Diabetes Metab J.
2023 Jan;47(1):118-134. 10.4093/dmj.2022.0007.
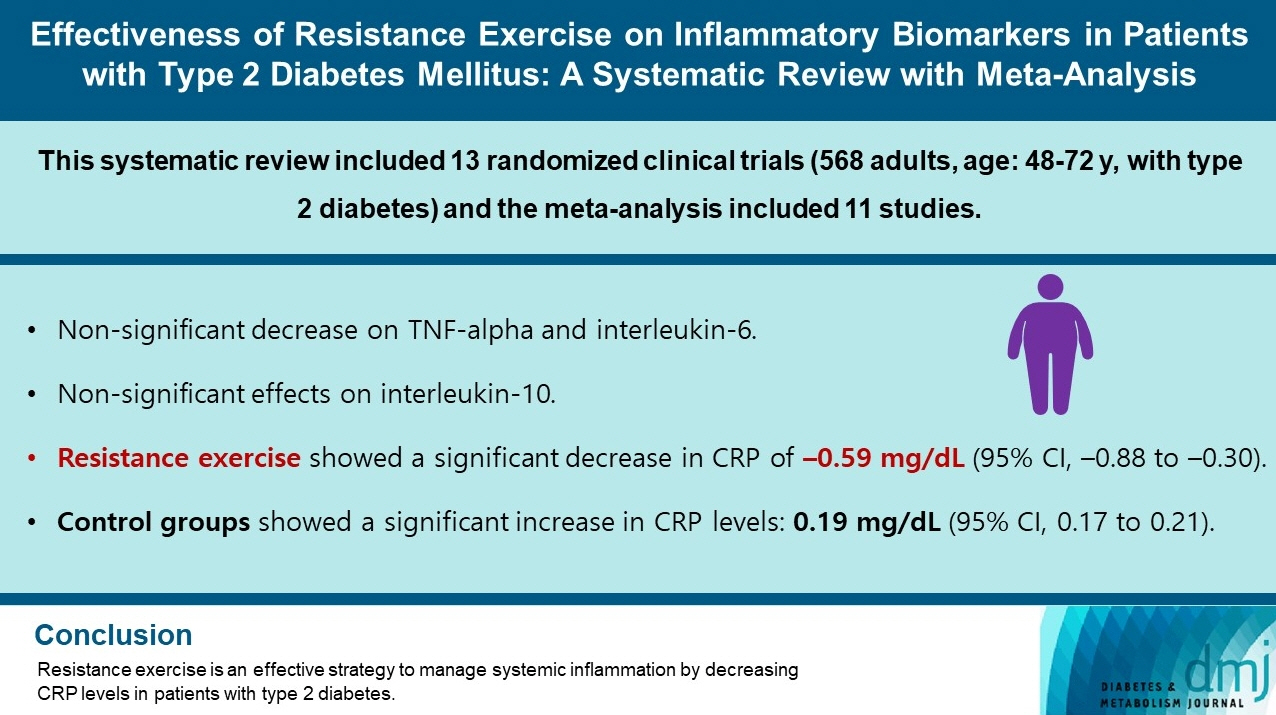
Effectiveness of Resistance Exercise on Inflammatory Biomarkers in Patients with Type 2 Diabetes Mellitus: A Systematic Review with Meta-Analysis
- Affiliations
-
- 1University of Castilla-La Mancha, Health and Social Research Center, Cuenca, Spain
- 2University of the Republic, Higher Institute of Physical Education, Rivera, Uruguay
- 3University of Castilla-La Mancha, Faculty of Nursing, Albacete, Spain
- 4State University of Londrina, Health Science Center, Londrina, Brazil
- 5University Autonomous of Chile, Faculty of Health Sciences, Talca, Chile
- KMID: 2538936
- DOI: http://doi.org/10.4093/dmj.2022.0007
Abstract
- Background
Type 2 diabetes mellitus (T2DM) is related to increased inflammatory processes. The effects of resistance exercise on inflammatory biomarkers in T2DM are controversial. Our purpose was to determine the effectiveness of resistance exercise on inflammatory biomarkers in patients diagnosed with T2DM.
