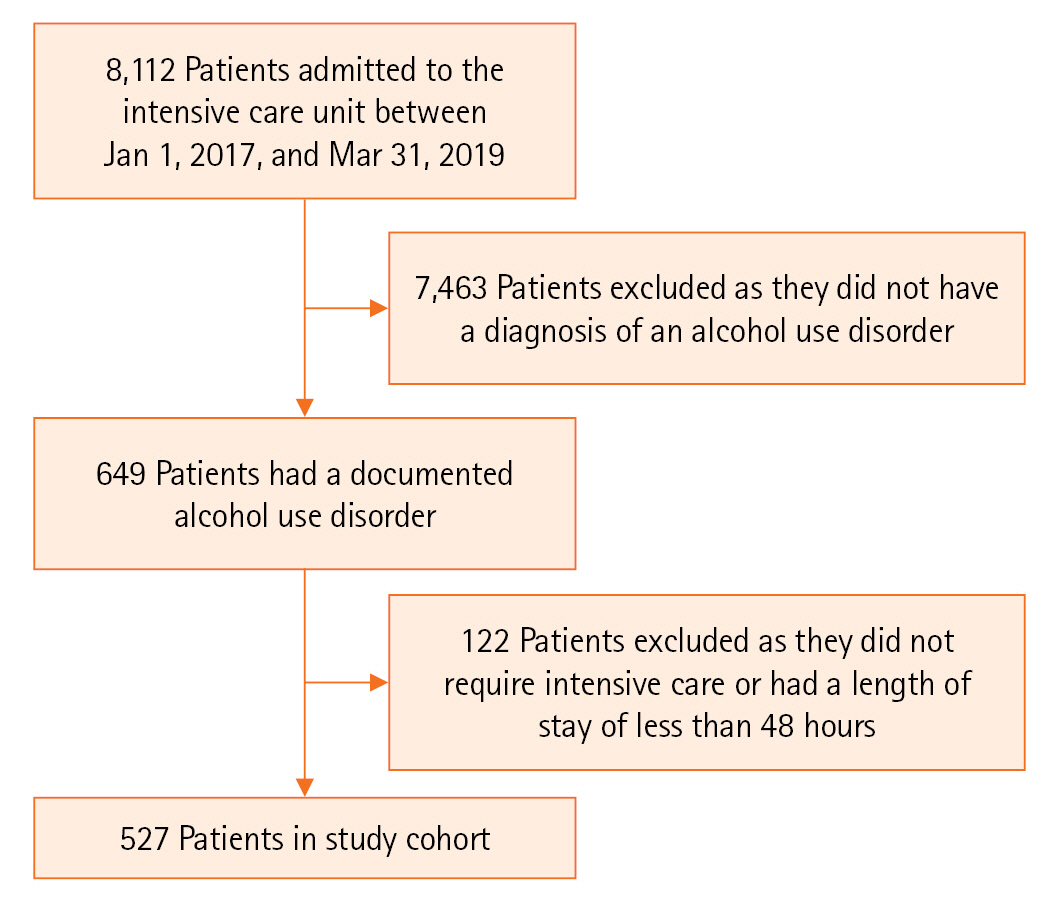
We retrospectively reviewed patient demographics, hospital data, and documentation of CD counseling by medical providers for all ICU patients with AUD admitted to our institution between January 2017 and March 2019. Primary outcomes were in-hospital and 1-year mortality.
Results
Of the 527 patients with AUD requiring ICU care, median age was 56 years (range, 18–86 years). Both in-hospital mortality (12%) and 1-year mortality rates (27%) were high. . Rural patients, comorbidities, older age, need for mechanical ventilation, and complications were associated with increased risk of in-hospital and 1-year mortality. CD counseling was documented for 73% of patients, and 50% of these patients accepted alcohol treatment or resources prior to discharge. CD evaluation and acceptance was associated with a significantly decreased rate of readmission for liver or alcohol-related issues (36% vs. 58%; odds ratio [OR], 0.41; 95% confidence intervals [CI], 0.27–0.61) and 1-year mortality (7% vs. 19.5%; OR, 0.32; 95% CI, 0.16–0.64). CD evaluation alone, regardless of patient acceptance, was associated with a significantly decreased 1-year post-discharge mortality rate (12% vs. 23%; OR, 0.44; 95% CI, 0.25–0.77.)
Conclusions
ICU patients with AUD had high in-hospital and 1-year mortality. CD evaluation, regardless of patient acceptance, was associated with a significant decrease in 1-year mortality.
Figure
Reference
-
1. Substance Abuse and Mental Health Services Administration. Key substance use and mental health indicators in the United States: results from the 2020 national survey on drug use and health. Substance Abuse and Mental Health Services Administration;2020.2. Rehm J, Gmel GE Sr, Gmel G, Hasan OS, Imtiaz S, Popova S, et al. The relationship between different dimensions of alcohol use and the burden of disease-an update. Addiction. 2017; 112:968–1001.
