Acute Crit Care.
2023 Feb;38(1):8-20. 10.4266/acc.2022.01039.
Theoretical definition of nurse–conscious mechanically ventilated patient communication: a scoping review with qualitative content analysis
- Affiliations
-
- 1Department of Psychiatric Nursing and Management, School of Nursing and Midwifery, Shahid Beheshti University of Medical Sciences, Tehran, Iran
- 2Department of Community Health Nursing, School of Nursing and Midwifery, Shahid Beheshti University of Medical Sciences, Tehran, Iran
- 3Department of Psychiatric Nursing and Management, School of Nursing and Midwifery, Shahid Beheshti University of Medical Sciences, Tehran, Iran
- KMID: 2540310
- DOI: http://doi.org/10.4266/acc.2022.01039
Abstract
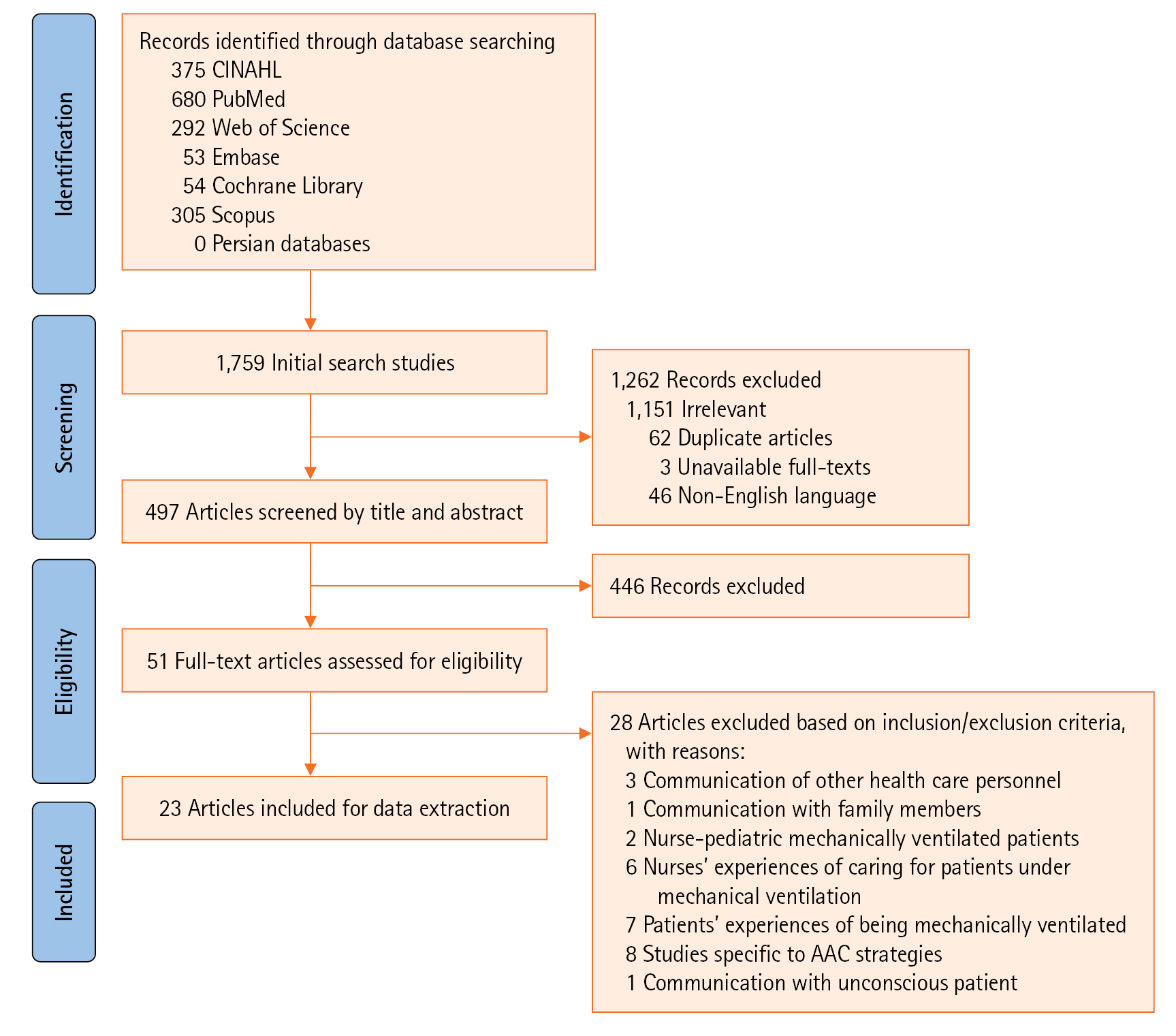
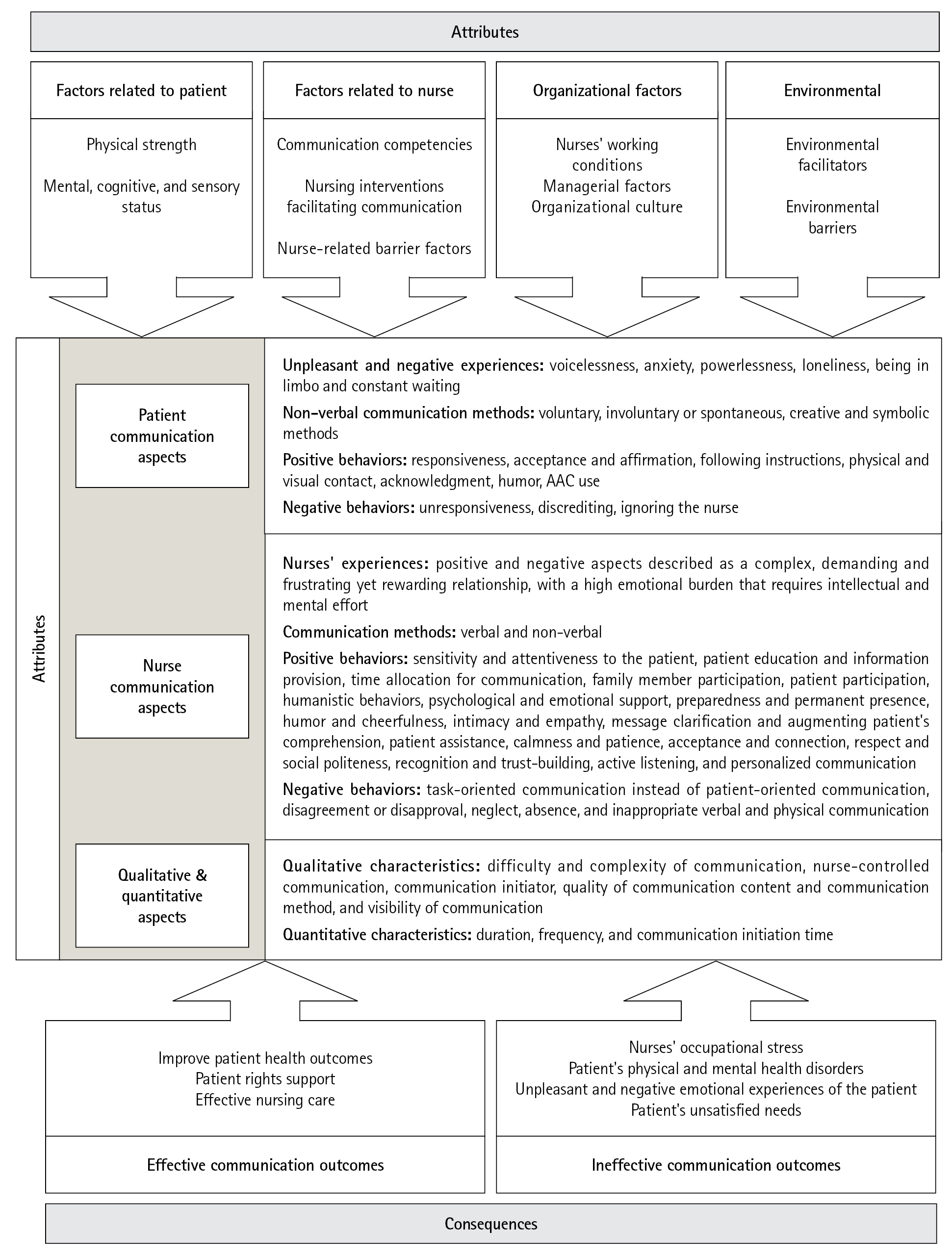
- Providing critical nursing care for conscious mechanically ventilated patients is mediated via effective communication. This study aimed to identify and map the antecedents, attributes, consequences, and definition of nurse–conscious mechanically ventilated patient communication (N-CMVPC). This scoping review was conducted by searching the Cochrane Library and the CINAHL, EMBASE, PubMed, Web of Science, and Scopus databases, between 2001 and 2021. The keywords queried included "nurses," "mechanically ventilated patients," "mechanical ventilation," "intubated patients," "communication," "interaction," "relationships," "nurse–patient communication," "nurse–patient relations," "intensive care units," and "critical care." Studies related to communication with healthcare personnel or family members were excluded. The results indicated that N-CMVPC manifests as a set of attributes in communication experiences, emotions, methods, and behaviors of the nurse and the patient and is classified into three main themes, nurse communication, patient communication, and quantitative-qualitative aspects. N-CMVPC is a complex, multidimensional, and multi-factor concept. It is often nurse-controlled and can express itself as questions, sentences, or commands in the context of experiences, feelings, and positive or negative behaviors involving the nurse and the patient.
