Prog Med Phys.
2022 Dec;33(4):136-141. 10.14316/pmp.2022.33.4.136.
Development of a Breath Control Training System for Breath-Hold Techniques and Respiratory-Gated Radiation Therapy
- Affiliations
-
- 1Interdisciplinary Program in Bioengineering, Seoul National University, Seoul, Korea
- 2Department of Radiation Oncology, Seoul National University Hospital, Seoul, Korea
- 3Biomedical Research Institute, Seoul National University Hospital, Seoul, Korea
- 4Institute of Radiation Medicine, Seoul National University Hospital, Seoul, Korea
- KMID: 2537882
- DOI: http://doi.org/10.14316/pmp.2022.33.4.136
Abstract
- Purpose
This study aimed to develop a breath control training system for breath-hold technique and respiratory-gated radiation therapy wherein the patients can learn breath-hold techniques in their convenient environment.
Methods
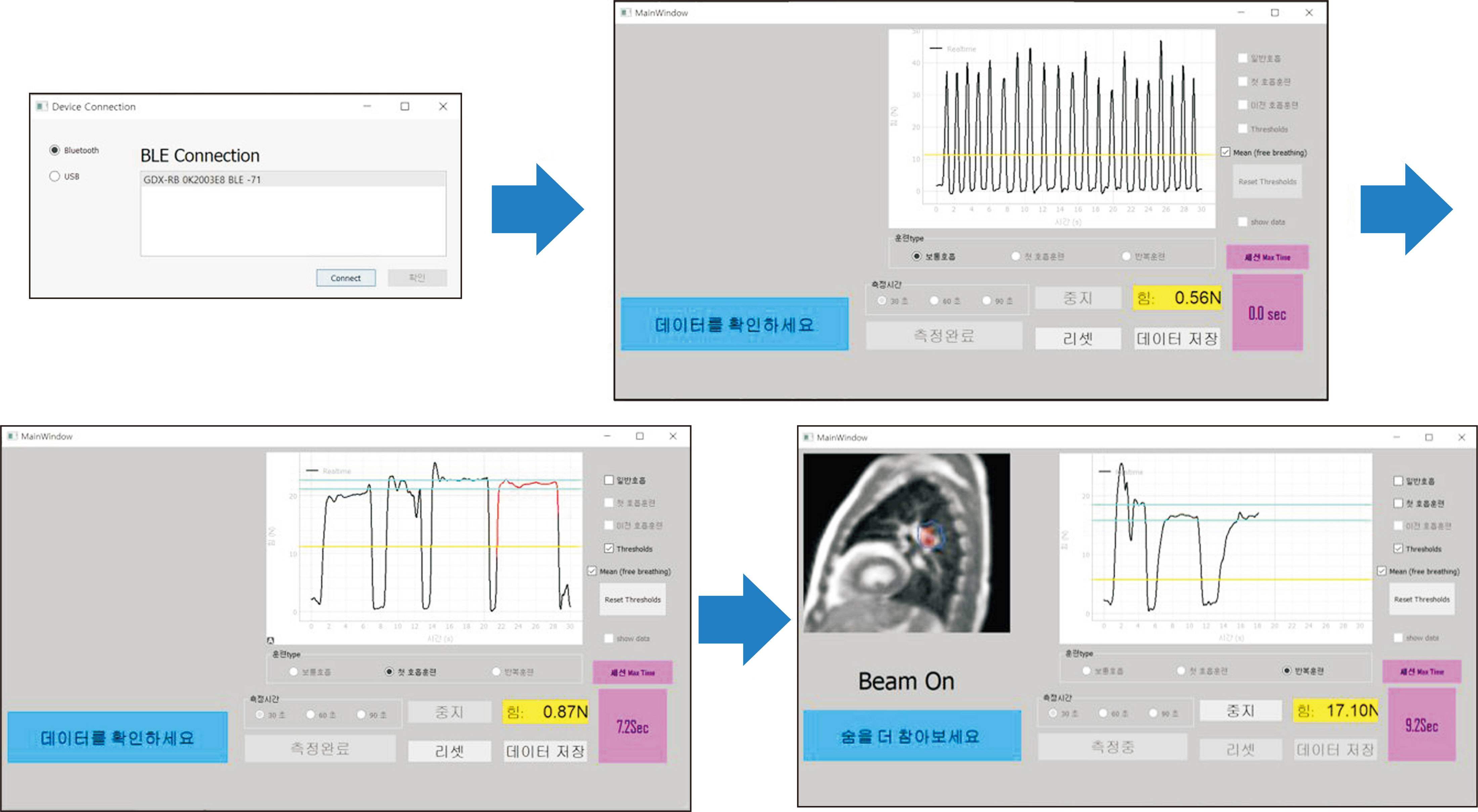