Article3. Esser MB, Sherk A, Liu Y, Naimi TS, Stockwell T, Stahre M, et al. Deaths and years of potential life lost from excessive alcohol use: United States, 2011-2015. MMWR Morb Mortal Wkly Rep. 2020; 69:1428–33.4. National Institute on Alcohol Abuse and Alcoholism (NIAAA). Alcohol facts and statistics [Internet]. NIAAA;2019. [cited 2022 Feb 18]. Available from: https://www.niaaa.nih.gov/publications/brochures-and-fact-sheets/alcohol-facts-and-statistics.5. Bouchery EE, Harwood HJ, Sacks JJ, Simon CJ, Brewer RD. Economic costs of excessive alcohol consumption in the U.S., 2006. Am J Prev Med. 2011; 41:516–24.
Article6. Longabaugh R, Woolard RE, Nirenberg TD, Minugh AP, Becker B, Clifford PR, et al. Evaluating the effects of a brief motivational intervention for injured drinkers in the emergency department. J Stud Alcohol. 2001; 62:806–16.
Article7. Cordovilla-Guardia S, Fernández-Mondéjar E, Vilar-López R, Navas JF, Portillo-Santamaría M, Rico-Martín S, et al. Effect of a brief intervention for alcohol and illicit drug use on trauma recidivism in a cohort of trauma patients. PLoS One. 2017; 12:e0182441.
Article8. Clark BJ, Moss M. Secondary prevention in the intensive care unit: does intensive care unit admission represent a “teachable moment?”. Crit Care Med. 2011; 39:1500–6.
Article9. Uusaro A, Parviainen I, Tenhunen JJ, Ruokonen E. The proportion of intensive care unit admissions related to alcohol use: a prospective cohort study. Acta Anaesthesiol Scand. 2005; 49:1236–40.
Article10. O’Brien JM Jr, Lu B, Ali NA, Martin GS, Aberegg SK, Marsh CB, et al. Alcohol dependence is independently associated with sepsis, septic shock, and hospital mortality among adult intensive care unit patients. Crit Care Med. 2007; 35:345–50.
Article11. McKenny M, O’Beirne S, Fagan C, O’Connell M. Alcohol-related admissions to an intensive care unit in Dublin. Ir J Med Sci. 2010; 179:405–8.
Article12. Geary T, O’Brien P, Ramsay S, Cook B; Scottish Intensive Care Trainees’ Audit Share Group. A national service evaluation of the impact of alcohol on admissions to Scottish intensive care units. Anaesthesia. 2012; 67:1132–7.
Article13. Gacouin A, Tadie JM, Uhel F, Sauvadet E, Fillâtre P, Letheulle J, et al. At-risk drinking is independently associated with ICU and one-year mortality in critically ill nontrauma patients. Crit Care Med. 2014; 42:860–7.
Article14. Lynch C, Pugh R, Battle C; Welsh Intensive Care Society Audit and Research Group (WICSARG). A multicentre prospective evaluation of alcohol-related admissions to intensive care units in Wales. J Intensive Care Soc. 2017; 18:193–7.
Article15. McPeake JM, Shaw M, O’Neill A, Forrest E, Puxty A, Quasim T, et al. Do alcohol use disorders impact on long term outcomes from intensive care? Crit Care. 2015; 19:185.
Article16. Trainor D, Martin L, Lavery G. Alcohol misuse requiring admission to a tertiary referral ICU: resource implications. Crit Care. 2009; 13:1–2.
Article17. Christensen S, Johansen MB, Pedersen L, Jensen R, Larsen KM, Larsson A, et al. Three-year mortality among alcoholic patients after intensive care: a population-based cohort study. Crit Care. 2012; 16:R5.
Article18. Mackle IJ, Swann DG, Cook B. One year outcome of intensive care patients with decompensated alcoholic liver disease. Br J Anaesth. 2006; 97:496–8.
Article19. Heydtmann M, McDonald SA. Survival and re-admission of patients admitted with alcoholic liver disease to a West of Scotland hospital. Scott Med J. 2013; 58:134–8.
Article20. Kavli M, Strøm T, Carlsson M, Dahler-Eriksen B, Toft P. The outcome of critical illness in decompensated alcoholic liver cirrhosis. Acta Anaesthesiol Scand. 2012; 56:987–94.
Article21. Aggarwal A, Ong JP, Younossi ZM, Nelson DR, Hoffman-Hogg L, Arroliga AC. Predictors of mortality and resource utilization in cirrhotic patients admitted to the medical ICU. Chest. 2001; 119:1489–97.
Article22. Goldfarb G, Nouel O, Poynard T, Rueff B. Efficiency of respiratory assistance in cirrhotic patients with liver failure. Intensive Care Med. 1983; 9:271–3.
