Acute Crit Care.
2022 Nov;37(4):592-600. 10.4266/acc.2022.00325.
Agreement between two methods for assessment of maximal inspiratory pressure in patients weaning from mechanical ventilation
- Affiliations
-
- 1Postgraduate Program in Physiotherapy, Federal University of Pernambuco, Recife, Brazil
- 2Department of Rehabilitation Sciences, Faculty of Movement and Rehabilitation Sciences, University Hospitals Leuven, Katholieke Universiteit of Leuven, Leuven, Belgium
- 3Department of Intensive Care Medicine, Hospital Agamenon Magalhães, Recife, Brazil
- 4Health Applied Biology Graduate Program, Federal University of Pernambuco, Recife, Brazil
- KMID: 2540147
- DOI: http://doi.org/10.4266/acc.2022.00325
Abstract
- Background
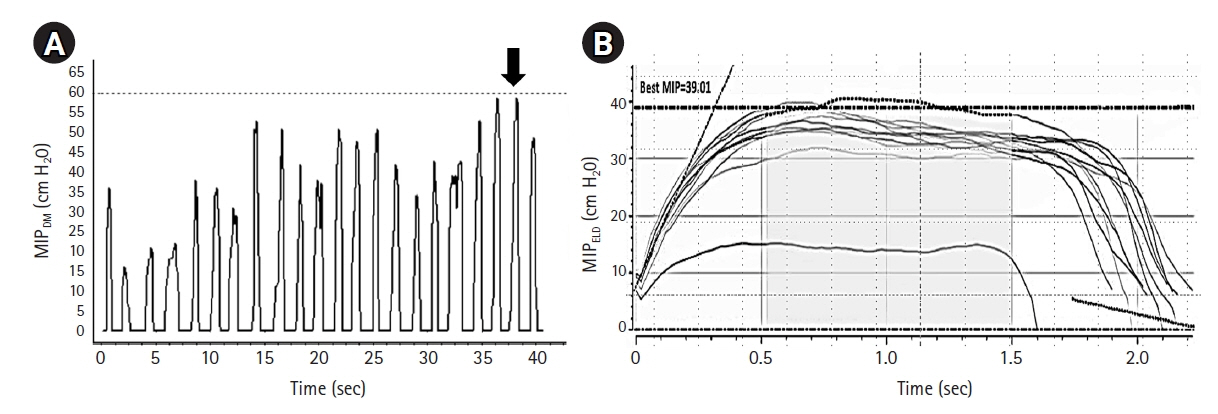
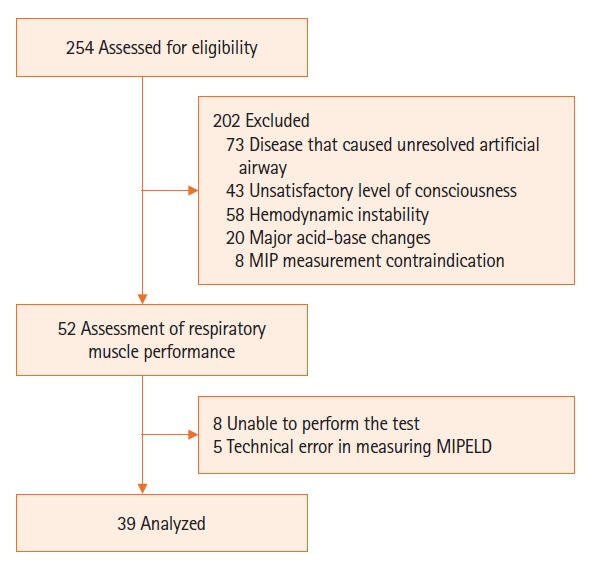
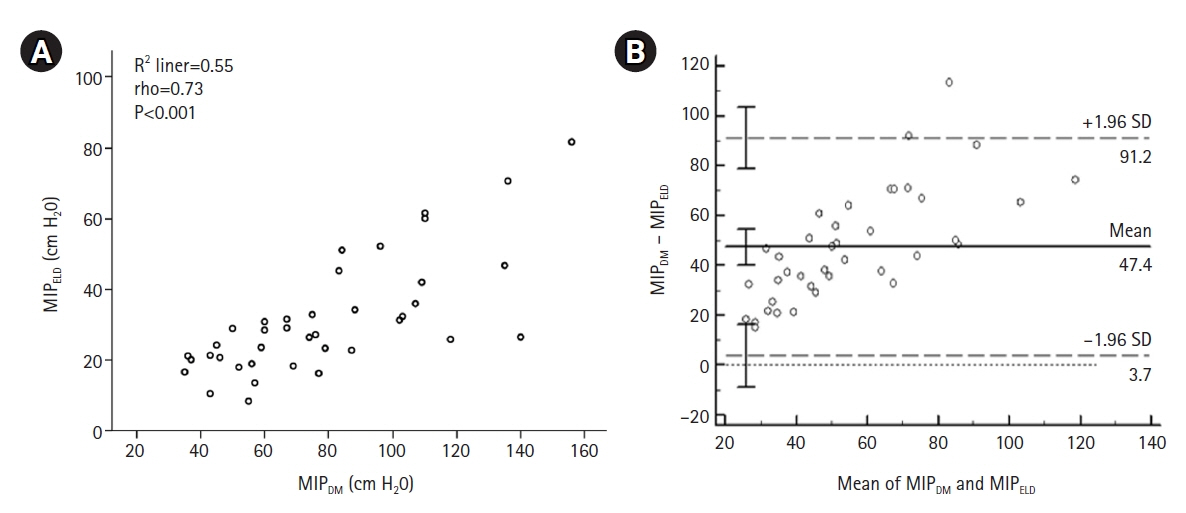
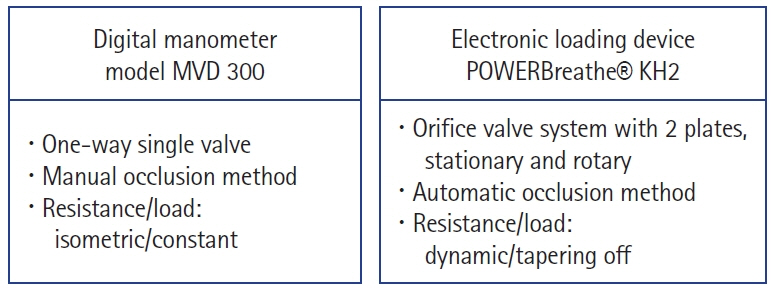
Respiratory muscle strength in patients with an artificial airway is commonly assessed as the maximal inspiratory pressure (MIP) and is measured using analogue or digital manometers. Recently, new electronic loading devices have been proposed to measure respiratory muscle strength. This study evaluates the agreement between the MIPs measured by a digital manometer and those according to an electronic loading device in patients being weaned from mechanical ventilation. Methods: In this prospective study, the standard MIP was obtained using a protocol adapted from Marini, in which repetitive inspiratory efforts were performed against an occluded airway with a one-way valve and were recorded with a digital manometer for 40 seconds (MIPDM). The MIP measured using the electronic loading device (MIPELD) was obtained from repetitively tapered flow resistive inspirations sustained for at least 2 seconds during a 40-second test. The agreement between the results was verified by a Bland-Altman analysis. Results: A total of 39 subjects (17 men, 55.4±17.7 years) was enrolled. Although a strong correlation between MIPDM and MIPELD (R=0.73, P<0.001) was observed, the Bland-Altman analysis showed a high bias of –47.4 (standard deviation, 