Arch Hand Microsurg.
2023 Mar;28(1):57-62. 10.12790/ahm.22.0070.
Comparison of groin lymph node anatomy in patients with upper-extremity lymphedema and healthy subjects using contrast-enhanced computed tomography
- Affiliations
-
- 1Department of Plastic Surgery, Korea University Ansan Hospital, Ansan, Korea
- KMID: 2540033
- DOI: http://doi.org/10.12790/ahm.22.0070
Abstract
- Purpose
Lymphedema is a chronic disease that affects patients’ quality of life. Vascularized groin lymph node transfer is a reliable treatment that requires detailed anatomic knowledge of the superficial inguinal lymph nodes (SILNs). This study compared the anatomy of SILNs between patients with upper-extremity lymphedema and individuals without lymphedema using pelvic computed tomography (CT).
Methods
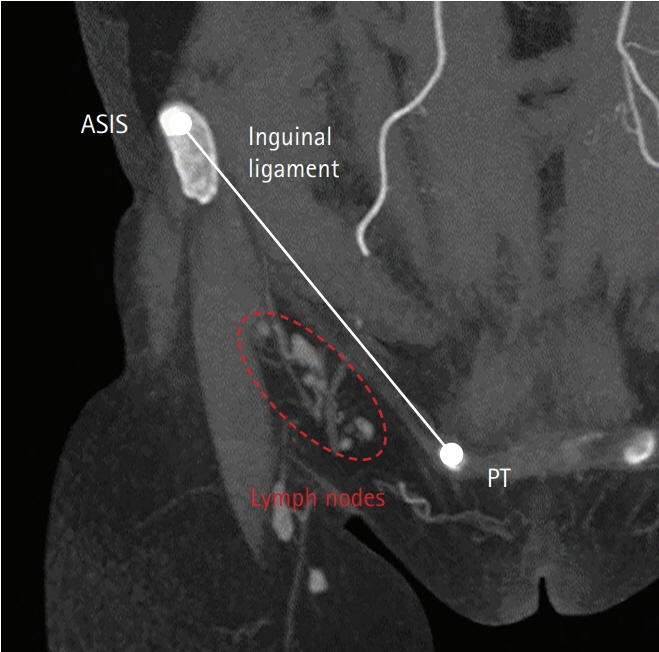
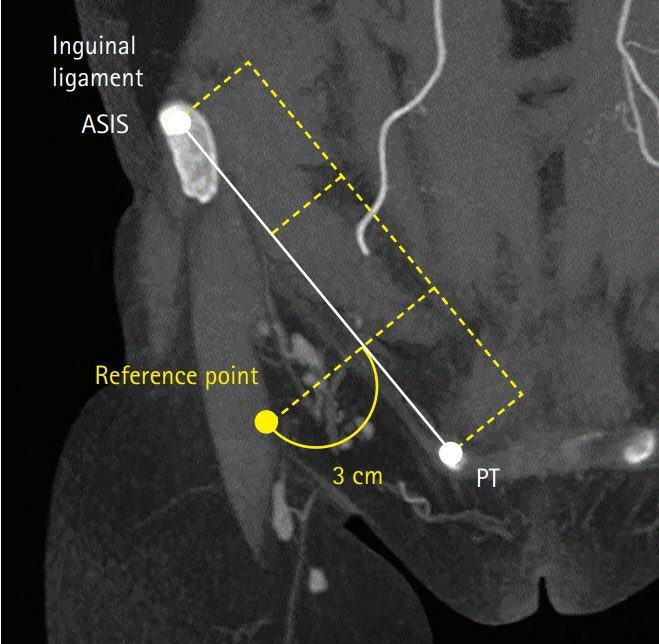
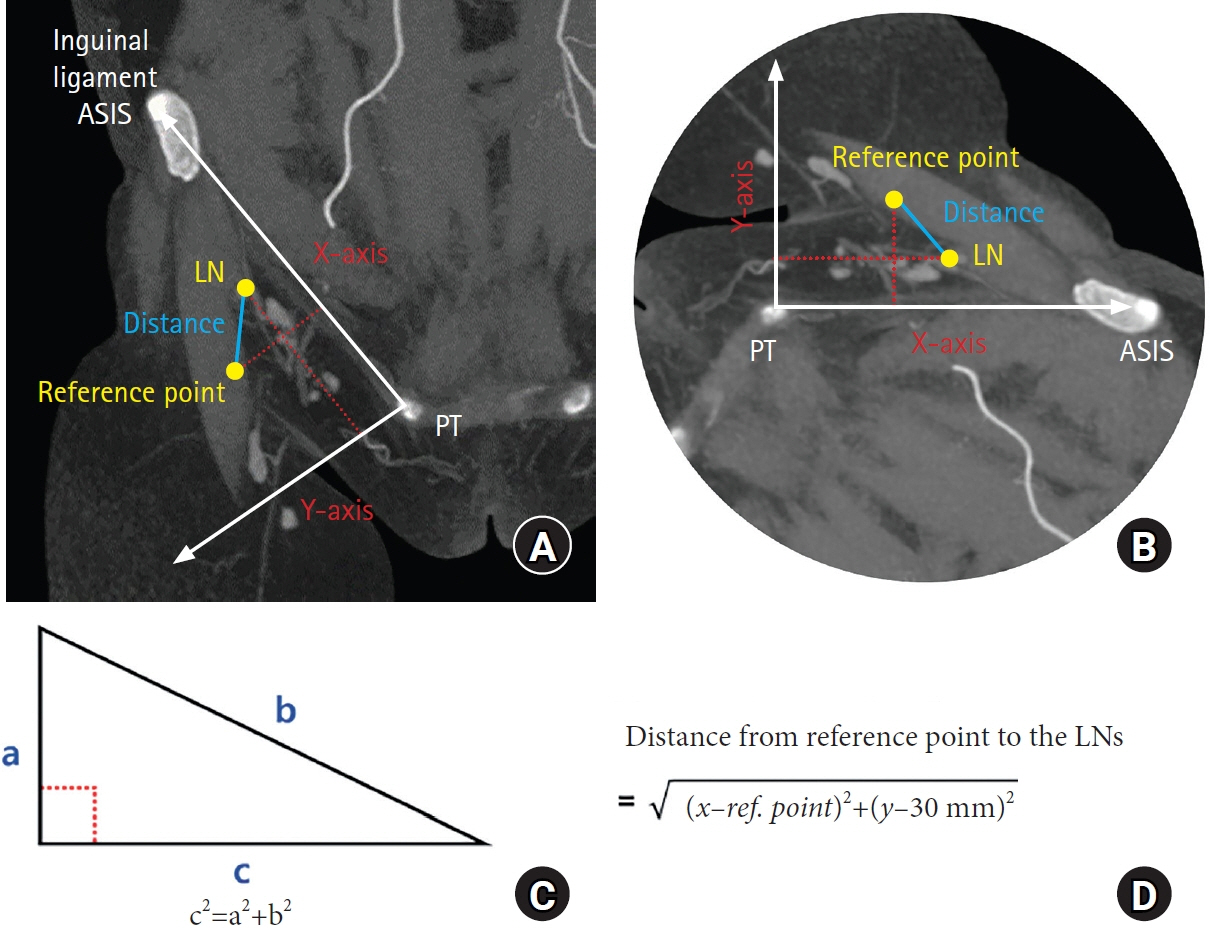
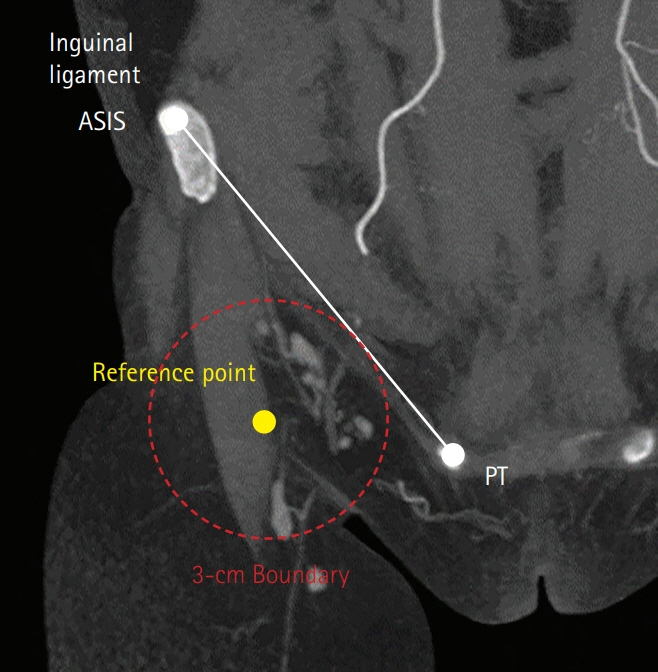
The CT scans of 17 patients (the patient group) with upper-extremity lymphedema and 34 individuals without lymphedema (the normal group) were studied. The reference point was marked 3 cm perpendicularly below one-third of the line from the pubic tubercle to the anterior superior iliac spine. The number, distance, and concentration of SILNs were measured relative to the reference point.
Results
The SILNs in the normal group had a mean count of 6.47±1.19, a mean distance from the reference point of 21.10±9.66 mm, and a mean concentration of 84%. The patient group had a mean lymph node count of 7.68±1.63, a mean distance of 22.48±9.51 mm, and a mean concentration of 77%. The normal and patient groups had significantly different mean lymph node counts (p=0.01). The mean distance from the reference point (p=0.07) and the mean lymph node concentration (p=0.20) did not differ significantly between groups.
Conclusion
Pelvic CT is a reliable method to evaluate the anatomy of SILNs in detail. A statistically significant difference was found in the number of lymph nodes between the lymphedema patient group and the normal group, but not in their distribution.
