J Korean Med Sci.
2023 Mar;38(9):e69. 10.3346/jkms.2023.38.e69.
Increased Prehospital Emergency Medical Service Time Interval and Nontransport Rate of Patients With Fever Using Emergency Medical Services Before and After COVID-19 in Busan, Korea
- Affiliations
-
- 1Department of Emergency Medicine, Dong-A University Hospital, Busan, Korea
- 2Department of Emergency Medicine, College of Medicine, Dong-A University, Busan, Korea
- KMID: 2540127
- DOI: http://doi.org/10.3346/jkms.2023.38.e69
Abstract
- Background
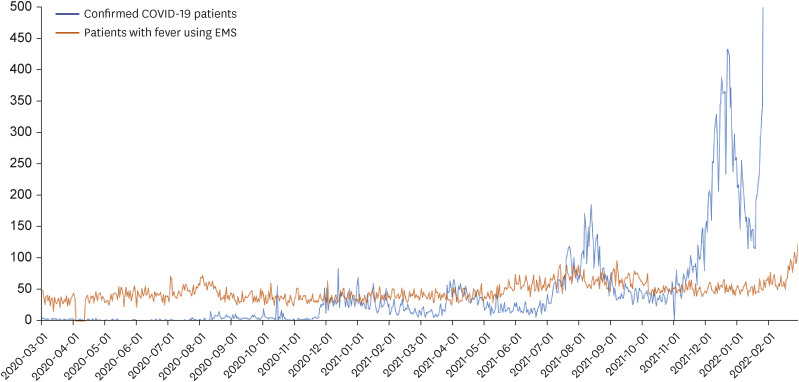
In Korea, patients with fever have been preemptively isolated to isolation beds in the emergency department (ED) since the coronavirus disease 2019 (COVID-19) pandemic began. However, isolation beds were not always available, and transport delays or failure (nontransport), especially for infants, were reported in the media. Few studies have focused on delays and failure in transporting fever patients to the ED. Therefore, this study aimed to examine and compare the emergency medical service (EMS) time interval and nontransport rate of patients with fever using EMSs before and after COVID-19.
Methods
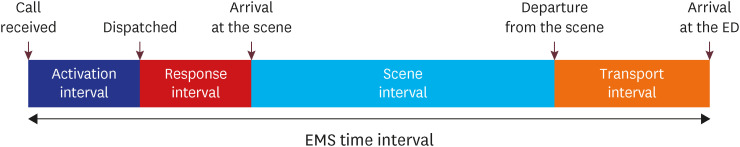
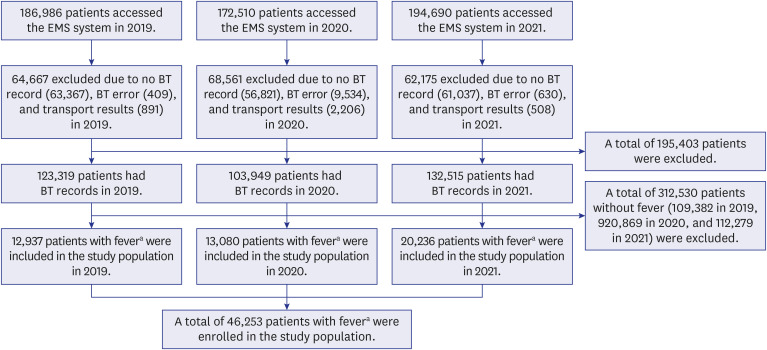
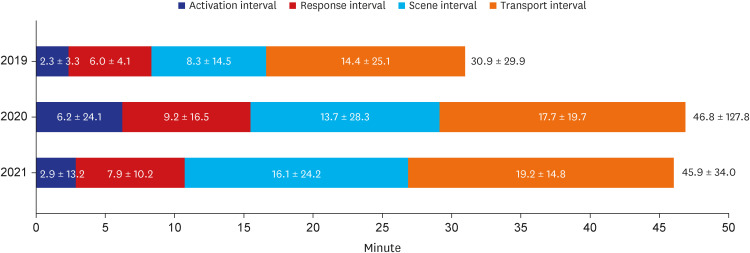
This retrospective observational study analyzed the prehospital EMS time interval and nontransport rate of fever patients who contacted EMSs in Busan, South Korea, from March 1, 2019 to February 28, 2022, using emergency dispatch reports. All fever patients (≥ 37.5°C) who contacted EMSs during this study were included. The EMS time interval was defined as the time between the patient’s EMS call and ED arrival time. Nontransport was defined as a case recorded as not being transported in the emergency dispatch reports. The study population of 2019 was compared to the population of 2020 and 2021 with the independent t-test, Mann-Whitney U test, and χ 2 test. As a subgroup, the EMS time intervals and nontransport rates of infants with fever were compared before and after COVID-19.