Methods
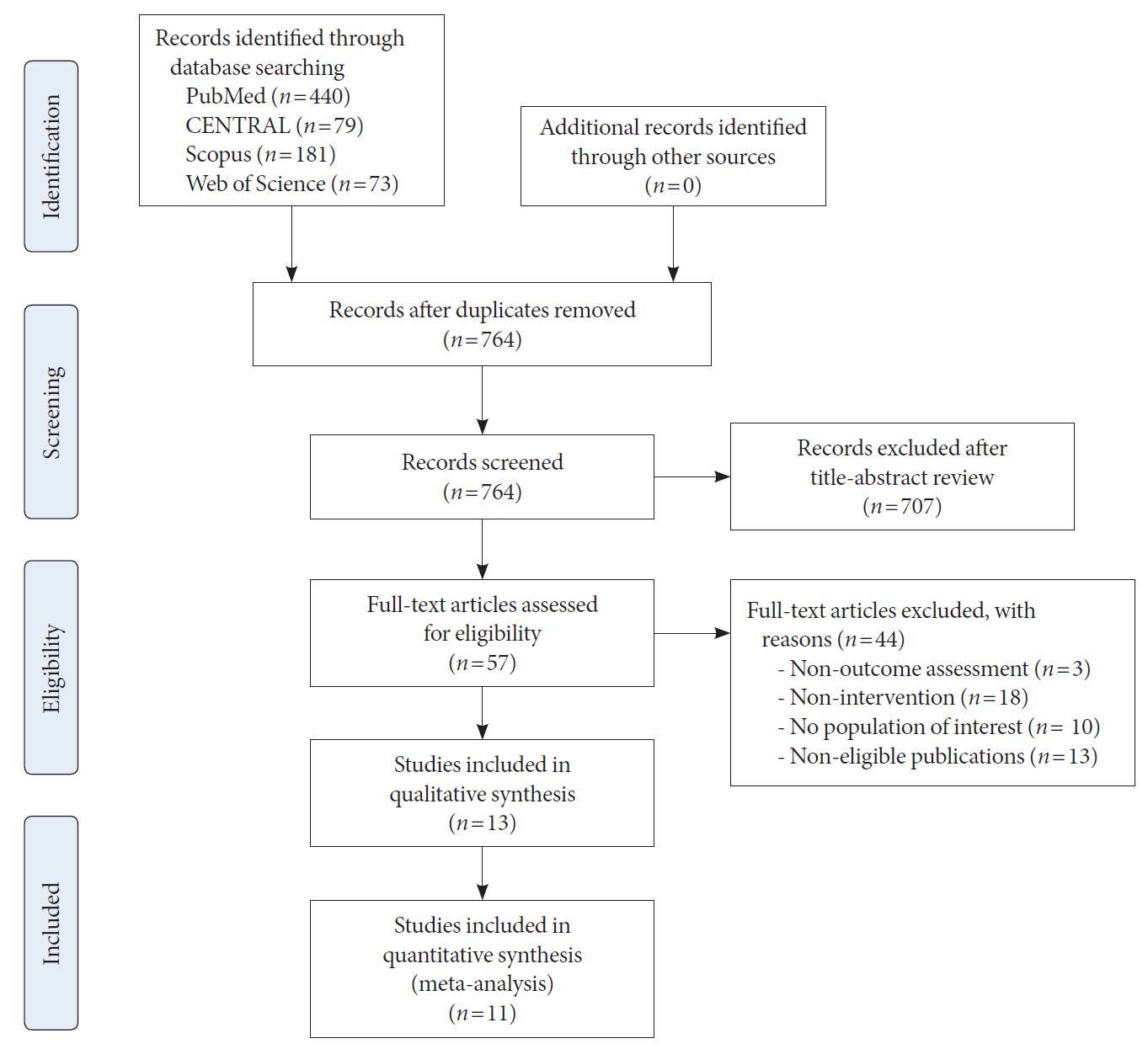
We searched four databases until September 2021. We included randomized clinical trials (RCTs) of the effects of resistance exercise on inflammatory biomarkers (C-reactive protein [CRP], tumor necrosis factor alpha, interleukin-6, and interleukin-10) in patients with T2DM. A random effects meta-analysis was conducted to determine the standardized mean difference (SMD) and the raw mean difference (MD) for CRP.
