J Korean Med Sci.
2023 Feb;38(6):e42. 10.3346/jkms.2023.38.e42.
Association Between Receipt of General Anesthesia During Childhood and Attention Deficit Hyperactive Disorder and Neurodevelopment
- Affiliations
-
- 1Department of Pediatrics, CHA Gangnam Medical Center, CHA University School of Medicine, Seoul, Korea
- 2Department of Computer Science and Engineering, Sungkyunkwan University, Suwon, Korea
- 3Department of Precision Medicine, Sungkyunkwan University School of Medicine, Suwon, Korea
- 4Department of Pediatrics, Hallym University Kangnam Sacred Heart Hospital, Seoul, Korea
- 5Department of Pediatrics, Hallym University Kangdong Sacred Heart Hospital, Seoul, Korea
- 6Department of Pediatrics, CHA Bundang Medical Center, CHA University School of Medicine, Seongnam, Korea
- KMID: 2539491
- DOI: http://doi.org/10.3346/jkms.2023.38.e42
Abstract
- Background
There are inconsistent reports regarding the association between general anesthesia and adverse neurodevelopmental and behavioral disorders in children.
Methods
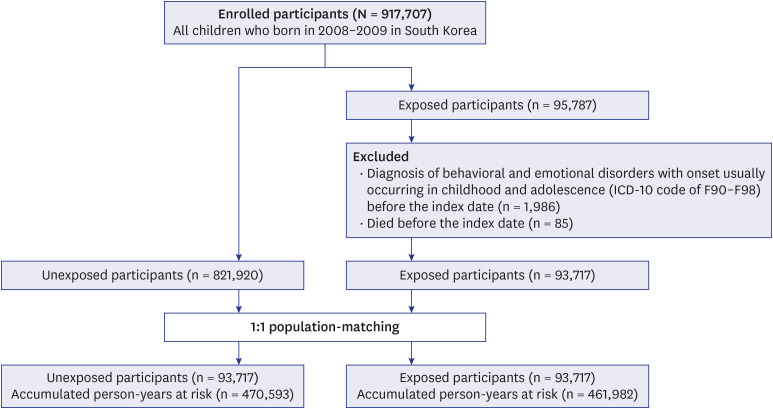
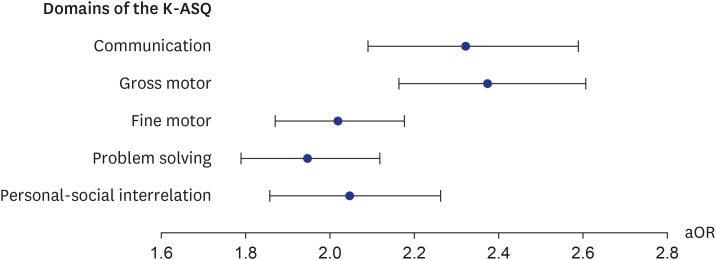
This nationwide administrative cohort study included children born in Korea between 2008 and 2009, and followed until December 31, 2017. The cohort included 93,717 participants who received general anesthesia with endotracheal intubation (ETI) who were matched to unexposed subjects in a 1:1 ratio. General anesthesia was defined by National Health Insurance Service treatment codes with intratracheal anesthesia, and the index date was the first event of general anesthesia. The primary outcome was attention deficit hyperactive disorder (ADHD), which was defined as at least a principal diagnosis of 10th revision of the International Classification of Diseases code F90.X after the age of 72 months. Neurodevelopment, which was assessed using a developmental screening test (Korean-Ages and Stages Questionnaire [K-ASQ]), was a secondary outcome. The K-ASQ is performed annually from 1 to 6 years of age and consists of 5 domains. The association between general anesthesia and ADHD was estimated using a Cox hazard model, and its association with neurodevelopment was estimated using a generalized estimation equation, with control for multiple risk factors beyond 1 year after the index date.
