Acute Crit Care.
2022 Nov;37(4):491-501. 10.4266/acc.2022.01158.
Asynchronies during invasive mechanical ventilation: narrative review and update
- Affiliations
-
- 1Servicio de Medicina Física y Rehabilitación, Hospital Alemán, Buenos Aires, Argentina
- 2Servicio de Medicina Física y Rehabilitación, Hospital San Juan de Dios, La Serena, Chile
- 3Servicio de Rehabilitación en UCI, Hospital General de México Dr. Eduardo Liceaga, Ciudad de México, México
- 4Servicio de Kinesiología, Hospital El Carmen, Godoy Cruz, Mendoza, Argentina
- 5Servicio de Kinesiología, Sanatorio Clínica Modelo de Morón, Buenos Aires, Argentina
- KMID: 2540137
- DOI: http://doi.org/10.4266/acc.2022.01158
Abstract
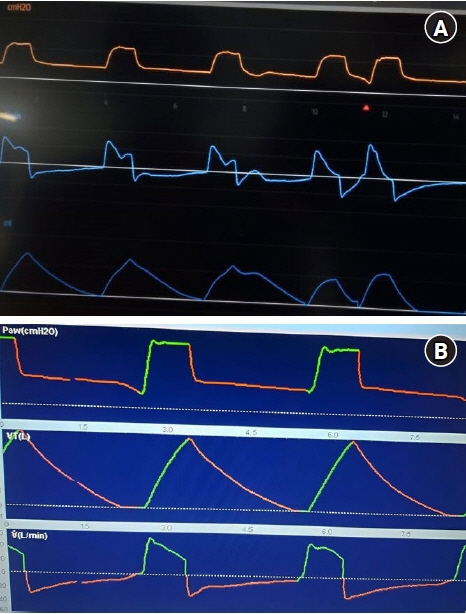
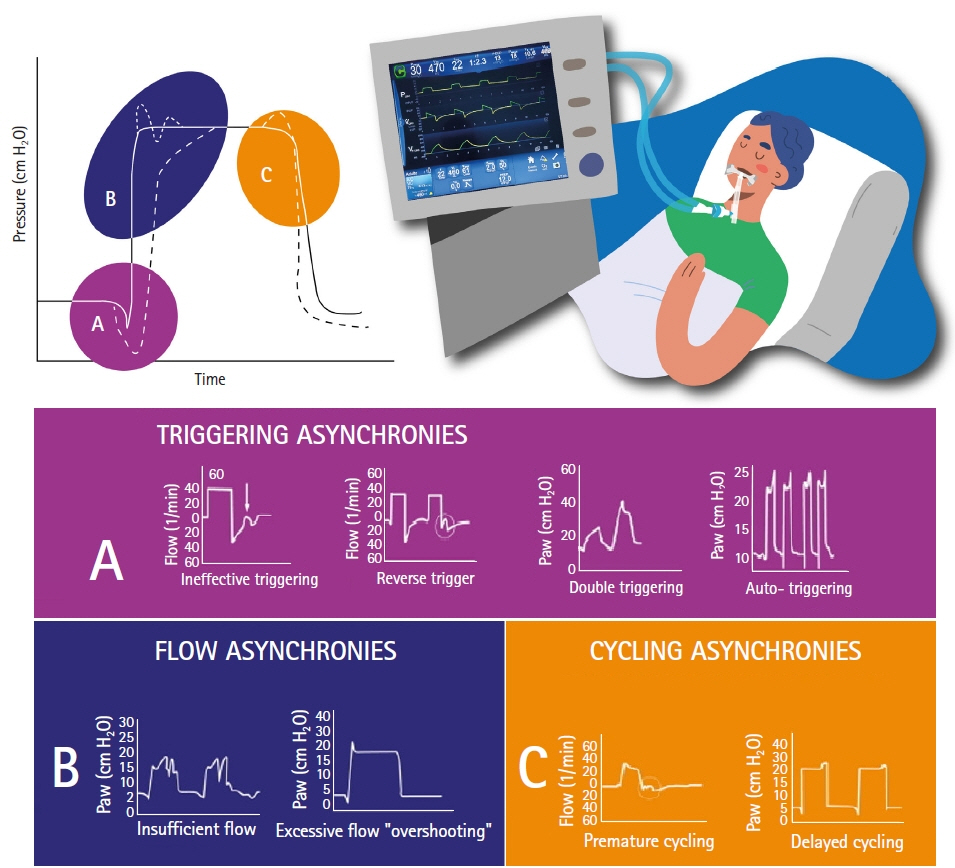
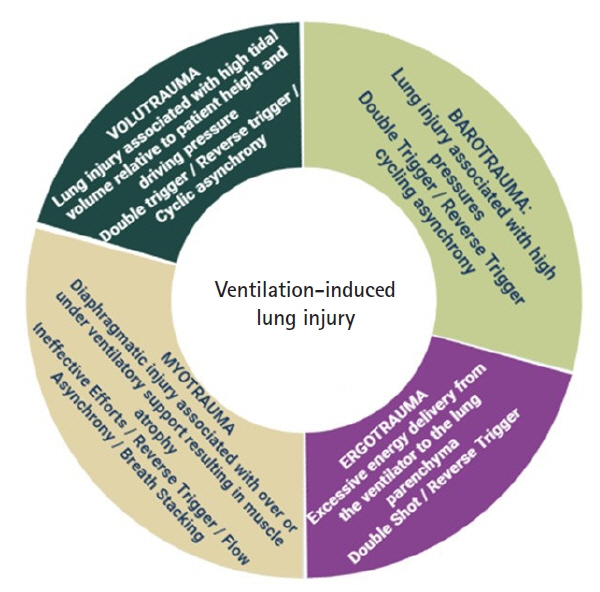
- Invasive mechanical ventilation is a frequent therapy in critically ill patients in critical care units. To achieve favorable outcomes, patient and ventilator interaction must be adequate. However, many clinical situations could attempt against this principle and generate a mismatch between these two actors. These asynchronies can lead the patient to worst outcomes; that is why it is vital to recognize and treat these entities as soon as possible. Early detection and recognition of the different asynchronies could favor the reduction of the days of mechanical ventilation, the days of hospital stay, and intensive care and improve clinical results.
Figure
Reference
-
1. Wunsch H, Linde-zwirble WT, Angus DC, Hartman ME, Milbrandt EB, Kahn JM. The epidemiology of mechanical ventilation use in the United States. Crit Care Med. 2010; 38:1947–53.