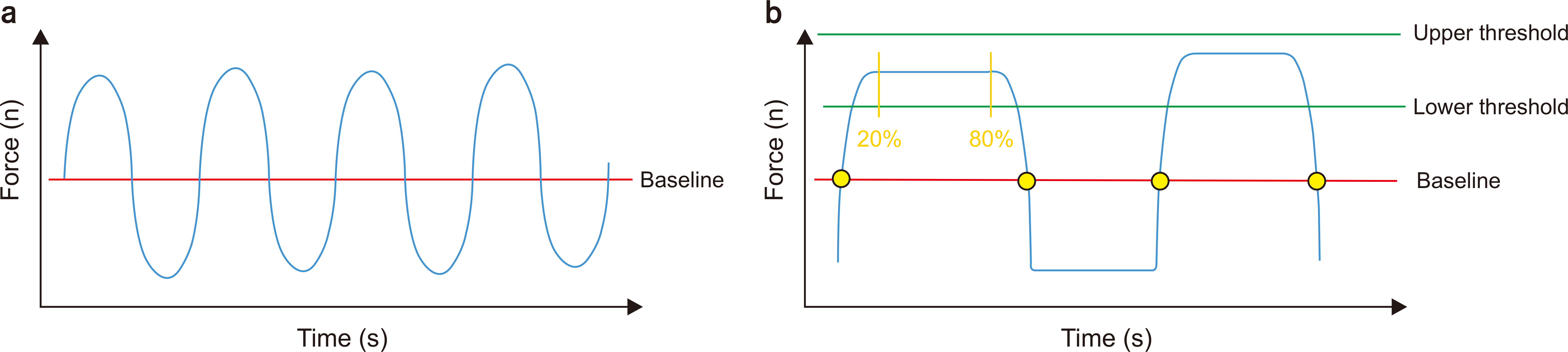
The breath control training system comprises a sensor device and software. The sensor device uses a loadcell sensor and an adjustable strap around the chest to acquire respiratory signals. The device connects via Bluetooth to a computer where the software is installed. The software visualizes the respiratory signal in near real-time with a graph. The developed system can signal patients through visual (software), auditory (buzzer), and tactile (vibrator) stimulation when breath-holding starts. A motion phantom was used to test the basic functions of the developed breath control training system. The relative standard deviation of the maxima of the emulated free breathing data was calculated. Moreover, a relative standard deviation of a breath-holding region was calculated for the simulated breath-holding data.