Results
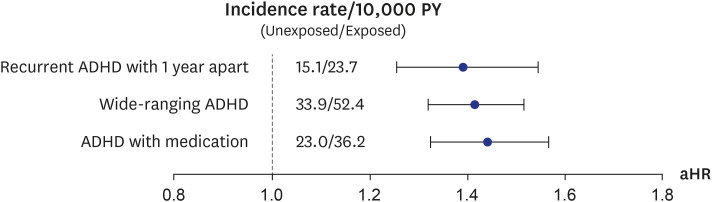
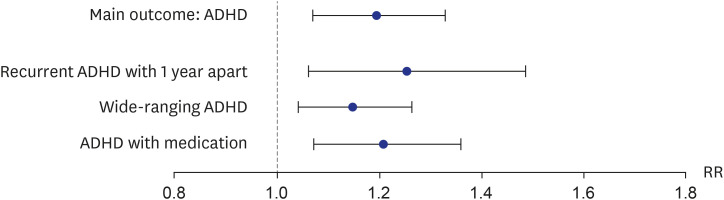
The median age at the index date was 3.8 (95% confidence interval [CI], 1.7–5.8) years, and there were 57,625 (61.5%) men. During a mean follow-up period of 5 years, the incidence rate of ADHD was 42.6 and 27.7 per 10,000 person-years (PY) in the exposed and unexposed groups, respectively (absolute rate difference 14.9 [95% CI, 12.5–17.3] per 10,000 PY). Compared to the unexposed group, the exposed group had an increased risk of ADHD (adjusted hazard ratio, 1.41 [95% CI, 1.30–1.52]). In addition, a longer duration of anesthesia with ETI and more general anesthesia procedures with ETI were associated with greater risk of ADHD. General anesthesia with ETI was also associated with poorer results in the K-ASQ.
Conclusion
Administration of general anesthesia with ETI to children is associated with an increased risk of ADHD and poor results in a neurodevelopmental screening test.
Figure
Reference
-
1. U.S. Food and Drug Administration. FDA Drug Safety Communication: FDA Review Results in New Warnings About Using General Anesthetics and Sedation Drugs in Young Children and Pregnant Women. Silver Spring, MD, USA: U.S. Food and Drug Administration;2017.2. Shi Y, Hu D, Rodgers EL, Katusic SK, Gleich SJ, Hanson AC, et al. Epidemiology of general anesthesia prior to age 3 in a population-based birth cohort. Paediatr Anaesth. 2018; 28(6):513–519. PMID: 29532559.
Article3. Walkden GJ, Gill H, Davies NM, Peters AE, Wright I, Pickering AE. Early childhood general anesthesia and neurodevelopmental outcomes in the Avon Longitudinal Study of parents and children birth cohort. Anesthesiology. 2020; 133(5):1007–1020. PMID: 32898216.
Article4. Korean Statistical Information Service. KOSIS statistical database. Updated 2022. Accessed August 10th, 2022. https://kosis.kr/eng/ .5. Sanders RD, Hassell J, Davidson AJ, Robertson NJ, Ma D. Impact of anaesthetics and surgery on neurodevelopment: an update. Br J Anaesth. 2013; 110(Suppl 1):Suppl 1. i53–i72. PMID: 23542078.
Article6. Walters JL, Paule MG. Review of preclinical studies on pediatric general anesthesia-induced developmental neurotoxicity. Neurotoxicol Teratol. 2017; 60:2–23. PMID: 27871903.
Article7. Andersen SL. Trajectories of brain development: point of vulnerability or window of opportunity? Neurosci Biobehav Rev. 2003; 27(1-2):3–18. PMID: 12732219.
Article8. Lin EP, Lee JR, Lee CS, Deng M, Loepke AW. Do anesthetics harm the developing human brain? An integrative analysis of animal and human studies. Neurotoxicol Teratol. 2017; 60:117–128. PMID: 27793659.
Article9. McCann ME, de Graaff JC, Dorris L, Disma N, Withington D, Bell G, et al. Neurodevelopmental outcome at 5 years of age after general anaesthesia or awake-regional anaesthesia in infancy (GAS): an international, multicentre, randomised, controlled equivalence trial. Lancet. 2019; 393(10172):664–677. PMID: 30782342.10. Warner DO, Zaccariello MJ, Katusic SK, Schroeder DR, Hanson AC, Schulte PJ, et al. Neuropsychological and behavioral outcomes after exposure of young children to procedures requiring general anesthesia: the Mayo Anesthesia Safety in Kids (MASK) study. Anesthesiology. 2018; 129(1):89–105. PMID: 29672337.