Article2. Bruni A, Garofalo E, Pelaia C, Messina A, Cammarota G, Murabito P, et al. Patient-ventilator asynchrony in adult critically ill patients. Minerva Anestesiol. 2019; 85:676–88.
Article3. Magrans R, Ferreira F, Sarlabous L, López-Aguilar J, Gomà G, Fernandez-Gonzalo S, et al. The effect of clusters of double triggering and ineffective efforts in critically ill patients. Crit Care Med. 2022; 50:e619–29.
Article4. Jonkman AH, Holleboom MC, de Vries HJ, Vriends M, Tuinman PR, Heunks LM. Expiratory muscle relaxation-induced ventilator triggering: a novel patient-ventilator dyssynchrony. Chest. 2022; 161:e337–41.5. Oto B, Annesi J, Foley RJ. Patient-ventilator dyssynchrony in the intensive care unit: a practical approach to diagnosis and management. Anaesth Intensive Care. 2021; 49:86–97.
Article6. Barwing J, Pedroni C, Olgemöller U, Quintel M, Moerer O. Electrical activity of the diaphragm (EAdi) as a monitoring parameter in difficult weaning from respirator: a pilot study. Crit Care. 2013; 17:R182.
Article7. Hickey SM, Giwa AO. Mechanical ventilation [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 [cited 2022 Jan 28]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539742/.8. Chen S, Li Y, Zheng Z, Luo Q, Chen R. The analysis of components that lead to increased work of breathing in chronic obstructive pulmonary disease patients. J Thorac Dis. 2016; 8:2212–8.
Article9. Cabello B, Mancebo J. Work of breathing. Intensive Care Med. 2006; 32:1311–4.
Article10. French CJ. Work of breathing measurement in the critically ill patient. Anaesth Intensive Care. 1999; 27:561–73.
