J Korean Med Sci.
2023 Jan;38(3):e10. 10.3346/jkms.2023.38.e10.
Mortality of Deep Brain Stimulation and Risk Factors in Patients With Parkinson's Disease: A National Cohort Study in Korea
- Affiliations
-
- 1Department of Neurology, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea
- 2Informatization Department, Ewha Womans University Seoul Hospital, Seoul, Korea
- 3Department of Occupational and Environmental Medicine, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea
- 4Department of Neurology, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2538369
- DOI: http://doi.org/10.3346/jkms.2023.38.e10
Abstract
- Background
This study aimed to investigate 1) long-term outcomes of deep brain stimulation (DBS), such as mortality after DBS as well as the causes of death, 2) demographic and socioeconomic factors influencing mortality, and 3) comorbidities affecting mortality after DBS in patients with Parkinson’s disease (PD).
Methods
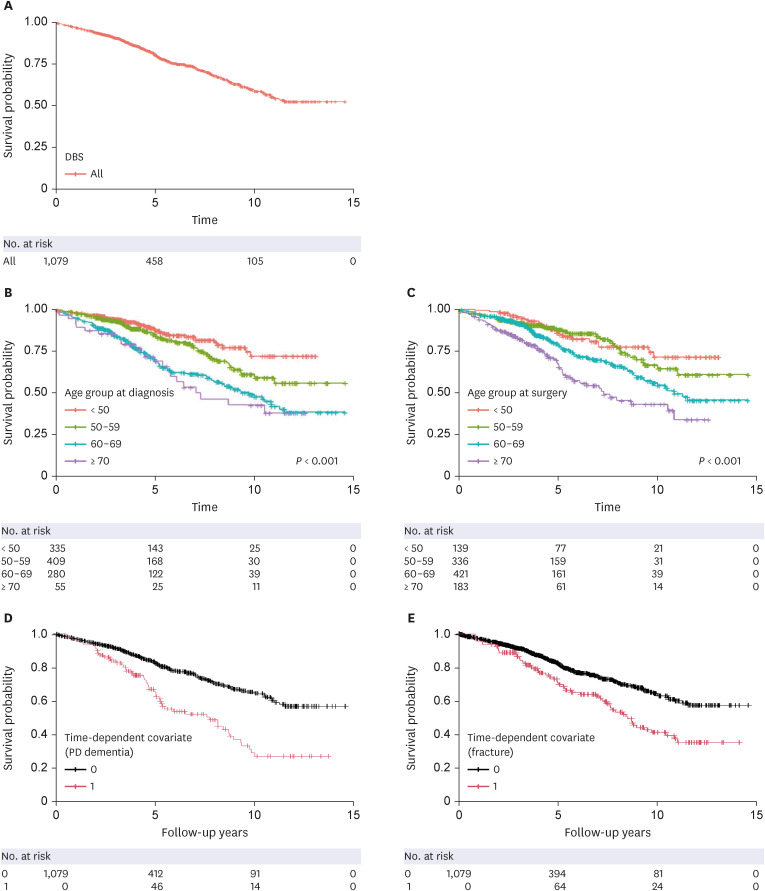
This study analyzed the National Health Insurance Service-National Health Information Database. Data on patients with PD diagnosis codes from 2002 to 2019 were extracted and analyzed. Data on the causes of death were obtained by linking the causes of death to data from Statistics Korea. The Kaplan-Meier method with the log-rank test was used for survival analysis. Multivariate Cox regression analyses were used to estimate hazard ratios (HRs) and their 95% confidence intervals. Regarding comorbidities such as PD dementia and fracture, which did not satisfy the assumption for the proportional HR, timedependent Cox analysis with the Mantel-Byar method was used.
Results
From 2005 to 2017, among 156,875 patients diagnosed with PD in Korea, 1,079 patients underwent DBS surgery, and 251 (23.3%) had died by 2019. The most common cause of death (47.1%) was PD. In the multivariate Cox regression analysis, the higher the age at diagnosis and surgery, the higher the mortality rate. The men and medical aid groups had significantly higher mortality rates. PD dementia and fracture were identified as risk factors for mortality.
Conclusion
Older age at diagnosis and surgery, being male, the use of medical aid, and the comorbidity of dementia and fractures were associated with a higher risk of mortality after DBS in patients with PD. Neurologists should consider these risk factors in assessing the prognosis of PD patients undergoing DBS.