Results
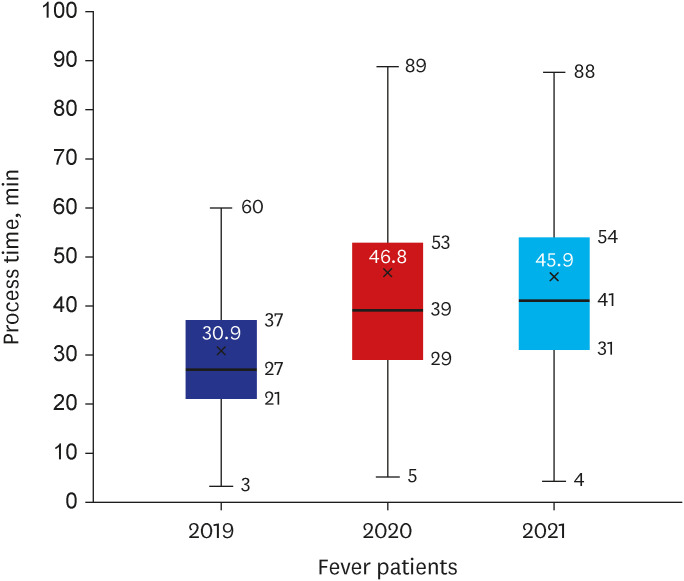
A total of 554,186 patients accessed the EMS during the study period, and 46,253 patients with fever were included. The EMS time interval (mean ± standard deviation, minutes) of fever patients was 30.9 ± 29.9 in 2019, 46.8 ± 127.8 in 2020 (P < 0.001) and 45.9 ± 34.0 in 2021 ( P < 0.001). The nontransport rate (%) was 4.4 in 2019, 20.6 in 2020 (P < 0.001), and 19.5 in 2021 (P < 0.001). For infants with fever, the EMS time interval was 27.6 ± 10.8 in 2019, 35.1 ± 15.4 in 2020 (P < 0.001), and 42.3 ± 20.5 in 2021 (P < 0.001), and the nontransport rate (%) was 2.6 in 2019, 25.0 in 2020, and 19.7 in 2021.
Conclusion
After the emergence of COVID-19, in Busan, the EMS time interval of fever patients was delayed, and approximately 20% of fever patients were not transported. However, infants with fever had shorter EMS time intervals and higher nontransport rates than the overall study population. A comprehensive approach, including prehospital and hospital ED flow improvements, is required beyond increasing the number of isolation beds.
Figure
Reference
-
1. World Health Organization. WHO coronavirus (COVID-19) dashboard. Updated 2020. Accessed September 9, 2022. https://covid19.who.int/ .2. Kim S, Ko Y, Kim YJ, Jung E. The impact of social distancing and public behavior changes on COVID-19 transmission dynamics in the Republic of Korea. PLoS One. 2020; 15(9):e0238684. PMID: 32970716.3. Peck KR. Early diagnosis and rapid isolation: response to COVID-19 outbreak in Korea. Clin Microbiol Infect. 2020; 26(7):805–807. PMID: 32344168.4. Edelson DP, Sasson C, Chan PS, Atkins DL, Aziz K, Becker LB, et al. Interim guidance for basic and advanced life support in adults, children, and neonates with suspected or confirmed COVID-19: from the emergency cardiovascular care committee and get with the guidelines-resuscitation adult and pediatric task forces of the American Heart Association. Circulation. 2020; 141(25):e933–e943. PMID: 32270695.5. Seo AR, Lee WJ, Woo SH, Moon J, Kim D. Pre-hospital delay in patients with acute stroke during the initial phase of the coronavirus disease 2019 outbreak. J Korean Med Sci. 2022; 37(6):e47. PMID: 35166083.6. Choi H, Lee JH, Park HK, Lee E, Kim MS, Kim HJ, et al. Impact of the COVID-19 Pandemic on Patient Delay and Clinical Outcomes for Patients With Acute Myocardial Infarction. J Korean Med Sci. 2022; 37(21):e167. PMID: 35638194.7. Lim D, Park SY, Choi B, Kim SH, Ryu JH, Kim YH, et al. The comparison of emergency medical service responses to and outcomes of out-of-hospital cardiac arrest before and during the COVID-19 pandemic in an area of Korea. J Korean Med Sci. 2021; 36(36):e255. PMID: 34519188.8. Friedman J, Calderón-Villarreal A, Bojorquez I, Vera Hernández C, Schriger DL, Tovar Hirashima E. Excess out-of-hospital mortality and declining oxygen saturation: the sentinel role of emergency medical services data in the COVID-19 crisis in Tijuana, Mexico. Ann Emerg Med. 2020; 76(4):413–426. PMID: 33012377.9. Prezant DJ, Lancet EA, Zeig-Owens R, Lai PH, Appel D, Webber MP, et al. System impacts of the COVID-19 pandemic on New York City’s emergency medical services. J Am Coll Emerg Physicians Open. 2020; 1(6):1205–1213. PMID: 33392524.10. Spina S, Marrazzo F, Migliari M, Stucchi R, Sforza A, Fumagalli R. The response of Milan’s emergency medical system to the COVID-19 outbreak in Italy. Lancet. 