Results
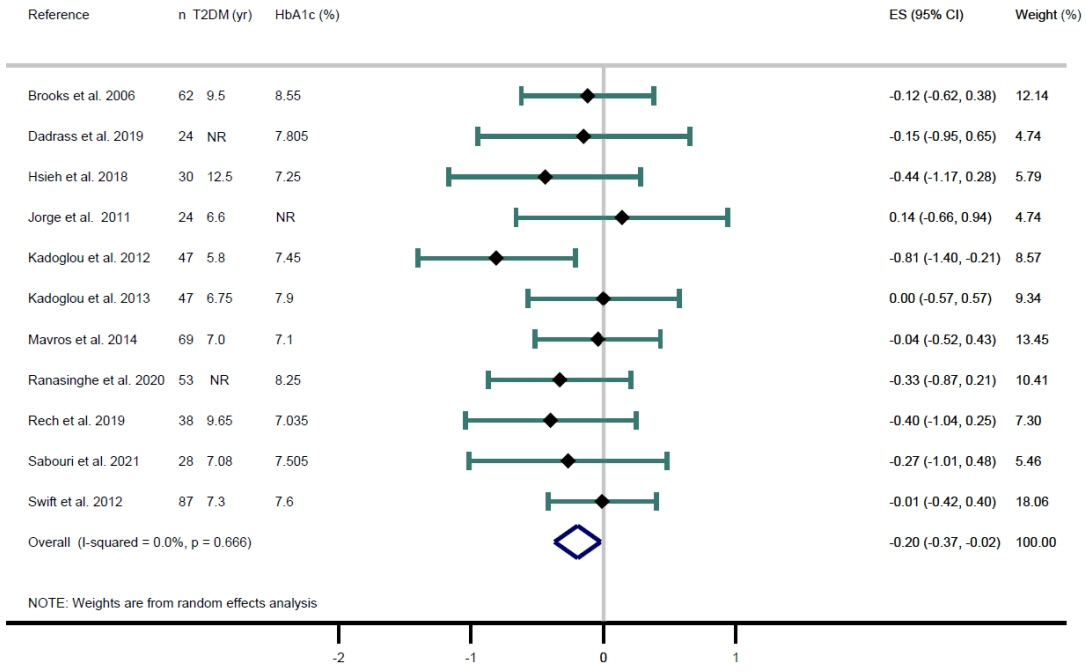
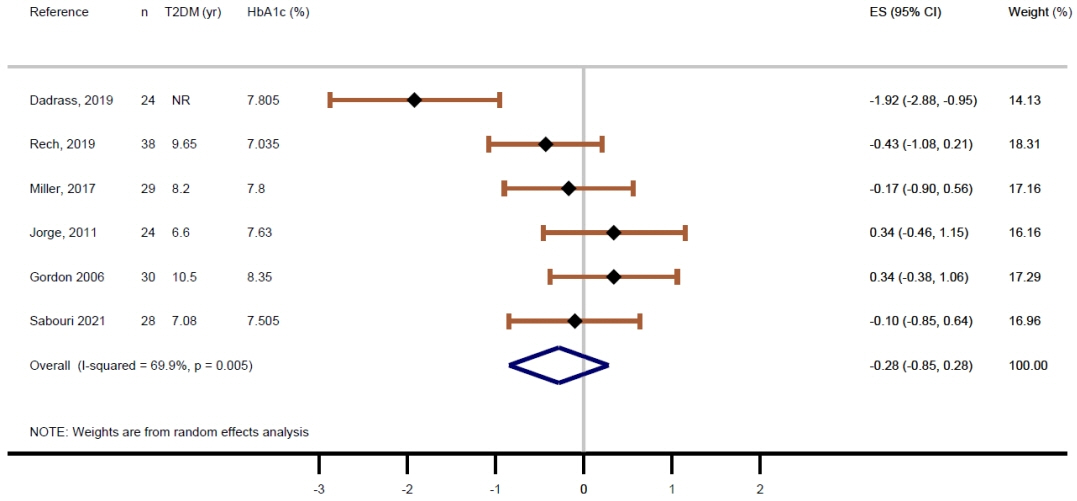
Thirteen RCTs were included in the review, and 11 in the meta-analysis for CRP. Lower CRP levels were observed when resistance exercise was compared with the control groups (SMD=–0.20; 95% confidence interval [CI], –0.37 to –0.02). When conducting the MD meta-analysis, resistance exercise showed a significant decrease in CRP of –0.59 mg/dL (95% CI, –0.88 to –0.30); otherwise, in the control groups, the CRP values increased 0.19 mg/dL (95% CI, 0.17 to 0.21).