22.3 cm H2O; 95% confidence interval, –54.7 to –40.2 cm H2O). Conclusions: The protocol of repetitively tapering flow resistive inspirations to measure the MIP with the electronic loading device is not in agreement with the standard protocol using one-way valve inspiratory occlusion when applied in poorly cooperative patients being weaned from mechanical ventilation.
Keyword
Figure
Reference
-
1. Medrinal C, Prieur G, Frenoy É, Robledo Quesada A, Poncet A, Bonnevie T, et al. Respiratory weakness after mechanical ventilation is associated with one-year mortality: a prospective study. Crit Care. 2016; 20:231.2. De Jonghe B, Bastuji-Garin S, Durand MC, Malissin I, Rodrigues P, Cerf C, et al. Respiratory weakness is associated with limb weakness and delayed weaning in critical illness. Crit Care Med. 2007; 35:2007–15.
Article3. Dres M, Demoule A. Diaphragm dysfunction during weaning from mechanical ventilation: an underestimated phenomenon with clinical implications. Crit Care. 2018; 22:73.
Article4. Laveneziana P, Albuquerque A, Aliverti A, Babb T, Barreiro E, Dres M, et al. ERS statement on respiratory muscle testing at rest and during exercise. Eur Respir J. 2019; 53:1801214.
Article5. Caruso P, Albuquerque AL, Santana PV, Cardenas LZ, Ferreira JG, Prina E, et al. Diagnostic methods to assess inspiratory and expiratory muscle strength. J Bras Pneumol. 2015; 41:110–23.
Article6. Marini JJ, Smith TC, Lamb V. Estimation of inspiratory muscle strength in mechanically ventilated patients: the measurement of maximal inspiratory pressure. J Crit Care. 1986; 1:32–8.
Article7. Truwit JD, Marini JJ. Validation of a technique to assess maximal inspiratory pressure in poorly cooperative patients. Chest. 1992; 102:1216–9.
Article8. American Thoracic Society/European Respiratory Society. ATS/ERS Statement on respiratory muscle testing. Am J Respir Crit Care Med. 2002; 166:518–624.9. Medrinal C, Prieur G, Combret Y, Quesada AR, Bonnevie T, Gravier FE, et al. Reliability of respiratory pressure measurements in ventilated and non-ventilated patients in ICU: an observational study. Ann Intensive Care. 2018; 8:14.
