Kosin Med J.
2022 Dec;37(4):361-366. 10.7180/kmj.22.027.
Multiple extraintestinal manifestations in a patient with acute severe ulcerative colitis: a case report
- Affiliations
-
- 1Department of Internal Medicine, Pusan National University School of Medicine, Busan, Korea
- 2Division of Gastroenterology, Department of Internal Medicine, Dong-Eui Medical Center, Busan, Korea
- 3Biomedical Research Institute, Pusan National University Hospital, Busan, Korea
- KMID: 2538866
- DOI: http://doi.org/10.7180/kmj.22.027
Abstract
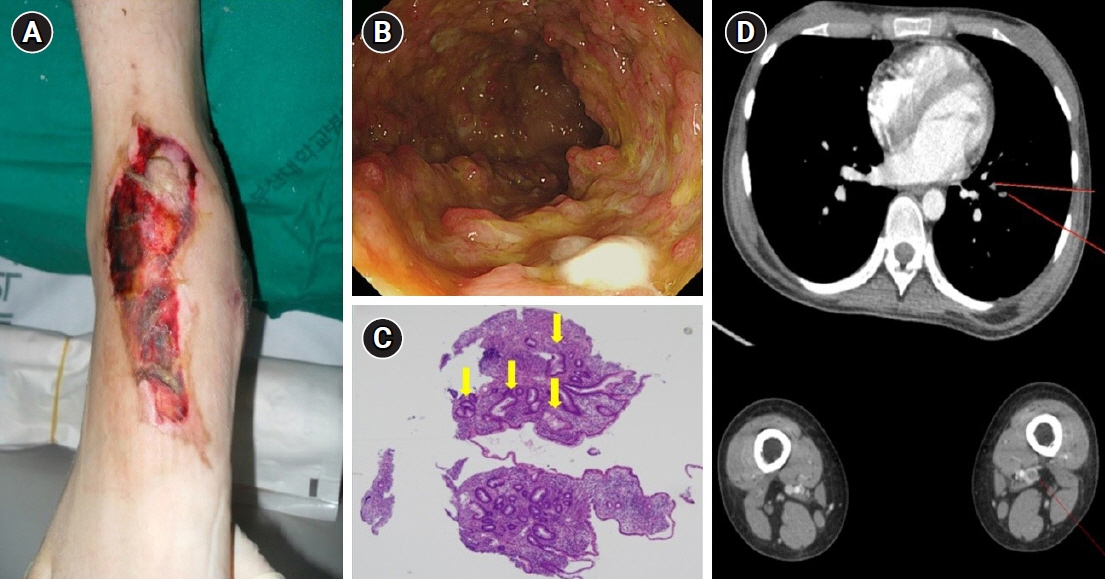
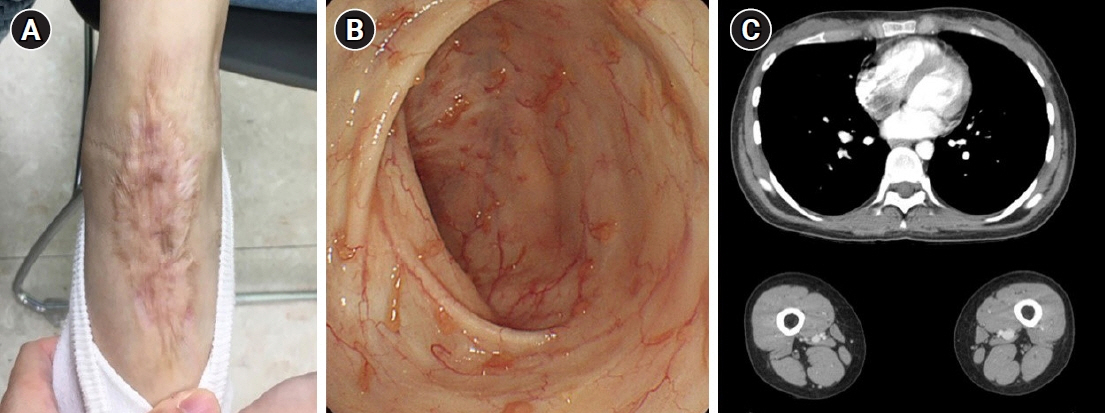
- Patients with inflammatory bowel disease (IBD) are at risk for extraintestinal manifestations (EIM) over the course of their disease. As EIMs can involve nearly every organ, and strongly influence the quality of life, early recognition and adequate treatment are necessary to prevent severe morbidity and mortality in affected patients. Pyoderma gangrenosum is a highly severe and debilitating skin condition that occurs in 1% to 10% of ulcerative colitis (UC) patients. Thromboembolic events are also serious EIMs and usually present as deep vein thromboses in the legs or as pulmonary embolisms. A 19-year-old woman presented with bloody diarrhea lasting for 3 months and deep ulceration on the right foot. She was diagnosed with UC. The patient's skin lesions did not improve with intravenous corticosteroids and oral mesalazine. After she was started on infliximab, we observed rapid resolution of the skin lesions. She continued to complain of mild dyspnea while in the hospital. Computed tomography performed using the thromboembolism protocol revealed pulmonary thromboembolism and deep venous thrombosis. The patient underwent anticoagulant therapy with low-molecular-weight heparin, and her dyspnea gradually improved. Anticoagulation was continued with warfarin. It is rare for IBD patients to have multiple EIMs; however, this case demonstrates that multiple EIMs are a possible presentation in UC and underscores the importance of a meticulous clinical examination and adequate evaluation in the management of IBD patients presenting with EIMs.