Results
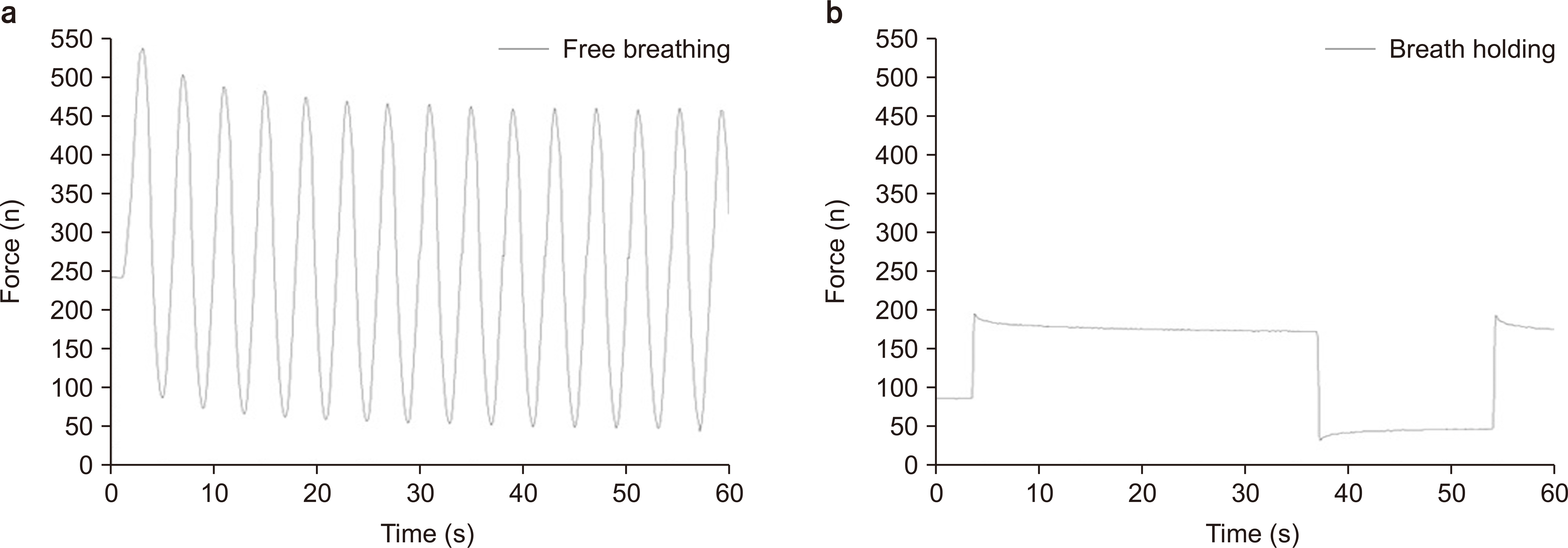
The average force of the maxima was 487.71 N, and the relative standard deviation was 4.8%, while the average force of the breath hold region was 398.5 N, and the relative standard deviation was 1.8%. The data acquired through the sensor was consistent with the motion created by the motion phantom.
Conclusions
We have developed a breath control training system comprising a sensor device and software that allow patients to learn breath-hold techniques in their convenient environment.
Keyword
Figure
Reference
-
References
1. Keall PJ, Mageras GS, Balter JM, Emery RS, Forster KM, Jiang SB, et al. 2006; The management of respiratory motion in radiation oncology report of AAPM Task Group 76. Med Phys. 33:3874–3900. DOI: 10.1118/1.2349696. PMID: 17089851.
Article2. Redmond KJ, Song DY, Fox JL, Zhou J, Rosenzweig CN, Ford E. 2009; Respiratory motion changes of lung tumors over the course of radiation therapy based on respiration-correlated four-dimensional computed tomography scans. Int J Radiat Oncol Biol Phys. 75:1605–1612. DOI: 10.1016/j.ijrobp.2009.05.024. PMID: 19931739.
Article3. George R, Keall PJ, Kini VR, Vedam SS, Siebers JV, Wu Q, et al. 2003; Quantifying the effect of intrafraction motion during breast IMRT planning and dose delivery. Med Phys. 30:552–562. DOI: 10.1118/1.1543151. PMID: 12722807.
Article4. Jiang SB. 2006; Technical aspects of image-guided respiration-gated radiation therapy. Med Dosim. 31:141–151. DOI: 10.1016/j.meddos.2005.12.005. PMID: 16690455.
Article5. Sixel KE, Aznar MC, Ung YC. 2001; Deep inspiration breath hold to reduce irradiated heart volume in breast cancer patients. Int J Radiat Oncol Biol Phys. 49:199–204. DOI: 10.1016/S0360-3016(00)01455-3. PMID: 11163515.