Article23. Levesque E, Saliba F, Ichaï P, Samuel D. Outcome of patients with cirrhosis requiring mechanical ventilation in ICU. J Hepatol. 2014; 60:570–8.
Article24. Baudry T, Hernu R, Valleix B, Jahandiez V, Faucher E, Simon M, et al. Cirrhotic patients admitted to the ICU with septic shock: factors predicting short and long-term outcome. Shock. 2019; 52:408–13.
Article25. Lai CC, Tseng KL, Ho CH, Chiang SR, Chan KS, Chao CM, et al. Outcome of liver cirrhosis patients requiring prolonged mechanical ventilation. Sci Rep. 2020; 10:4980.
Article26. McPhail MJ, Parrott F, Wendon JA, Harrison DA, Rowan KA, Bernal W. Incidence and outcomes for patients with cirrhosis admitted to the United Kingdom critical care units. Crit Care Med. 2018; 46:705–12.
Article27. Gildea TR, Cook WC, Nelson DR, Aggarwal A, Carey W, Younossi ZM, et al. Predictors of long-term mortality in patients with cirrhosis of the liver admitted to a medical ICU. Chest. 2004; 126:1598–603.
Article28. Huang YF, Lin CS, Cherng YG, Yeh CC, Chen RJ, Chen TL, et al. A population-based cohort study of mortality of intensive care unit patients with liver cirrhosis. BMC Gastroenterol. 2020; 20:15.
Article29. Patidar KR, Peng JL, Kaur H, Worden A, Kettler CD, Pike F, et al. Severe alcohol-associated hepatitis is associated with worse survival in critically ill patients with acute on chronic liver failure. Hepatol Commun. 2022; 6:1090–9.
Article30. Horvatits T, Drolz A, Trauner M, Fuhrmann V. Liver injury and failure in critical illness. Hepatology. 2019; 70:2204–15.
Article31. Albillos A, Lario M, Álvarez-Mon M. Cirrhosis-associated immune dysfunction: distinctive features and clinical relevance. J Hepatol. 2014; 61:1385–96.
Article32. Flores B, Trivedi HD, Robson SC, Bonder A. Hemostasis, bleeding and thrombosis in liver disease. J Transl Sci. 2017; 3:10.15761/JTS.1000182.
Article33. Boente RD, Sheikh A, Bosslet GT, Ghabril MS. Outcomes of acute respiratory distress syndrome in mechanically ventilated patients with cirrhosis. Crit Care Explor. 2019; 1:e0040.
Article34. Herrero R, Sánchez G, Asensio I, López E, Ferruelo A, Vaquero J, et al. Liver-lung interactions in acute respiratory distress syndrome. Intensive Care Med Exp. 2020; 8(Suppl 1):48.
Article35. Stirnimann J, Stirnimann G. Nutritional challenges in patients with advanced liver cirrhosis. J Clin Med. 2019; 8:1926.
Article36. Borders TF, Booth BM. Rural, suburban, and urban variations in alcohol consumption in the United States: findings from the National Epidemiologic Survey on Alcohol and Related Conditions. J Rural Health. 2007; 23:314–21.
Article37. Cervellione KL, Shah A, Patel MC, Curiel Duran L, Ullah T, Thurm C. Alcohol and drug abuse resource utilization in the ICU. Subst Abuse. 2019; 13:1178221819869327.
Article38. Clark BJ, Sorrell T, Hodapp RM, Reed K, Moss M, Aagaard L, et al. Pilot randomized trial of a recovery navigator program for survivors of critical illness with problematic alcohol use. Crit Care Explor. 2019; 1:e0051.
Article39. Schermer CR, Moyers TB, Miller WR, Bloomfield LA. Trauma center brief interventions for alcohol disorders decrease subsequent driving under the influence arrests. J Trauma. 2006; 60:29–34.
Article40. Clark BJ, Smart A, House R, Douglas I, Burnham EL, Moss M. Severity of acute illness is associated with baseline readiness to change in medical intensive care unit patients with unhealthy alcohol use. Alcohol Clin Exp Res. 2012; 36:544–51.
Article41. Harry ML, Lake E, Woehrle TA, Heger AM, Vogel LE. Implementing a screening and brief intervention protocol for excessive alcohol use in a trauma center: a healthcare improvement project. J Addict Nurs. 2022; 33:247–54.42. Tucker JA, Chandler SD, Witkiewitz K. Epidemiology of recovery from alcohol use disorder. Alcohol Res. 2020; 40:02.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Can the intensivists predict the outcomes of critically ill patients on the appropriateness of intensive care unit admission for limited intensive care unit resources ?
- Cardiac Complications in Patients Admitted to the Neuro-Intensive Care Unit
- Superficial Keratopathy of Patients in Intensive Care Unit
- Risk Factors for Cognitive Impairment in Intensive Care Unit Survivors
- Factors Influencing Intensive Care Unit Nurses’ Competency in Delirium Care in A Tertiary General Hospital