Keyword
Figure
Reference
-
1. Kleiner-Fisman G, Herzog J, Fisman DN, Tamma F, Lyons KE, Pahwa R, et al. Subthalamic nucleus deep brain stimulation: summary and meta-analysis of outcomes. Mov Disord. 2006; 21(Suppl 14):S290–S304. PMID: 16892449.2. Deuschl G, Schade-Brittinger C, Krack P, Volkmann J, Schäfer H, Bötzel K, et al. A randomized trial of deep-brain stimulation for Parkinson’s disease. N Engl J Med. 2006; 355(9):896–908. PMID: 16943402.3. Schüpbach MW, Welter ML, Bonnet AM, Elbaz A, Grossardt BR, Mesnage V, et al. Mortality in patients with Parkinson’s disease treated by stimulation of the subthalamic nucleus. Mov Disord. 2007; 22(2):257–261. PMID: 17149702.4. Toft M, Lilleeng B, Ramm-Pettersen J, Skogseid IM, Gundersen V, Gerdts R, et al. Long-term efficacy and mortality in Parkinson’s disease patients treated with subthalamic stimulation. Mov Disord. 2011; 26(10):1931–1934. PMID: 21656853.5. Rocha S, Monteiro A, Linhares P, Chamadoira C, Basto MA, Reis C, et al. Long-term mortality analysis in Parkinson’s disease treated with deep brain stimulation. Parkinsons Dis. 2014; 2014:717041. PMID: 24772365.6. Bang Henriksen M, Johnsen EL, Sunde N, Vase A, Gjelstrup MC, Østergaard K. Surviving 10 years with deep brain stimulation for Parkinson’s disease--a follow-up of 79 patients. Eur J Neurol. 2016; 23(1):53–61. PMID: 25492023.7. Ryu HS, Kim MS, You S, Kim MJ, Kim YJ, Kim J, et al. Mortality of advanced Parkinson’s disease patients treated with deep brain stimulation surgery. J Neurol Sci. 2016; 369:230–235. PMID: 27653896.8. Ngoga D, Mitchell R, Kausar J, Hodson J, Harries A, Pall H. Deep brain stimulation improves survival in severe Parkinson’s disease. J Neurol Neurosurg Psychiatry. 2014; 85(1):17–22. PMID: 23843542.9. Wider C, Pollo C, Bloch J, Burkhard PR, Vingerhoets FJ. Long-term outcome of 50 consecutive Parkinson’s disease patients treated with subthalamic deep brain stimulation. Parkinsonism Relat Disord. 2008; 14(2):114–119. PMID: 17822940.10. Lilleeng B, Brønnick K, Toft M, Dietrichs E, Larsen JP. Progression and survival in Parkinson’s disease with subthalamic nucleus stimulation. Acta Neurol Scand. 2014; 130(5):292–298. PMID: 24495107.11. Genc G, Abboud H, Oravivattanakul S, Alsallom F, Thompson NR, Cooper S, et al. Socioeconomic status may impact functional outcome of deep brain stimulation surgery in Parkinson’s disease. Neuromodulation. 2016; 19(1):25–30. PMID: 26076401.12. Merola A, Rizzi L, Artusi CA, Zibetti M, Rizzone MG, Romagnolo A, et al. Subthalamic deep brain stimulation: clinical and neuropsychological outcomes in mild cognitive impaired parkinsonian patients. J Neurol. 2014; 261(9):1745–1751. PMID: 24952619.13. National Health Insurance Service (KR). Population covered by health insurance. Updated 2022. Accessed August 20, 2022. https://www.nhis.or.kr/nhis/policy/wbhada01700m01.do .14. Statistics Korea. The 8th Korean Standard Disease Cause Classification. Daejeon, Korea: Statistics Korea;2020.15. Jeong SM, Han K, Kim D, Rhee SY, Jang W, Shin DW. Body mass index, diabetes, and the risk of Parkinson’s disease. Mov Disord. 2020; 35(2):236–244. PMID: 31785021.16. Nam GE, Kim NH, Han K, Choi KM, Chung HS, Kim JW, et al. Chronic renal dysfunction, proteinuria, and risk of Parkinson’s disease in the elderly. Mov Disord. 2019; 34(8):1184–1191. PMID: 31021467.17. York MK, Dulay M, Macias A, Levin HS, Grossman R, Simpson R, et al. Cognitive declines following bilateral subthalamic nucleus deep brain stimulation for the treatment of Parkinson’s disease. J Neurol Neurosurg Psychiatry. 