Conclusion
Evidence supports resistance exercise as an effective strategy to manage systemic inflammation by decreasing CRP levels in patients with T2DM. The evidence is still inconclusive for other inflammatory biomarkers.
Keyword
Figure
Reference
-
1. Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res Clin Pract. 2019; 157:107843.
Article2. Teixeira-Lemos E, Nunes S, Teixeira F, Reis F. Regular physical exercise training assists in preventing type 2 diabetes development: focus on its antioxidant and anti-inflammatory properties. Cardiovasc Diabetol. 2011; 10:12.
Article3. Berbudi A, Rahmadika N, Tjahjadi AI, Ruslami R. Type 2 diabetes and its impact on the immune system. Curr Diabetes Rev. 2020; 16:442–9.
Article4. Calle MC, Fernandez ML. Inflammation and type 2 diabetes. Diabetes Metab. 2012; 38:183–91.
Article5. King GL. The role of inflammatory cytokines in diabetes and its complications. J Periodontol. 2008; 79(8 Suppl):1527–34.
Article6. Neeland IJ, Turer AT, Ayers CR, Powell-Wiley TM, Vega GL, Farzaneh-Far R, et al. Dysfunctional adiposity and the risk of prediabetes and type 2 diabetes in obese adults. JAMA. 2012; 308:1150–9.
Article7. Trayhurn P, Wood IS. Signalling role of adipose tissue: adipokines and inflammation in obesity. Biochem Soc Trans. 2005; 33(Pt 5):1078–81.
Article8. Balducci S, Sacchetti M, Haxhi J, Orlando G, D’Errico V, Fallucca S, et al. Physical exercise as therapy for type 2 diabetes mellitus. Diabetes Metab Res Rev. 2014; 30 Suppl 1:13–23.
Article9. Melo LC, Dativo-Medeiros J, Menezes-Silva CE, Barbosa FT, de Sousa-Rodrigues CF, Rabelo LA. Physical exercise on inflammatory markers in type 2 diabetes patients: a systematic review of randomized controlled trials. Oxid Med Cell Longev. 2017; 2017:8523728.
Article10. Chen X, Sun X, Wang C, He H. Effects of exercise on inflammatory cytokines in patients with type 2 diabetes: a meta-analysis of randomized controlled trials. Oxid Med Cell Longev. 2020; 2020:6660557.
Article11. Acosta-Manzano P, Rodriguez-Ayllon M, Acosta FM, Niederseer D, Niebauer J. Beyond general resistance training. Hypertrophy versus muscular endurance training as therapeutic interventions in adults with type 2 diabetes mellitus: a systematic review and meta-analysis. Obes Rev. 2020; 21:e13007.
Article12. Maestroni L, Read P, Bishop C, Papadopoulos K, Suchomel TJ, Comfort P, et al. The benefits of strength training on musculoskeletal system health: practical applications for interdisciplinary care. Sports Med. 2020; 50:1431–50.
Article13. Andersen H, Nielsen S, Mogensen CE, Jakobsen J. Muscle strength in type 2 diabetes. Diabetes. 2004; 53:1543–8.
Article14. Celis-Morales CA, Petermann F, Hui L, Lyall DM, Iliodromiti S, McLaren J, et al. Associations between diabetes and both cardiovascular disease and all-cause mortality are modified by grip strength: evidence from UK Biobank, a prospective population-based cohort study. Diabetes Care. 2017; 40:1710–8.
Article15. American Diabetes Association. 5. Facilitating behavior change and well-being to improve health outcomes: standards of medical care in diabetes-2021. Diabetes Care. 2021; 44(Suppl 1):S53–72.16. Hayashino Y, Jackson JL, Hirata T, Fukumori N, Nakamura F, Fukuhara S, et al. Effects of exercise on C-reactive protein, inflammatory cytokine and adipokine in patients with type 2 diabetes: a meta-analysis of randomized controlled trials. Metabolism. 2014; 63:431–40.
