Ann Surg Treat Res.
2023 Mar;104(3):137-143. 10.4174/astr.2023.104.3.137.
The use of absorbable skin stapler in mastectomy does not increase the rate of surgical site infection
- Affiliations
-
- 1Division of Breast, Department of General Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2539691
- DOI: http://doi.org/10.4174/astr.2023.104.3.137
Abstract
- Purpose
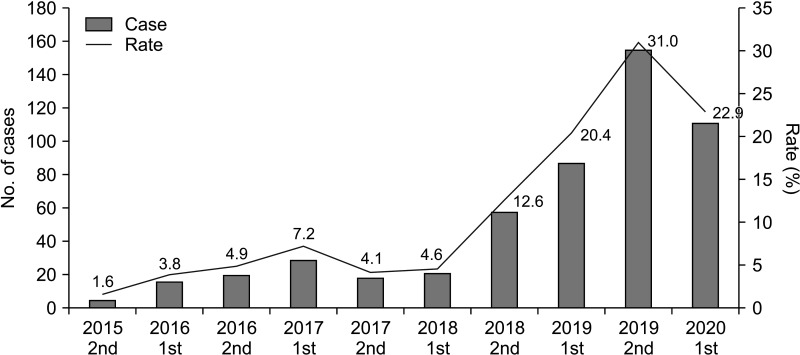
The use of absorbable skin staplers (ASS) for skin closure has been increasing due to their convenience and timesaving effect. In this study, we evaluated the effectiveness of ASS in reducing skin closure time and its safety regarding surgical site infection (SSI), comparing it to conventional hand sewing (HS) in patients who underwent mastectomy.
Methods
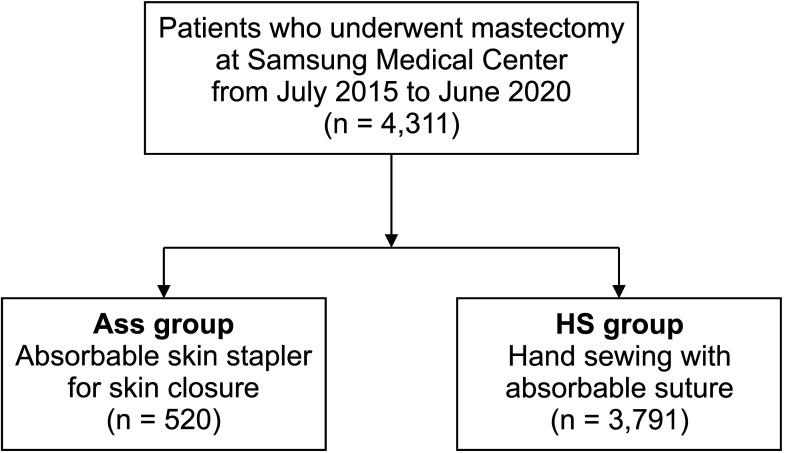
A single-center, retrospective study was conducted. The electronic medical records of patients who underwent mastectomy between July 2015 and June 2020 in Samsung Medical Center were reviewed. The data included previously known risk factors for SSI. We compared the time expended on skin closure and the occurrence rate of SSI between the ASS group and the HS group.
Results
We included 4,311 patients in the analysis. Among them, 520 patients were treated with ASS and 3,791 patients with HS. The average time for skin closure was 16.2 ± 10.1 minutes in the ASS group and 36.5 ± 29.0 minutes in the HS group (P < 0.001). The SSI rate was 0.38% (2 of 520) in the ASS group and 0.36% (14 of 3,791) in the HS group (P > 0.999).
Conclusion
The use of ASS in mastectomy reduced the time for skin closure significantly but did not increase the SSI. Therefore, it can be an effective and safe choice to use ASS instead of HS for skin closure in mastectomy.
