Kosin Med J.
2022 Sep;37(3):220-227. 10.7180/kmj.22.107.
Clinical significance of copeptin as an early predictor of renal graft dysfunction in renal transplant recipients
- Affiliations
-
- 1Department of Internal Medicine, Inje University Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea
- KMID: 2538801
- DOI: http://doi.org/10.7180/kmj.22.107
Abstract
- Background
Copeptin is the carboxyl-terminal part of the vasopressin precursor protein, and its concentration is an independent predictor of the onset of chronic kidney disease and a rapid decline in the glomerular filtration rate. The glomerular filtration rate is regarded as the best indicator of kidney transplant function and is a predictor of graft and patient survival. We investigated the clinical significance of copeptin as an early predictor of renal graft dysfunction in renal transplant recipients.
Methods
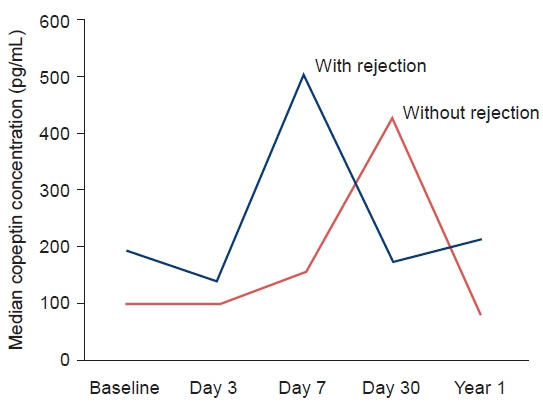
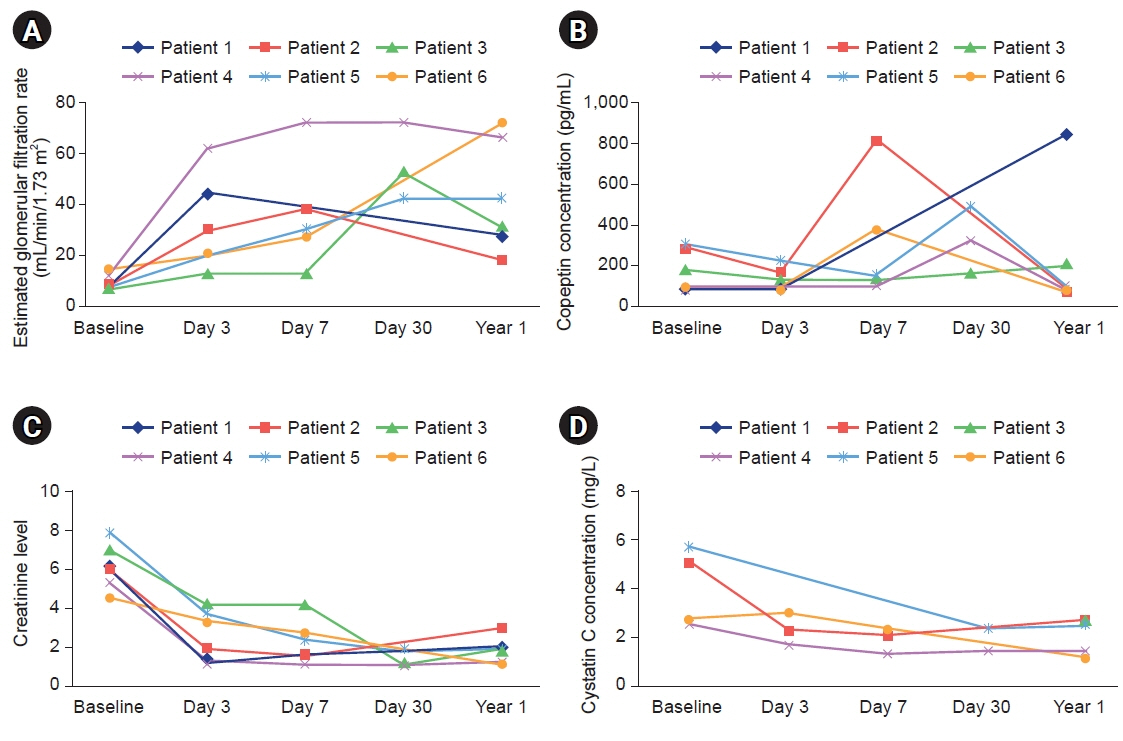
We measured serum creatinine, cystatin C, and copeptin concentrations in renal transplant recipients on the day of their operation, as well as on postoperative days 3, 7, 30, and 365. Acute rejection was defined as a sudden decrease in renal function accompanied by histological changes.
Results
Eight renal transplant recipients were enrolled in the study from July 2018 to December 2019. Four patients experienced histologically confirmed transplant rejection. All four cases involved acute T-cell rejection. No significant correlation was found between the copeptin level and the presence or absence of rejection at any time point. In subgroup analyses, changes in creatinine, the estimated glomerular filtration rate, cystatin, and copeptin did not show statistical significance.
Conclusions
We anticipated that copeptin would be useful to identify individuals at high risk of transplant rejection; however, our study failed to show an association. Further research will be needed to overcome the limitations of this study.