Article17. Higgins J, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (Updated March 2011). Available from: https://handbook-5-1.cochrane.org (cited 2022 Mar 23).18. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021; 372:n71.19. Sterne JAC, Savovic J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019; 366:l4898.
Article20. Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011; 64:383–94.
Article21. DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986; 7:177–88.
Article22. Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002; 21:1539–58.
Article23. Page MJ, Sterne J, Higgins J, Egger M. Investigating and dealing with publication bias and other reporting biases in meta-analyses of health research: a review. Res Synth Methods. 2021; 12:248–59.
Article24. Gordon PL, Vannier E, Hamada K, Layne J, Hurley BF, Roubenoff R, et al. Resistance training alters cytokine gene expression in skeletal muscle of adults with type 2 diabetes. Int J Immunopathol Pharmacol. 2006; 19:739–49.
Article25. Brooks N, Layne JE, Gordon PL, Roubenoff R, Nelson ME, Castaneda-Sceppa C. Strength training improves muscle quality and insulin sensitivity in Hispanic older adults with type 2 diabetes. Int J Med Sci. 2006; 4:19–27.
Article26. Rech A, Botton CE, Lopez P, Quincozes-Santos A, Umpierre D, Pinto RS. Effects of short-term resistance training on endothelial function and inflammation markers in elderly patients with type 2 diabetes: a randomized controlled trial. Exp Gerontol. 2019; 118:19–25.
Article27. Ranasinghe C, Devage S, Constantine GR, Katulanda P, Hills AP, King NA. Glycemic and cardiometabolic effects of exercise in South Asian Sri Lankans with type 2 diabetes mellitus: a randomized controlled trial Sri Lanka diabetes aerobic and resistance training study (SL-DARTS). Diabetes Metab Syndr. 2021; 15:77–85.
Article28. Sabouri M, Hatami E, Pournemati P, Shabkhiz F. Inflammatory, antioxidant and glycemic status to different mode of high-intensity training in type 2 diabetes mellitus. Mol Biol Rep. 2021; 48:5291–304.
Article29. Jorge ML, de Oliveira VN, Resende NM, Paraiso LF, Calixto A, Diniz AL, et al. The effects of aerobic, resistance, and combined exercise on metabolic control, inflammatory markers, adipocytokines, and muscle insulin signaling in patients with type 2 diabetes mellitus. Metabolism. 2011; 60:1244–52.
Article30. Kadoglou NP, Fotiadis G, Athanasiadou Z, Vitta I, Lampropoulos S, Vrabas IS. The effects of resistance training on ApoB/ ApoA-I ratio, Lp(a) and inflammatory markers in patients with type 2 diabetes. Endocrine. 2012; 42:561–9.
Article31. Swift DL, Johannsen NM, Earnest CP, Blair SN, Church TS. Effect of exercise training modality on C-reactive protein in type 2 diabetes. Med Sci Sports Exerc. 2012; 44:1028–34.
Article32. Kadoglou NP, Fotiadis G, Kapelouzou A, Kostakis A, Liapis CD, Vrabas IS. The differential anti-inflammatory effects of exercise modalities and their association with early carotid atherosclerosis progression in patients with type 2 diabetes. Diabet Med. 2013; 30:e41–50.33. Mavros Y, Kay S, Simpson KA, Baker MK, Wang Y, Zhao RR, et al. Reductions in C-reactive protein in older adults with type 2 diabetes are related to improvements in body composition following a randomized controlled trial of resistance training. J Cachexia Sarcopenia Muscle. 2014; 5:111–20.
Article34. Hsieh PL, Tseng CH, Tseng YJ, Yang WS. Resistance training improves muscle function and cardiometabolic risks but not quality of life in older people with type 2 diabetes mellitus: a randomized controlled trial. J Geriatr Phys Ther. 2018; 41:65–76.
Article35. Miller EG, Sethi P, Nowson CA, Dunstan DW, Daly RM. Effects of progressive resistance training and weight loss versus weight loss alone on inflammatory and endothelial biomarkers in older adults with type 2 diabetes. Eur J Appl Physiol. 2017; 117:1669–78.