Figure
Reference
-
1. He Q, Wang W, Zhu S, Wang M, Kang Y, Zhang R, et al. The epidemiology and clinical outcomes of ventilator-associated events among 20,769 mechanically ventilated patients at intensive care units: an observational study. Crit Care. 2021; 25:44.2. Namadian M, Taran Z. The effect of sedation protocol on sedation level and pharmacological and non-pharmacological interventions on mechanically ventilated patients. Iran J Nurs Midwifery Res. 2021; 26:316–23.3. Zisk-Rony RY, Weissman C, Weiss YG. Mechanical ventilation patterns and trends over 20 years in an Israeli hospital system: policy ramifications. Isr J Health Policy Res. 2019; 8:20.4. Karlsson V, Forsberg A, Bergbom I. Communication when patients are conscious during respirator treatment: a hermeneutic observation study. Intensive Crit Care Nurs. 2012; 28:197–207.5. Blackstone SW, Pressman H. Patient communication in health care settings: new opportunities for augmentative and alternative communication. Augment Altern Commun. 2016; 32:69–79.6. Dithole K, Sibanda S, Moleki MM, Thupayagale-Tshweneagae G. Exploring communication challenges between nurses and mechanically ventilated patients in the intensive care unit: a structured review. Worldviews Evid Based Nurs. 2016; 13:197–206.7. Foà C, Cavalli L, Maltoni A, Tosello N, Sangilles C, Maron I, et al. Communications and relationships between patient and nurse in intensive care unit: knowledge, knowledge of the work, knowledge of the emotional state. Acta Biomed. 2016; 87:71–82.8. Martinho CI, Rodrigues IT. Communication of mechanically ventilated patients in intensive care units. Rev Bras Ter Intensiva. 2016; 28:132–40.9. Carruthers H, Astin F, Munro W. Which alternative communication methods are effective for voiceless patients in intensive care units? A systematic review. Intensive Crit Care Nurs. 2017; 42:88–96.10. Burkhart LJ. What is AAC? [Internet]. International Society for Augmentative and Alternative Communication; 2018 [cited 2022 Dec 1]. Available from: https://www.isaac-online.org/english/what-is-AAC.11. Leung CC, Pun J, Lock G, Slade D, Gomersall CD, Wong WT, et al. Exploring the scope of communication content of mechanically ventilated patients. J Crit Care. 2018; 44:136–41.12. Holm A, Viftrup A, Karlsson V, Nikolajsen L, Dreyer P. Nurses' communication with mechanically ventilated patients in the intensive care unit: umbrella review. J Adv Nurs. 2020; 76:2909–20.13. Holm A, Dreyer P. Intensive care unit patients' experience of being conscious during endotracheal intubation and mechanical ventilation. Nurs Crit Care. 2017; 22:81–8.14. Dithole KS, Sibanda S, Moleki MM, Thupayagale-Tshweneagae G. Nurses' communication with patients who are mechanically ventilated in intensive care: the Botswana experience. Int Nurs Rev. 2016; 63:415–21.15. Happ MB. Giving voice: nurse-patient communication in the intensive care unit. Am J Crit Care. 2021; 30:256–65.16. Fleischer S, Berg A, Zimmermann M, Wüste K, Behrens J. Nurse-patient interaction and communication: A systematic literature review. J Pub Health. 2009; 17:339–53.17. Nilsen ML, Sereika SM, Hoffman LA, Barnato A, Donovan H, Happ MB. Nurse and patient interaction behaviors' effects on nursing care quality for mechanically ventilated older adults in the ICU. Res Gerontol Nurs. 2014; 7:113–25.18. Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005; 8:19–32.19. Peters MD, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc. 2015; 13:141–6.20. Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018; 169:467–73.21. Levac D, Colquhoun H, O'Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010; 5:69.22. Page MJ, Shamseer L, Tricco AC. Registration of systematic reviews in PROSPERO: 30,000 records and counting. Syst Rev. 2018; 7:32.23. Graneheim UH, Lindgren BM, Lundman B. Methodological challenges in qualitative content analysis: a discussion paper. Nurse Educ Today. 