2020; 395(10227):e49–e50. PMID: 32119824.11. Fagoni N, Perone G, Villa GF, Celi S, Bera P, Sechi GM, et al. The Lombardy emergency medical system faced with COVID-19: the impact of out-of-hospital outbreak. Prehosp Emerg Care. 2021; 25(1):1–7. PMID: 32940538.12. Statistical Geographical Information Service. Statistical Geographical Information Service homepage. Update 2022. Accessed September 9, 2022. https://sgis.kostat.go.kr/jsp/english/index.jsp .13. Kim J, Kim C, Park SY. Impact of COVID-19 on emergency medical services for patients with acute stroke presentation in Busan, South Korea. J Clin Med. 2021; 11(1):94. PMID: 35011835.14. Spaite DW, Valenzuela TD, Meislin HW, Criss EA, Hinsberg P. Prospective validation of a new model for evaluating emergency medical services systems by in-field observation of specific time intervals in prehospital care. Ann Emerg Med. 1993; 22(4):638–645. PMID: 8457088.15. Eitel DR, Rudkin SE, Malvehy MA, Killeen JP, Pines JM. Improving service quality by understanding emergency department flow: a white paper and position statement prepared for the American Academy of Emergency Medicine. J Emerg Med. 2010; 38(1):70–79. PMID: 18514465.16. Asplin BR, Flottemesch TJ, Gordon BD. Developing models for patient flow and daily surge capacity research. Acad Emerg Med. 2006; 13(11):1109–1113. PMID: 17015412.17. National Emergency Medical Center. General situation board. Updated 2022. Accessed September 9, 2022. https://portal.nemc.or.kr:444/medi_info/dashboards/dash_total_emer_org_popup_for_egen.do .18. Asaro PV, Lewis LM, Boxerman SB. The impact of input and output factors on emergency department throughput. Acad Emerg Med. 2007; 14(3):235–242. PMID: 17284466.19. Guo F, Qin Y, Fu H, Xu F. The impact of COVID-19 on emergency department length of stay for urgent and life-threatening patients. BMC Health Serv Res. 2022; 22(1):696. PMID: 35610608.20. Lucero A, Sokol K, Hyun J, Pan L, Labha J, Donn E, et al. Worsening of emergency department length of stay during the COVID-19 pandemic. J Am Coll Emerg Physicians Open. 2021; 2(3):e12489. PMID: 34189522.21. Satty T, Ramgopal S, Elmer J, Mosesso VN, Martin-Gill C. EMS responses and non-transports during the COVID-19 pandemic. Am J Emerg Med. 2021; 42:1–8. PMID: 33429185.22. Choi HJ, Kim HJ, Lee HJ, Lee BR. Comparison with in-hospital Korean Triage and Acuity Scale (KTAS) and prehospital triage system in a metropolitan city. J Korean Soc Emerg Med. 2018; 29(5):391–398.23. Couturier K, Nelson AR, Burns K, Cone DC, Rollins M, Venkatesh AK, et al. EMS non-transport of low-risk COVID-19 patients. Prehosp Emerg Care. 2022; 1–5.24. Cooney DR, Millin MG, Carter A, Lawner BJ, Nable JV, Wallus HJ. Ambulance diversion and emergency department offload delay: resource document for the National Association of EMS Physicians position statement. Prehosp Emerg Care. 2011; 15(4):555–561. PMID: 21870947.25. Jonkmans N, D’Acremont V, Flahault A.. Scoping future outbreaks: a scoping review on the outbreak prediction of the WHO blueprint list of priority diseases. BMJ Glob Health. 2021; 6(9):e006623.26. Baker RE, Mahmud AS, Miller IF, Rajeev M, Rasambainarivo F, Rice BL, et al. Infectious disease in an era of global change. Nat Rev Microbiol. 2022; 20(4):193–205. PMID: 34646006.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prehospital transport of critically ill children via 119 emergency medical service providers: problems and improvement plan
- Changes in the activity times of 119 ambulance units according to the presence of fever or respiratory symptoms: comparison before and after the pandemic of COVID-19
- The Impact of the COVID-19 Outbreak on Emergency Medical Service: An Analysis of Patient Transportations and Time Intervals
- How to Improve the Emergency Medical Service System: Levels of Knowledge and Techniques in Prehospital Care for 119 Relief Squad Members and Emergency Room Nurses
- Impact of COVID-19 on Out-of-Hospital Cardiac Arrest in Korea