Article11. Parthasarathy S, Jubran A, Tobin MJ. Assessment of neural inspiratory time in ventilator-supported patients. Am J Respir Crit Care Med. 2000; 162(2 Pt 1):546–52.
Article12. Shah VH, Samanta A, Ray S. Patient-ventilator asynchrony: etiology and solutions. Indian J Clin Pract. 2021; 31:714–24.13. Spinelli E, Mauri T, Beitler JR, Pesenti A, Brodie D. Respiratory drive in the acute respiratory distress syndrome: pathophysiology, monitoring, and therapeutic interventions. Intensive Care Med. 2020; 46:606–18.
Article14. Vaporidi K, Akoumianaki E, Telias I, Goligher EC, Brochard L, Georgopoulos D. Respiratory drive in critically ill patients: pathophysiology and clinical implications. Am J Respir Crit Care Med. 2020; 201:20–32.
Article15. Jonkman AH, de Vries HJ, Heunks LM. Physiology of the respiratory drive in ICU patients: implications for diagnosis and treatment. Crit Care. 2020; 24:104.
Article16. Telias I, Spadaro S. Techniques to monitor respiratory drive and inspiratory effort. Curr Opin Crit Care. 2020; 26:3–10.
Article17. Pham T, Telias I, Piraino T, Yoshida T, Brochard LJ. Asynchrony consequences and management. Crit Care Clin. 2018; 34:325–41.
Article18. Varon J, Fromm R, Rodarte J, Reinoso M. Prevalence of patient ventilator asynchrony in critically ill patients. Chest. 1994; 106(2 Suppl):141S–144S.19. Thille AW, Rodriguez P, Cabello B, Lellouche F, Brochard L. Patient-ventilator asynchrony during assisted mechanical ventilation. Intensive Care Med. 2006; 32:1515–22.
Article20. Blanch L, Villagra A, Sales B, Montanya J, Lucangelo U, Luján M, et al. Asynchronies during mechanical ventilation are associated with mortality. Intensive Care Med. 2015; 41:633–41.
Article21. Kyo M, Shimatani T, Hosokawa K, Taito S, Kataoka Y, Ohshimo S, et al. Patient-ventilator asynchrony, impact on clinical outcomes and effectiveness of interventions: a systematic review and meta-analysis. J Intensive Care. 2021; 9:50.
Article22. Mireles-Cabodevila E, Siuba MT, Chatburn RL. A taxonomy for patient-ventilator interactions and a method to read ventilator waveforms. Respir Care. 2022; 67:129–48.
Article23. Esperanza JA, Sarlabous L, de Haro C, Magrans R, Lopez-Aguilar J, Blanch L. Monitoring asynchrony during invasive mechanical ventilation. Respir Care. 2020; 65:847–69.
Article24. Akoumianaki E, Maggiore SM, Valenza F, Bellani G, Jubran A, Loring SH, et al. The application of esophageal pressure measurement in patients with respiratory failure. Am J Respir Crit Care Med. 2014; 189:520–31.
Article25. de Vries HJ, Jonkman AH, Tuinman PR, Girbes AR, Heunks LM. Respiratory entrainment and reverse triggering in a mechanically ventilated patient. Ann Am Thorac Soc. 2019; 16:499–505.
Article26. Rodriguez PO, Tiribelli N, Fredes S, Gogniat E, Plotnikow G, Fernandez Ceballos I, et al. Prevalence of reverse triggering in early ARDS: results from a multicenter observational study. Chest. 2021; 159:186–95.27. Dianti J, Bertoni M, Goligher EC. Monitoring patient-ventilator interaction by an end-expiratory occlusion maneuver. Intensive Care Med. 2020; 46:2338–41.
Article28. Baedorf Kassis E, Su HK, Graham AR, Novack V, Loring SH, Talmor DS. Reverse trigger phenotypes in acute respiratory distress syndrome. Am J Respir Crit Care Med. 2021; 203:67–77.
Article29. Lin Z, Zhou J, Lin X, Wang Y, Zheng H, Huang W, et al. Reverse trigger in ventilated non-ards patients: a phenomenon can not be ignored! Front Physiol. 2021; 12:670172.
Article30. Acute Respiratory Distress Syndrome Network, Brower RG, Matthay MA, Morris A, Schoenfeld D, Thompson BT, et al. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000; 342:1301–8.