Keyword
Figure
Reference
-
References
1. Petrek JA, Heelan MC. Incidence of breast carcinoma-related lymphedema. Cancer. 1998; 83(12 Suppl American):2776–81.2. Warren AG, Brorson H, Borud LJ, Slavin SA. Lymphedema: a comprehensive review. Ann Plast Surg. 2007; 59:464–72.3. Chang DW. Lymphatic reconstruction of the extremities. In : Neligan PC, Song DH, editors. Plastic surgery. Vol. 4:4th ed. Toronto, ON: Elsevier Canada;2018. p. 83–92.4. Becker C, Vasile JV, Levine JL, et al. Microlymphatic surgery for the treatment of iatrogenic lymphedema. Clin Plast Surg. 2012; 39:385–98.5. Dayan JH, Dayan E, Kagen A, et al. The use of magnetic resonance angiography in vascularized groin lymph node transfer: an anatomic study. J Reconstr Microsurg. 2014; 30:41–5.6. Raghu PK, Danial AC, Babak JM. Pathophysiology of lymphedema. In : Neligan PC, Gurtner GC, editors. Plastic surgery. Vol. 1:4th ed. Toronto, ON: Elsevier Canada;2018. p. 515–28.7. Park SI, Yang EJ, Kim DK, Jeong HJ, Kim GC, Sim YJ. Prevalence and epidemiological factors involved in cellulitis in Korean patients with lymphedema. Ann Rehabil Med. 2016; 40:326–33.8. Bontumasi N, Jacobson JA, Caoili E, Brandon C, Kim SM, Jamadar D. Inguinal lymph nodes: size, number, and other characteristics in asymptomatic patients by CT. Surg Radiol Anat. 2014; 36:1051–5.9. Shinaoka A, Koshimune S, Suami H, et al. Lower-limb lymphatic drainage pathways and lymph nodes: a CT lymphangiography cadaver study. Radiology. 2020; 294:223–9.10. Vignes S, Blanchard M, Yannoutsos A, Arrault M. Complications of autologous lymph-node transplantation for limb lymphoedema. Eur J Vasc Endovasc Surg. 2013; 45:516–20.11. Pons G, Abdelfattah U, Sarria J, Duch J, Masia J. Reverse lymph node mapping using indocyanine green lymphography: a step forward in minimizing donor-site morbidity in vascularized lymph node transfer. Plast Reconstr Surg. 2021; 147:207e–212e.12. Demiri E, Dionyssiou D, Tsimponis A, et al. Donor-site lymphedema following lymph node transfer for breast cancer-related lymphedema: a systematic review of the literature. Lymphat Res Biol. 2018; 16:2–8.13. Zeltzer AA, Anzarut A, Braeckmans D, et al. The vascularized groin lymph node flap (VGLN): anatomical study and flap planning using multi-detector CT scanner: the golden triangle for flap harvesting. J Surg Oncol. 2017; 116:378–83.14. Scaglioni MF, Suami H. Lymphatic anatomy of the inguinal region in aid of vascularized lymph node flap harvesting. J Plast Reconstr Aesthet Surg. 2015; 68:419–27.15. Lee YH, Kim HK, You HJ, Kim DW. Lymphatic vessels mapping in the lower extremities of a healthy Asian population. Arch Hand Microsurg. 2020; 25:225–31.16. Patel KM, Chu SY, Huang JJ, Wu CW, Lin CY, Cheng MH. Preplanning vascularized lymph node transfer with duplex ultrasonography: an evaluation of 3 donor sites. Plast Reconstr Surg Glob Open. 2014; 2:e193.17. Cheng MH, Chen SC, Henry SL, Tan BK, Chia-Yu Lin M, Huang JJ. Vascularized groin lymph node flap transfer for postmastectomy upper limb lymphedema: flap anatomy, recipient sites, and outcomes. Plast Reconstr Surg. 2013; 131:1286–98.18. Gharb BB, Rampazzo A, Spanio di Spilimbergo S, Xu ES, Chung KP, Chen HC. Vascularized lymph node transfer based on the hilar perforators improves the outcome in upper limb lymphedema. Ann Plast Surg. 2011; 67:589–93.19. Tourani SS, Taylor GI, Ashton MW. Anatomy of the superficial lymphatics of the abdominal wall and the upper thigh and its implications in lymphatic microsurgery. J Plast Reconstr Aesthet Surg. 2013; 66:1390–5.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Evidence-Based Analysis of Lymph Node Transfer in Postmastectomy Upper Extremity Lymphedema
- Indirect Lymphangiography as a diagnostic technique of lymphedema
- Inflammatory Pseudotumor of the Inguinal Lymph Node: A Case Report
- Management of Lymphedema
- Vascularized Free Lymph Node Flap Transfer in Advanced Lymphedema Patient after Axillary Lymph Node Dissection