Keyword
Figure
Reference
-
References
1. Holwerda DA. A glycopeptide from the posterior lobe of pig pituitaries. I. Isolation and characterization. Eur J Biochem. 1972; 28:334–9.2. Seidah NG, Benjannet S, Chretien M. The complete sequence of a novel human pituitary glycopeptide homologous to pig posterior pituitary glycopeptide. Biochem Biophys Res Commun. 1981; 100:901–7.3. Bouby N, Hassler C, Bankir L. Contribution of vasopressin to progression of chronic renal failure: study in Brattleboro rats. Life Sci. 1999; 65:991–1004.4. Bardoux P, Bichet DG, Martin H, Gallois Y, Marre M, Arthus MF, et al. Vasopressin increases urinary albumin excretion in rats and humans: involvement of V2 receptors and the renin-angiotensin system. Nephrol Dial Transplant. 2003; 18:497–506.5. Bouby N, Bachmann S, Bichet D, Bankir L. Effect of water intake on the progression of chronic renal failure in the 5/6 nephrectomized rat. Am J Physiol. 1990; 258(4 Pt 2):F973–9.6. Perico N, Zoja C, Corna D, Rottoli D, Gaspari F, Haskell L, et al. V1/V2 Vasopressin receptor antagonism potentiates the renoprotection of renin-angiotensin system inhibition in rats with renal mass reduction. Kidney Int. 2009; 76:960–7.7. Morgenthaler NG, Struck J, Alonso C, Bergmann A. Assay for the measurement of copeptin, a stable peptide derived from the precursor of vasopressin. Clin Chem. 2006; 52:112–9.8. Tasevska I, Enhorning S, Christensson A, Persson M, Nilsson PM, Melander O. Increased levels of copeptin, a surrogate marker of arginine vasopressin, are associated with an increased risk of chronic kidney disease in a general population. Am J Nephrol. 2016; 44:22–8.9. White C, Akbari A, Hussain N, Dinh L, Filler G, Lepage N, et al. Estimating glomerular filtration rate in kidney transplantation: a comparison between serum creatinine and cystatin C-based methods. J Am Soc Nephrol. 2005; 16:3763–70.10. Luis-Lima S, Marrero-Miranda D, Gonzalez-Rinne A, Torres A, Gonzalez-Posada JM, Rodriguez A, et al. Estimated glomerular filtration rate in renal transplantation: the nephrologist in the mist. Transplantation. 2015; 99:2625–33.11. Han SS, Han M, Park JY, An JN, Park S, Park SK, et al. Posttransplant hyponatremia predicts graft failure and mortality in kidney transplantation recipients: a multicenter cohort study in Korea. PLoS One. 2016; 11:e0156050.12. Mazloum M, Jouffroy J, Brazier F, Legendre C, Neuraz A, Garcelon N, et al. Osmoregulation performance and kidney transplant outcome. J Am Soc Nephrol. 2019; 30:1282–93.13. Meijer E, Bakker SJ, de Jong PE, Homan van der Heide JJ, van Son WJ, Struck J, et al. Copeptin, a surrogate marker of vasopressin, is associated with accelerated renal function decline in renal transplant recipients. Transplantation. 2009; 88:561–7.14. Morgenthaler NG, Struck J, Jochberger S, Dunser MW. Copeptin: clinical use of a new biomarker. Trends Endocrinol Metab. 2008; 19:43–9.15. Mockel M, Searle J, Hamm C, Slagman A, Blankenberg S, Huber K, et al. Early discharge using single cardiac troponin and copeptin testing in patients with suspected acute coronary syndrome (ACS): a randomized, controlled clinical process study. Eur Heart J. 2015; 36:369–76.16. Potier L, Roussel R, Marre M, Bjornstad P, Cherney DZ, El Boustany R, et al. Plasma copeptin and risk of lower-extremity amputation in type 1 and type 2 diabetes. Diabetes Care. 2019; 42:2290–7.17. Villela-Torres ML, Higareda-Mendoza AE, Gomez-Garcia A, Alvarez-Paredes AR, Garcia-Lopez E, Stenvikel P, et al. Copeptin plasma levels are associated with decline of renal function in patients with type 2 diabetes mellitus. Arch Med Res. 2018; 49:36–43.18. Zhu FX, Wu HL, Tu KS, Chen JX, Zhang M, Shi C. Serum levels of copeptin are associated with type 2 diabetes and diabetic complications in Chinese population. J Diabetes Complications. 2016; 30:1566–70.19. Enhorning S, Hedblad B, Nilsson PM, Engstrom G, Melander O. Copeptin is an independent predictor of diabetic heart disease and death. Am Heart J. 2015; 169:549–56.20. Malyszko J, Przybylowski P, Koc-Zorawska E, Iaina-Levin N, Sadowski J, Mysliwiec M, et al. Copeptin in relation to New York Heart Association class in heart transplant recipients and kidney transplant recipients. Transplant Proc. 2010; 42:4259–62.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Significance of Anti-endothelial Cell Antibody in Renal Transplant Recipients
- Malignancy in Renal Transplant Recipients
- Clinical Manifestations of BK Virus Infection in Kidney Transplant Recipients: A Single Center Experience
- The Risk Factors and Natural History of Chronic Kidney Disease in Liver Transplant Recipients
- Kidney Transplant Program of the Ajou University Hospital