2008; 79(7):789–795. PMID: 17965146.18. Shin H, Shin Y, Hwang D, Choi B, Yoon S. Medical Aid System Evaluation and Basic Plan Establishment Research. Sejong, Korea: Korea Institute for Health and Social Affairs;2017.19. Sundararajan V, Henderson T, Perry C, Muggivan A, Quan H, Ghali WA. New ICD-10 version of the Charlson comorbidity index predicted in-hospital mortality. J Clin Epidemiol. 2004; 57(12):1288–1294. PMID: 15617955.20. Shintani AK, Girard TD, Eden SK, Arbogast PG, Moons KG, Ely EW. Immortal time bias in critical care research: application of time-varying Cox regression for observational cohort studies. Crit Care Med. 2009; 37(11):2939–2945. PMID: 19770737.21. Herlofson K, Lie SA, Arsland D, Larsen JP. Mortality and Parkinson disease: a community based study. Neurology. 2004; 62(6):937–942. PMID: 15037696.22. Willis AW, Schootman M, Kung N, Evanoff BA, Perlmutter JS, Racette BA. Predictors of survival in patients with Parkinson disease. Arch Neurol. 2012; 69(5):601–607. PMID: 22213411.23. Hughes TA, Ross HF, Mindham RH, Spokes EG. Mortality in Parkinson’s disease and its association with dementia and depression. Acta Neurol Scand. 2004; 110(2):118–123. PMID: 15242420.24. Harris-Hayes M, Willis AW, Klein SE, Czuppon S, Crowner B, Racette BA. Relative mortality in U.S. Medicare beneficiaries with Parkinson disease and hip and pelvic fractures. J Bone Joint Surg Am. 2014; 96(4):e27. PMID: 24553896.25. Benzinger P, Rapp K, Maetzler W, König HH, Jaensch A, Klenk J, et al. Risk for femoral fractures in Parkinson’s disease patients with and without severe functional impairment. PLoS One. 2014; 9(5):e97073. PMID: 24853110.26. Lau B, Meier N, Serra G, Czernecki V, Schuepbach M, Navarro S, et al. Axial symptoms predict mortality in patients with Parkinson disease and subthalamic stimulation. Neurology. 2019; 92(22):e2559–e2570. PMID: 31043471.27. Weaver FM, Stroupe KT, Smith B, Gonzalez B, Huo Z, Cao L, et al. Survival in patients with Parkinson’s disease after deep brain stimulation or medical management. Mov Disord. 2017; 32(12):1756–1763. PMID: 29150873.28. Castrioto A, Lozano AM, Poon YY, Lang AE, Fallis M, Moro E. Ten-year outcome of subthalamic stimulation in Parkinson disease: a blinded evaluation. Arch Neurol. 2011; 68(12):1550–1556. PMID: 21825213.29. Zhang Y, Wang C, Wang Y, Xiao Q, Liu J, Ma J, et al. Mortality from Parkinson’s disease in China: findings from a ten-year follow up study in Shanghai. Parkinsonism Relat Disord. 2018; 55:75–80. PMID: 29802079.30. Rocha AL, Oliveira A, Sousa C, Monteiro P, Rosas MJ, Vaz R. Long term mortality of patients with Parkinson’s disease treated with deep brain stimulation in a reference center. Clin Neurol Neurosurg. 2021; 202:106486. PMID: 33493881.31. Kanna SV, Bhanu K. A simple bedside test to assess the swallowing dysfunction in Parkinson’s disease. Ann Indian Acad Neurol. 2014; 17(1):62–65. PMID: 24753662.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Levodopa-induced respiratory dysfunction in Parkinson’s disease managed with subthalamic nucleus deep brain stimulation
- A Nationwide Cohort Study of Mortality of Deep Brain Stimulation Surgery in Parkinson’s Disease
- Inadequate Efficacy of Deep Brain Stimulation in a Patient with Parkinson's disease due to Partial Breakage of Electrode Lead
- Benefits of Levodopa-Carbidopa Intestinal Gel Infusion in Patients with Parkinson's Disease Experiencing Gait Dysfunction Following Subthalamic Deep Brain Stimulation
- Deep Brain Stimulation of the Subthalamic and Pedunculopontine Nucleus in a Patient with Parkinson's Disease