Article31. He X, Luo XY, Chen GQ, Zhou JX. Detection of reverse triggering in a 55-year-old man under deep sedation and controlled mechanical ventilation. J Thorac Dis. 2018; 10:E682–5.
Article32. Imanaka H, Nishimura M, Takeuchi M, Kimball WR, Yahagi N, Kumon K. Autotriggering caused by cardiogenic oscillation during flow-triggered mechanical ventilation. Crit Care Med. 2000; 28:402–7.
Article33. Holanda MA, Vasconcelos RD, Ferreira JC, Pinheiro BV. Patient-ventilator asynchrony. J Bras Pneumol. 2018; 44:321–33.
Article34. Georgopoulos D, Prinianakis G, Kondili E. Bedside waveforms interpretation as a tool to identify patient-ventilator asynchronies. Intensive Care Med. 2006; 32:34–47.
Article35. Blanch L, Sales B, Montanya J, Lucangelo U, Garcia-Esquirol O, Villagra A, et al. Validation of the Better Care® system to detect ineffective efforts during expiration in mechanically ventilated patients: a pilot study. Intensive Care Med. 2012; 38:772–80.
Article36. Sassoon CS. Triggering of the ventilator in patient-ventilator interactions. Respir Care. 2011; 56:39–51.
Article37. Mirabella L, Cinnella G, Costa R, Cortegiani A, Tullo L, Rauseo M, et al. Patient-ventilator asynchronies: clinical implications and practical solutions. Respir Care. 2020; 65:1751–66.
Article38. de Haro C, López-Aguilar J, Magrans R, Montanya J, Fernández-Gonzalo S, Turon M, et al. Double cycling during mechanical ventilation: frequency, mechanisms, and physiologic implications. Crit Care Med. 2018; 46:1385–92.39. Holanda MA, Vasconcelos R, Ferreira JC, Pinheiro BV. Patient-ventilator asynchrony. J Bras Pneumol. 2018; 44:321–33.
Article40. Colombo D, Cammarota G, Alemani M, Carenzo L, Barra FL, Vaschetto R, et al. Efficacy of ventilator waveforms observation in detecting patient-ventilator asynchrony. Crit Care Med. 2011; 39:2452–7.
Article41. Ramirez II, Arellano DH, Adasme RS, Landeros JM, Salinas FA, Vargas AG, et al. Ability of ICU health-care professionals to identify patient-ventilator asynchrony using Waveform analysis. Respir Care. 2017; 62:144–9.
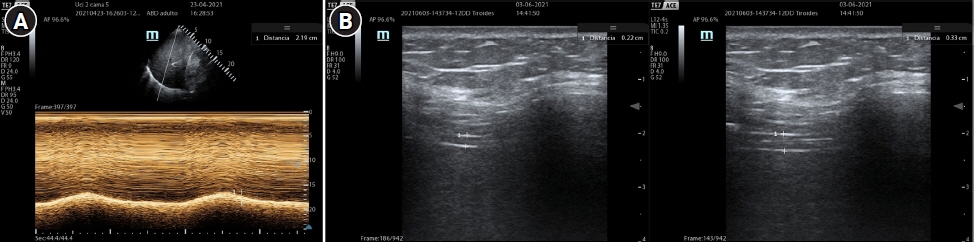
Article42. Soilemezi E, Vasileiou M, Spyridonidou C, Tsagourias M, Matamis D. Understanding patient-ventilator asynchrony using diaphragmatic ultrasonography. Am J Respir Crit Care Med. 2019; 200:e27–8.
Article43. Mauri T, Yoshida T, Bellani G, Goligher EC, Carteaux G, Rittayamai N, et al. Esophageal and transpulmonary pressure in the clinical setting: meaning, usefulness and perspectives. Intensive Care Med. 2016; 42:1360–73.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment of acute respiratory failure: invasive mechanical ventilation
- Home mechanical ventilation in children with chronic respiratory failure: a narrative review
- The Comparative Study of Central Venous Pressure Measurements during Mechanical Ventilation and after Disconnection of Ventilation
- Acute Neuromuscular Respiratory Failure
- Respiratory Failure in Guillain-Barre Syndrome