Article10. Pinheiro Filho GR, Reis HF, Almeida ML, Andrade WS, Rocha RL, Leite PA. Comparison and effects of two different airway occlusion times during measurement of maximal inspiratory pressure in adult intensive care unit neurological patients. Rev Bras Ter Intensiva. 2010; 22:33–9.11. de Souza LC, da Silva CT Jr, Lugon JR. Evaluation of the inspiratory pressure using a digital vacuometer in mechanically ventilated patients: analysis of the time to achieve the inspiratory peak. Respir Care. 2012; 57:257–62.
Article12. Guimarães FS, Alves FF, Constantino SS, Dias CM, Menezes SL. Maximal inspiratory pressure evaluation among non-cooperative critical patients: comparison between two methods. Braz J Phys Ther. 2007; 11:233–8.13. Minahan C, Sheehan B, Doutreband R, Kirkwood T, Reeves D, Cross T. Repeated-sprint cycling does not induce respiratory muscle fatigue in active adults: measurements from the powerbreathe® inspiratory muscle trainer. J Sports Sci Med. 2015; 14:233–8.14. Spurling DA, Lam DH, Skelton A, McConnell AK, Cecelja F, Broomhead P, inventors. Respiratory muscle training device. United States patent US 8.459.255 B2. 2013 Jun 11.15. Langhan ML, Riera A, Kurtz JC, Schaeffer P, Asnes AG. Implementation of newly adopted technology in acute care settings: a qualitative analysis of clinical staff. J Med Eng Technol. 2015; 39:44–53.
Article16. Hendra KP, Bonis PA, Joyce-Brady M. Development and prospective validation of a model for predicting weaning in chronic ventilator dependent patients. BMC Pulm Med. 2003; 3:3.
Article17. Zhang JB, Zhu JQ, Cao LX, Jin XH, Chen LL, Song YK, et al. Use of the modified Glasgow Coma Scale score to guide sequential invasive-noninvasive mechanical ventilation weaning in patients with AECOPD and respiratory failure. Exp Ther Med. 2020; 20:1441–6.
Article18. de Souza LC, Guimarães FS, Lugon JR. Evaluation of a new index of mechanical ventilation weaning: the timed inspiratory effort. J Intensive Care Med. 2015; 30:37–43.
Article19. Caruso P, Friedrich C, Denari SD, Ruiz SA, Deheinzelin D. The unidirectional valve is the best method to determine maximal inspiratory pressure during weaning. Chest. 1999; 115:1096–101.
Article20. Giavarina D. Understanding Bland Altman analysis. Biochem Med (Zagreb). 2015; 25:141–51.
Article21. Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986; 327:307–10.
Article22. Ratnovsky A, Elad D, Halpern P. Mechanics of respiratory muscles. Respir Physiol Neurobiol. 2008; 163:82–9.
Article23. Whitelaw WA, Derenne JP, Milic-Emili J. Occlusion pressure as a measure of respiratory center output in conscious man. Respir Physiol. 1975; 23:181–99.24. Silva PE, de Carvalho KL, Frazão M, Maldaner V, Daniel CR, Gomes-Neto M. Assessment of maximum dynamic inspiratory pressure. Respir Care. 2018; 63:1231–8.
Article25. Marshall R. Relationships between stimulus and work of breathing at different lung volumes. J Appl Physiol. 1962; 17:917–21.
Article26. McDonald T, Stiller K. Inspiratory muscle training is feasible and safe for patients with acute spinal cord injury. J Spinal Cord Med. 2019; 42:220–7.
Article27. Langer D, Jacome C, Charususin N, Scheers H, McConnell A, Decramer M, et al. Measurement validity of an electronic inspiratory loading device during a loaded breathing task in patients with COPD. Respir Med. 2013; 107:633–5.
Article28. Bissett BM, Leditschke IA, Neeman T, Boots R, Paratz J. Inspiratory muscle training to enhance recovery from mechanical ventilation: a randomised trial. Thorax. 2016; 71:812–9.
Article29. Vorona S, Sabatini U, Al-Maqbali S, Bertoni M, Dres M, Bissett B, et al. Inspiratory muscle rehabilitation in critically ill adults: a systematic review and meta-analysis. Ann Am Thorac Soc. 2018; 15:735–44.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Initial Weaning Success Rates and Weaning Periods between Synchronized Intermittent Mandatory Ventilation and Pressure Support Ventilation
- Respiratory Parameters of Pressure Support Ventilation and Synchronized Intermittent Mandatory Ventilation during the Weaning Process
- Weaning Approach with Weaning Index for Postoperative Patients with Mechanical Ventilator Support in the ICU
- A Comparison of Clinical Efficacy of Weaning Method Between the Mode of Intermittent Mandatory Ventilation and Intermittent Mandatory Ventilation Plus Pressure Support
- The Usefulness of Noninvasive Positive Pressure Ventilation as a New Weaning Method