Article36. Dadrass A, Mohamadzadeh Salamat K, Hamidi K, Azizbeigi K. Anti-inflammatory effects of vitamin D and resistance training in men with type 2 diabetes mellitus and vitamin D deficiency: a randomized, double-blinded, placebo-controlled clinical trial. J Diabetes Metab Disord. 2019; 18:323–31.
Article37. Melo LC, Dativo-Medeiros J, Menezes-Silva CE, Barbosa FT, de Sousa-Rodrigues CF, Rabelo LA. Physical exercise on inflammatory markers in type 2 diabetes patients: a systematic review of randomized controlled trials. Oxid Med Cell Longev. 2017; 2017:8523728.
Article38. Cronin O, Keohane DM, Molloy MG, Shanahan F. The effect of exercise interventions on inflammatory biomarkers in healthy, physically inactive subjects: a systematic review. QJM. 2017; 110:629–37.
Article39. Coelho DB, Lopes L, de Oliveira EC, Becker LK, de Paula Costa G, Hermsdorff H, et al. Baseline diet quality is related to changes in the body composition and inflammatory markers: an intervention study based on resistance training and nutritional advice. Biomed Res Int. 2021; 2021:6681823.
Article40. Hariharan R, Odjidja EN, Scott D, Shivappa N, Hebert JR, Hodge A, et al. The dietary inflammatory index, obesity, type 2 diabetes, and cardiovascular risk factors and diseases. Obes Rev. 2022; 23:e13349.
Article41. Wawrzyniak-Gramacka E, Hertmanowska N, Tylutka A, Morawin B, Wacka E, Gutowicz M, et al. The association of anti-inflammatory diet ingredients and lifestyle exercise with inflammaging. Nutrients. 2021; 13:3696.
Article42. Anusruti A, Xuan Y, Gao X, Jansen E, Laetsch DC, Brenner H, et al. Factors associated with high oxidative stress in patients with type 2 diabetes: a meta-analysis of two cohort studies. BMJ Open Diabetes Res Care. 2020; 8:e000933.
Article43. Tahrani AA, Barnett AH, Bailey CJ. Pharmacology and therapeutic implications of current drugs for type 2 diabetes mellitus. Nat Rev Endocrinol. 2016; 12:566–92.
Article44. Chen CN, Chen TC, Tsai SC, Hwu CM. Factors associated with relative muscle strength in patients with type 2 diabetes mellitus. Arch Gerontol Geriatr. 2021; 95:104384.
Article45. You T, Arsenis NC, Disanzo BL, Lamonte MJ. Effects of exercise training on chronic inflammation in obesity: current evidence and potential mechanisms. Sports Med. 2013; 43:243–56.
Article46. Gippini A, Mato A, Pazos R, Suarez B, Vila B, Gayoso P, et al. Effect of long-term strength training on glucose metabolism. Implications for individual impact of high lean mass and high fat mass on relationship between BMI and insulin sensitivity. J Endocrinol Invest. 2002; 25:520–5.
Article47. Richter-Stretton GL, Fenning AS, Vella RK. Skeletal muscle: a bystander or influencer of metabolic syndrome? Diabetes Metab Syndr. 2020; 14:867–75.48. Franceschi C, Campisi J. Chronic inflammation (inflammaging) and its potential contribution to age-associated diseases. J Gerontol A Biol Sci Med Sci. 2014; 69 Suppl 1:S4–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effectiveness of Green Tea or Green Tea Extract on Insulin Resistance and Glycemic Control in Type 2 Diabetes Mellitus: A Meta-Analysis
- A Meta-Analysis of the Effects of Exercise Programs on Glucose and Lipid Metabolism and Cardiac Function in Patients with TypeII Diabetes Mellitus
- Letter: Effects of Aerobic Exercise Intensity on Insulin Resistance in Patients with Type 2 Diabetes Mellitus (Korean Diabetes J 33(5):401-411, 2009)
- Response: Effects of Aerobic Exercise Intensity on Insulin Resistance in Patients with Type 2 Diabetes Mellitus (Korean Diabetes J 33:(5)401-411, 2009)
- The Effect of Regular Exercise on Insulin Sensitivity in Type 2 Diabetes Mellitus: A Systematic Review and Meta-Analysis