Article11. Hu D, Flick RP, Zaccariello MJ, Colligan RC, Katusic SK, Schroeder DR, et al. Association between exposure of young children to procedures requiring general anesthesia and learning and behavioral outcomes in a population-based birth cohort. Anesthesiology. 2017; 127(2):227–240. PMID: 28609302.
Article12. Kim JH, Lee JE, Shim SM, Ha EK, Yon DK, Kim OH, et al. Cohort profile: national investigation of birth cohort in Korea study 2008 (NICKs-2008). Clin Exp Pediatr. 2021; 64(9):480–488. PMID: 33445832.
Article13. Gruschow SM, Yerys BE, Power TJ, Durbin DR, Curry AE. Validation of the use of electronic health records for classification of ADHD status. J Atten Disord. 2016; 23(13):1647–1655. PMID: 28112025.
Article14. Shi Y, Dykhoff HJ, Guevara LR, Sangaralingham LR, Schroeder DR, Flick RP, et al. Moderators of the association between attention-deficit/hyperactivity disorder and exposure to anaesthesia and surgery in children. Br J Anaesth. 2021; 127(5):722–728. PMID: 34503832.
Article15. Tsai CJ, Lee CT, Liang SH, Tsai PJ, Chen VC, Gossop M. Risk of ADHD after multiple exposures to general anesthesia: a nationwide retrospective cohort study. J Atten Disord. 2018; 22(3):229–239. PMID: 26023173.
Article16. Ko WR, Liaw YP, Huang JY, Zhao DH, Chang HC, Ko PC, et al. Exposure to general anesthesia in early life and the risk of attention deficit/hyperactivity disorder development: a nationwide, retrospective matched-cohort study. Paediatr Anaesth. 2014; 24(7):741–748. PMID: 24612161.
Article17. Grabowski J, Goldin A, Arthur LG, Beres AL, Guner YS, Hu YY, et al. The effects of early anesthesia on neurodevelopment: a systematic review. J Pediatr Surg. 2021; 56(5):851–861. PMID: 33509654.
Article18. Davidson AJ, Disma N, de Graaff JC, Withington DE, Dorris L, Bell G, et al. Neurodevelopmental outcome at 2 years of age after general anaesthesia and awake-regional anaesthesia in infancy (GAS): an international multicentre, randomised controlled trial. Lancet. 2016; 387(10015):239–250. PMID: 26507180.
Article19. McCann ME, Soriano SG. Does general anesthesia affect neurodevelopment in infants and children? BMJ. 2019; 367:l6459. PMID: 31818811.
Article20. Briner A, De Roo M, Dayer A, Muller D, Habre W, Vutskits L. Volatile anesthetics rapidly increase dendritic spine density in the rat medial prefrontal cortex during synaptogenesis. Anesthesiology. 2010; 112(3):546–556. PMID: 20124985.
Article21. Vutskits L. General anesthesia: a gateway to modulate synapse formation and neural plasticity? Anesth Analg. 2012; 115(5):1174–1182. PMID: 22859689.22. Zhang LL, Pathak HR, Coulter DA, Freed MA, Vardi N. Shift of intracellular chloride concentration in ganglion and amacrine cells of developing mouse retina. J Neurophysiol. 2006; 95(4):2404–2416. PMID: 16371454.
Article23. Edwards DA, Shah HP, Cao W, Gravenstein N, Seubert CN, Martynyuk AE. Bumetanide alleviates epileptogenic and neurotoxic effects of sevoflurane in neonatal rat brain. Anesthesiology. 2010; 112(3):567–575. PMID: 20124973.
Article24. Dalla Massara L, Osuru HP, Oklopcic A, Milanovic D, Joksimovic SM, Caputo V, et al. General anesthesia causes epigenetic histone modulation of c-Fos and brain-derived neurotrophic factor, target genes important for neuronal development in the immature rat hippocampus. Anesthesiology. 2016; 124(6):1311–1327. PMID: 27028464.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case Report of a Child who has Attention Deficit Hyperactivity Disorder, Mental Retardation, and Mania
- Association between the Brain-Derived Neurotropic Factor and Attention Deficit Hyperactivity Disorder
- OROS Methylphenidate Treatment of Secondary Adult ADHD after Traumatic Brain Injury
- Childhood Attention Deficit in the Patients with Bipolar Disorder and CHRNA7 Gene Polymorphisms
- Factors related to Medication Adherence according to Severity of Attention Deficit Hyperactivity Disorder in Children