2017; 56:29–34.24. Tembo AC, Higgins I, Parker V. The experience of communication difficulties in critically ill patients in and beyond intensive care: findings from a larger phenomenological study. Intensive Crit Care Nurs. 2015; 31:171–8.25. Karlsen MW, Ølnes MA, Heyn LG. Communication with patients in intensive care units: a scoping review. Nurs Crit Care. 2019; 24:115–31.26. Wallander Karlsen MM, Heggdal K, Finset A, Heyn LG. Attention-seeking actions by patients on mechanical ventilation in intensive care units: a phenomenological-hermeneutical study. J Clin Nurs. 2019; 28:66–79.27. Happ MB, Garrett K, Thomas DD, Tate J, George E, Houze M, et al. Nurse-patient communication interactions in the intensive care unit. Am J Crit Care. 2011; 20:e28–40.28. Meriläinen M, Kyngäs H, Ala-Kokko T. Patients' interactions in an intensive care unit and their memories of intensive care: a mixed method study. Intensive Crit Care Nurs. 2013; 29:78–87.29. Salem A, Ahmad MM. Communication with invasive mechanically ventilated patients and the use of alternative devices: integrative review. J Res Nurs. 2018; 23:614–30.30. Bayog KM, Bello DM, Benabaye JM, Benegas TM, Benito AL, Berioso MA, et al. A conjoint analysis of the communication preferences of registered nurses towards mechanically ventilated patients. Int J Nurs Pract. 2020; 26:e12809.31. Momennasab M, Ardakani MS, Rad FD, Dokoohaki R, Dakhesh R, Jaberi A. Quality of nurses' communication with mechanically ventilated patients in a cardiac surgery intensive care unit. Invest Educ Enferm. 2019; 37:e02.32. Nilsen ML, Sereika S, Happ MB. Nurse and patient characteristics associated with duration of nurse talk during patient encounters in ICU. Heart Lung. 2013; 42:5–12.33. Khalaila R, Zbidat W, Anwar K, Bayya A, Linton DM, Sviri S. Communication difficulties and psychoemotional distress in patients receiving mechanical ventilation. Am J Crit Care. 2011; 20:470–9.34. Ten Hoorn S, Elbers PW, Girbes AR, Tuinman PR. Communicating with conscious and mechanically ventilated critically ill patients: a systematic review. Crit Care. 2016; 20:333.35. Grossbach I, Stranberg S, Chlan L. Promoting effective communication for patients receiving mechanical ventilation. Crit Care Nurse. 2011; 31:46–60.36. Dithole KS, Thupayagale-Tshweneagae G, Akpor OA, Moleki MM. Communication skills intervention: promoting effective communication between nurses and mechanically ventilated patients. BMC Nurs. 2017; 16:74.37. Happ MB, Garrett KL, Tate JA, DiVirgilio D, Houze MP, Demirci JR, et al. Effect of a multi-level intervention on nurse-patient communication in the intensive care unit: results of the SPEACS trial. Heart Lung. 2014; 43:89–98.38. Noguchi A, Inoue T, Yokota I. Promoting a nursing team's ability to notice intent to communicate in lightly sedated mechanically ventilated patients in an intensive care unit: an action research study. Intensive Crit Care Nurs. 2019; 51:64–72.39. Gorzin K, Sanagoo A, Jouybari L, Pahlavanzadeh B, Jesmi AA. The effect of education on function and communication skill of nurse with intubated patient in intensive care unit. J Nurs Midwifery Sci. 2020; 7:84–7.40. Walker LO, Avant KC. Strategies for theory construction in nursing. Pearson;2005.41. Wanko Keutchafo EL, Kerr J, Jarvis MA. Evidence of nonverbal communication between nurses and older adults: a scoping review. BMC Nurs. 2020; 19:53.42. Abdolrahimi M, Ghiyasvandian S, Zakerimoghadam M, Ebadi A. Therapeutic communication in nursing students: a Walker & Avant concept analysis. Electron Physician. 2017; 9:4968–77.43. Xue W, Heffernan C. Therapeutic communication within the nurse-patient relationship: a concept analysis. Int J Nurs Pract. 2021; 27:e12938.44. Guttormson JL, Bremer KL, Jones RM. "Not being able to talk was horrid": a descriptive, correlational study of communication during mechanical ventilation. Intensive Crit Care Nurs. 2015; 31:179–86.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Scoping Review Approach to Synthesize Nursing Research Evidence
- Evaluation of Nurses' Competency in Nurse-Patient Communication about Medications: Conversational Analysis Approach
- Conversation Analysis for Improving Nursing Communication
- The Application of Augmentative and Alternative Communication in Intubated Patients in the Intensive Care Unit: A Scoping Review
- Comparison of salivary and serum cortisol levels in mechanically ventilated patients and non-critically ill patients