Figure
Reference
-
1. KHerman TF, Bordoni B. Wound Classification. StatPearls [Internet]. StatPearls Publishing;2022. updated 2022 Apr 28. cited 2021 Sep 28. Available from: https://www.ncbi.nlm.nih.gov/books/NBK554456/ .2. Kugler NW, Carver TW, Paul JS. Negative pressure therapy is effective in abdominal incision closure. J Surg Res. 2016; 203:491–494. PMID: 27363660.3. CooperSurgical, Inc. The INSORB skin stapler [Internet]. CooperSurgical, Inc.;c2023. cited 2021 May 12. Available from: https://www.insorb.com/insorb-overview/ .4. Patel V, Green JL, Christopher AN, Morris MP, Weiss ES, Broach RB, et al. Use of absorbable dermal stapler in reduction mammoplasty: assessing technical, quality-of-life, and aesthetics outcomes. Plast Reconstr Surg Glob Open. 2021; 9:e3784. PMID: 34476162.5. Nitsche J, Howell C, Howell T. Skin closure with subcuticular absorbable staples after cesarean section is associated with decreased analgesic use. Arch Gynecol Obstet. 2012; 285:979–983. PMID: 22037686.6. Fisher DA, Bengero LL, Clapp BC, Burgess M. A randomized, prospective study of total hip wound closure with resorbable subcuticular staples. Orthopedics. 2010; 33:665. PMID: 20839703.7. Malard O, Duteille F, Darnis E, Espitalier F, Perrot P, Ferron C, et al. A novel absorbable stapler provides patient-reported outcomes and cost-effectiveness noninferior to subcuticular skin closure: a prospective, single-blind, randomized clinical trial. Plast Reconstr Surg. 2020; 146:777e–789e.8. Schrufer-Poland TL, Ruiz MP, Kassar S, Tomassian C, Algren SD, Yeast JD. Incidence of wound complications in cesarean deliveries following closure with absorbable subcuticular staples versus conventional skin closure techniques. Eur J Obstet Gynecol Reprod Biol. 2016; 206:53–56. PMID: 27632411.9. Huotari K. Surveillance of surgical site infections following major hip and knee surgery in Finland. Finland National Public Health Institute;2007.10. Edlich RF, Gubler K, Stevens HS, Wallis AG, Clark JJ, Dahlstrom JJ, et al. Scientific basis for the selection of surgical staples and tissue adhesives for closure of skin wounds. J Environ Pathol Toxicol Oncol. 2010; 29:327–337. PMID: 21284596.11. Duteille F, Rouif M, Alfandari B, Andreoletti JB, Sinna R, Laurent B, et al. Reduction of skin closure time without loss of healing quality: a multicenter prospective study in 100 patients comparing the use of Insorb absorbable staples with absorbable thread for dermal suture. Surg Innov. 2013; 20:70–73. PMID: 22589018.12. Bron T, Zakine G. Placement of absorbable dermal staples in mammaplasty and abdominoplasty: a 12-month prospective study of 60 patients. Aesthet Surg J. 2016; 36:459–468. PMID: 26530478.13. Cross KJ, Teo EH, Wong SL, Lambe JS, Rohde CH, Grant RT, et al. The absorbable dermal staple device: a faster, more cost-effective method for incisional closure. Plast Reconstr Surg. 2009; 124:156–162. PMID: 19568054.14. Gu A, Wei C, Chen AZ, Malahias MA, Fassihi SC, Ast MP, et al. Operative time greater than 120 minutes is associated with increased pulmonary and thromboembolic complications following revision total hip arthroplasty. Eur J Orthop Surg Traumatol. 2020; 30:1393–1400. PMID: 32524203.15. Scott CF Jr. Length of operation and morbidity: is there a relationships? Plast Reconstr Surg. 1982; 69:1017–1021. PMID: 7079394.16. Harris M, Chung F. Complications of general anesthesia. Clin Plast Surg. 2013; 40:503–513. PMID: 24093647.17. Singh S, Swarer K, Resnick K. Longer operative time is associated with increased post-operative complications in patients undergoing minimally-invasive surgery for endometrial cancer. Gynecol Oncol. 2017; 147:554–557. PMID: 28982521.18. Cregar WM, Goodloe JB, Lu Y, Gerlinger TL. Increased operative time impacts rates of short-term complications after unicompartmental knee arthroplasty. J Arthroplasty. 2021; 36:488–494. PMID: 32921548.19. Allan J, Goltsman D, Moradi P, Ascherman JA. The effect of operative time on complication profile and length of hospital stay in autologous and implant-based breast reconstruction patients: an analysis of the 2007-2012 ACS-NSQIP database. J Plast Reconstr Aesthet Surg. 2020; 73:1292–1298. PMID: 32201323.20. Brady JS, Desai SV, Crippen MM, Eloy JA, Gubenko Y, Baredes S, et al. Association of anesthesia duration with complications after microvascular reconstruction of the head and neck. JAMA Facial Plast Surg. 2018; 20:188–195. PMID: 28983575.21. Surace P, Sultan AA, George J, Samuel LT, Khlopas A, Molloy RM, et al. The association between operative time and short-term complications in total hip arthroplasty: an analysis of 89,802 surgeries. J Arthroplasty. 2019; 34:426–432. PMID: 30528133.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Use of Absorbable Surgical Mesh after Partial Mastectomy for Improving the Cosmetic Outcome
- Surgical skin adhesive bond is safe and feasible wound closure method to reduce surgical site infection following minimally invasive colorectal cancer surgery
- Absorbable Plate-Related Infection after Facial Bone Fracture Reduction
- Retrospective study of superficial wound complication comparison between monofilament absorbable versus monofilament nonabsorbable sutures for skin closure in kidney transplant
- A randomized controlled trial comparing liquid skin adhesives and staplers for surgical wound management