Article6. Kini VR, Vedam SS, Keall PJ, Patil S, Chen C, Mohan R. 2003; Patient training in respiratory-gated radiotherapy. Med Dosim. 28:7–11. DOI: 10.1016/S0958-3947(02)00136-X. PMID: 12747612.
Article7. Boda-Heggemann J, Knopf AC, Simeonova-Chergou A, Wertz H, Stieler F, Jahnke A, et al. 2016; Deep inspiration breath hold-based radiation therapy: a clinical review. Int J Radiat Oncol Biol Phys. 94:478–492. DOI: 10.1016/j.ijrobp.2015.11.049. PMID: 26867877.
Article8. George R, Chung TD, Vedam SS, Ramakrishnan V, Mohan R, Weiss E, et al. 2006; Audio-visual biofeedback for respiratory-gated radiotherapy: impact of audio instruction and audio-visual biofeedback on respiratory-gated radiotherapy. Int J Radiat Oncol Biol Phys. 65:924–933. DOI: 10.1016/j.ijrobp.2006.02.035. PMID: 16751075.
Article9. He P, Li Q, Zhao T, Liu X, Dai Z, Ma Y. 2016; Effectiveness of respiratory-gated radiotherapy with audio-visual biofeedback for synchrotron-based scanned heavy-ion beam delivery. Phys Med Biol. 61:8541–8552. DOI: 10.1088/0031-9155/61/24/8541. PMID: 27845937.
Article10. Linthout N, Bral S, Van de Vondel I, Verellen D, Tournel K, Gevaert T, et al. 2009; Treatment delivery time optimization of respiratory gated radiation therapy by application of audio-visual feedback. Radiother Oncol. 91:330–335. DOI: 10.1016/j.radonc.2009.03.019. PMID: 19368987.
Article11. Kim JI, Lee H, Wu HG, Chie EK, Kang HC, Park JM. 2017; Development of patient-controlled respiratory gating system based on visual guidance for magnetic-resonance image-guided radiation therapy. Med Phys. 44:4838–4846. DOI: 10.1002/mp.12447. PMID: 28675492.
Article12. Choun HJ, Kim JI, Choi CH, Jung S, Jin H, Wu HG, et al. 2022; Performance evaluation of a visual guidance patient-controlled respiratory gating system for respiratory-gated magnetic-resonance image-guided radiation therapy. Phys Eng Sci Med. 45:809–816. DOI: 10.1007/s13246-022-01144-0. PMID: 35723860.
Article13. Berson AM, Emery R, Rodriguez L, Richards GM, Ng T, Sanghavi S, et al. 2004; Clinical experience using respiratory gated radiation therapy: comparison of free-breathing and breath-hold techniques. Int J Radiat Oncol Biol Phys. 60:419–426. DOI: 10.1016/j.ijrobp.2004.03.037. PMID: 15380575.
Article14. Masaoka Y, Homma I. 1997; Anxiety and respiratory patterns: their relationship during mental stress and physical load. Int J Psychophysiol. 27:153–159. DOI: 10.1016/S0167-8760(97)00052-4. PMID: 9342646.
Article15. Kim A, Kalet AM, Cao N, Hippe DS, Fang LC, Young L, et al. 2018; Effects of preparatory coaching and home practice for deep inspiration breath hold on cardiac dose for left breast radiation therapy. Clin Oncol (R Coll Radiol). 30:571–577. DOI: 10.1016/j.clon.2018.04.009. PMID: 29773446.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Quasi-breath-hold (QBH) Biofeedback in Gated 3D Thoracic MRI: Feasibility Study
- MR Cholangiopancreatography: Comparison of Breath-hold Fast Spin Echo and Respiratory Triggered Fast Spin Echo Techniques
- Effectiveness of Breath Hold with a ABC for SRS of Lung Cancer
- Comparison of Non-Breath-Hold T2-weighted Turbo Spin-Echo and Three Breath-Hold T2-weighted MR Images for Detection of Focal Hepatic Lesion
- Single breath-hold MR imaging of liver