Keyword
Figure
Reference
-
References
1. Bernstein CN, Blanchard JF, Rawsthorne P, Yu N. The prevalence of extraintestinal diseases in inflammatory bowel disease: a population-based study. Am J Gastroenterol. 2001; 96:1116–22.
Article2. Lebwohl M, Lebwohl O. Cutaneous manifestations of inflammatory bowel disease. Inflamm Bowel Dis. 1998; 4:142–8.
Article3. Grainge MJ, West J, Card TR. Venous thromboembolism during active disease and remission in inflammatory bowel disease: a cohort study. Lancet. 2010; 375:657–63.
Article4. Aghazadeh R, Zali MR, Bahari A, Amin K, Ghahghaie F, Firouzi F. Inflammatory bowel disease in Iran: a review of 457 cases. J Gastroenterol Hepatol. 2005; 20:1691–5.
Article5. Arivarasan K, Bhardwaj V, Sud S, Sachdeva S, Puri AS. Biologics for the treatment of pyoderma gangrenosum in ulcerative colitis. Intest Res. 2016; 14:365–8.
Article6. Hayashi H, Kuwabara C, Tarumi K, Makino E, Fujimoto W. Successful treatment with infliximab for refractory pyoderma gangrenosum associated with inflammatory bowel disease. J Dermatol. 2012; 39:576–8.
Article7. Vavricka SR, Schoepfer A, Scharl M, Lakatos PL, Navarini A, Rogler G. Extraintestinal manifestations of inflammatory bowel disease. Inflamm Bowel Dis. 2015; 21:1982–92.
Article8. Greuter T, Vavricka SR. Extraintestinal manifestations in inflammatory bowel disease: epidemiology, genetics, and pathogenesis. Expert Rev Gastroenterol Hepatol. 2019; 13:307–17.9. Hedin CR, Vavricka SR, Stagg AJ, Schoepfer A, Raine T, Puig L, et al. The pathogenesis of extraintestinal manifestations: implications for IBD research, diagnosis, and therapy. J Crohns Colitis. 2019; 13:541–54.
Article10. Vavricka SR, Brun L, Ballabeni P, Pittet V, Prinz Vavricka BM, Zeitz J, et al. Frequency and risk factors for extraintestinal manifestations in the Swiss inflammatory bowel disease cohort. Am J Gastroenterol. 2011; 106:110–9.
Article11. Harbord M, Annese V, Vavricka SR, Allez M, Barreiro-de Acosta M, Boberg KM, et al. The first European evidence-based consensus on extra-intestinal manifestations in inflammatory bowel disease. J Crohns Colitis. 2016; 10:239–54.
Article12. Polcz M, Gu J, Florin T. Pyoderma gangrenosum in inflammatory bowel disease: the experience at Mater Health Services’ Adult Hospital 1998-2009. J Crohns Colitis. 2011; 5:148–51.
Article13. Jose FA, Heyman MB. Extraintestinal manifestations of inflammatory bowel disease. J Pediatr Gastroenterol Nutr. 2008; 46:124–33.
Article14. Zezos P, Kouklakis G, Saibil F. Inflammatory bowel disease and thromboembolism. World J Gastroenterol. 2014; 20:13863–78.
Article15. Fumery M, Xiaocang C, Dauchet L, Gower-Rousseau C, Peyrin-Biroulet L, Colombel JF. Thromboembolic events and cardiovascular mortality in inflammatory bowel diseases: a meta-analysis of observational studies. J Crohns Colitis. 2014; 8:469–79.
Article16. Papay P, Miehsler W, Tilg H, Petritsch W, Reinisch W, Mayer A, et al. Clinical presentation of venous thromboembolism in inflammatory bowel disease. J Crohns Colitis. 2013; 7:723–9.
Article17. Bernstein CN, Blanchard JF, Houston DS, Wajda A. The incidence of deep venous thrombosis and pulmonary embolism among patients with inflammatory bowel disease: a population-based cohort study. Thromb Haemost. 2001; 85:430–4.
Article18. Solem CA, Loftus EV, Tremaine WJ, Sandborn WJ. Venous thromboembolism in inflammatory bowel disease. Am J Gastroenterol. 2004; 99:97–101.
Article19. Nguyen GC, Sam J. Rising prevalence of venous thromboembolism and its impact on mortality among hospitalized inflammatory bowel disease patients. Am J Gastroenterol. 2008; 103:2272–80.
Article20. Monsen U, Sorstad J, Hellers G, Johansson C. Extracolonic diagnoses in ulcerative colitis: an epidemiological study. Am J Gastroenterol. 1990; 85:711–6.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Acute Pancreatitis associated with Ulcerative Colitis
- Immune Thrombocytopenic Purpur and Neutropenia Associatedwith Ulcerative Colitis
- A Case of Pyoderma Gangrenosum Associated with Ulcerative Colitis
- A Case of Nonischemic Central Retinal Vein Occlusion Developed in the course of Ulcerative Colits
- A Case of Chronic Ulcerative Colitis Complicated by Budd-Chiari Syndrome and Colon Cancer