J Korean Neurosurg Soc.
2023 Jan;66(1):33-43. 10.3340/jkns.2022.0112.
Comparison of Outcomes of Multi-Level Anterior, Oblique, Transforaminal Lumbar Interbody Fusion Surgery : Impact on Global Sagittal Alignment
- Affiliations
-
- 1Department of Neurosurgery, Kyung Hee University Hospital at Gangdong, Kyung Hee University College of Medicine, Seoul, Korea
- KMID: 2537846
- DOI: http://doi.org/10.3340/jkns.2022.0112
Abstract
Objective
: To compare the outcomes of anterior lumbar interbody fusion (ALIF), oblique lumbar interbody fusion (OLIF), and transforaminal lumbar interbody fusion (TLIF) in terms of global sagittal alignment.
Methods
: From January 2007 to December 2019, 141 adult patients who underwent multilevel interbody fusion for lumbar degenerative disorders were enrolled. Regarding the approach, patients were divided into the ALIF (n=23), OLIF (n=60), and TLIF (n=58) groups. Outcomes, including local radiographic parameters and global sagittal alignment, were then compared between the treatment groups.
Results
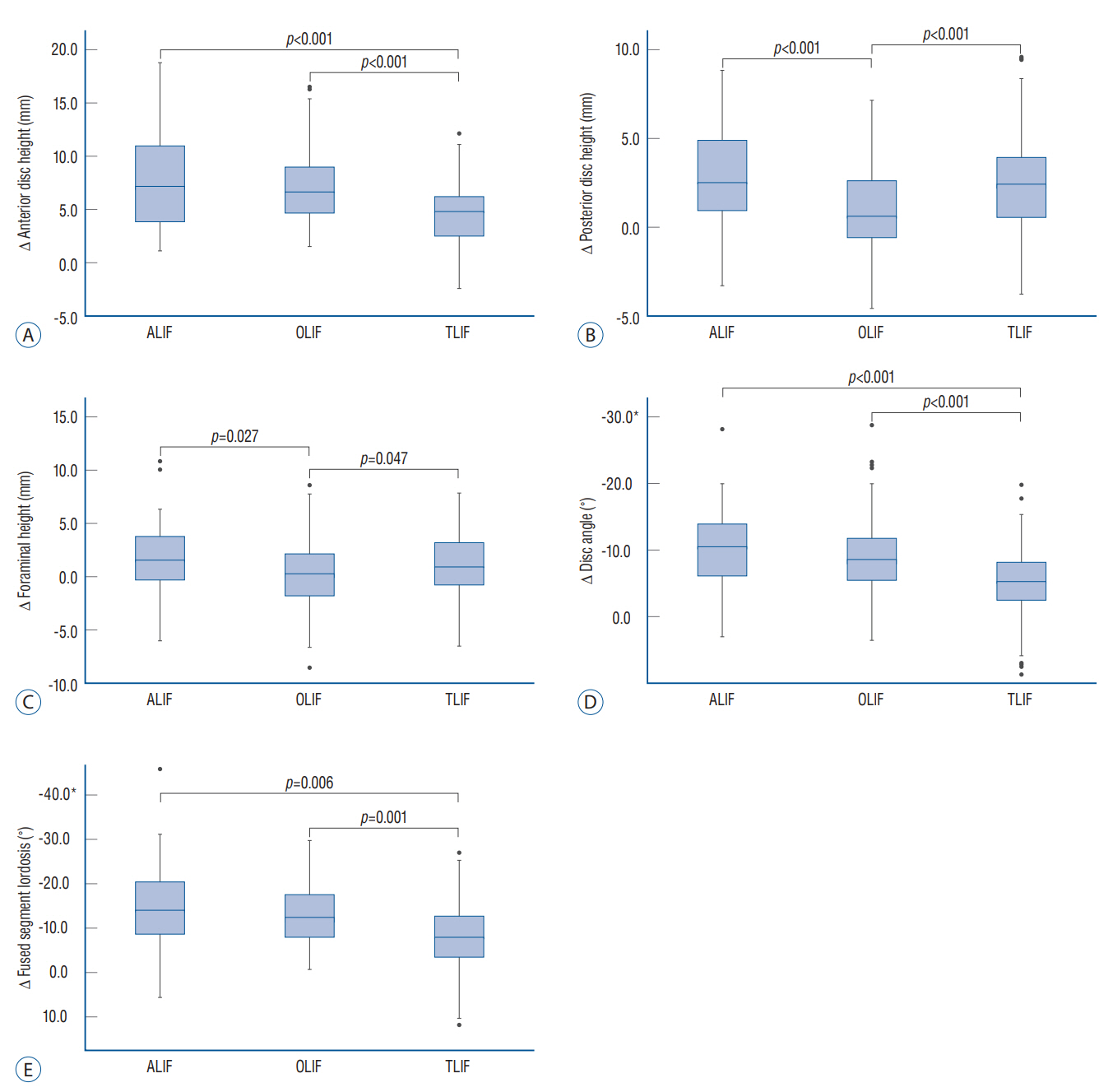
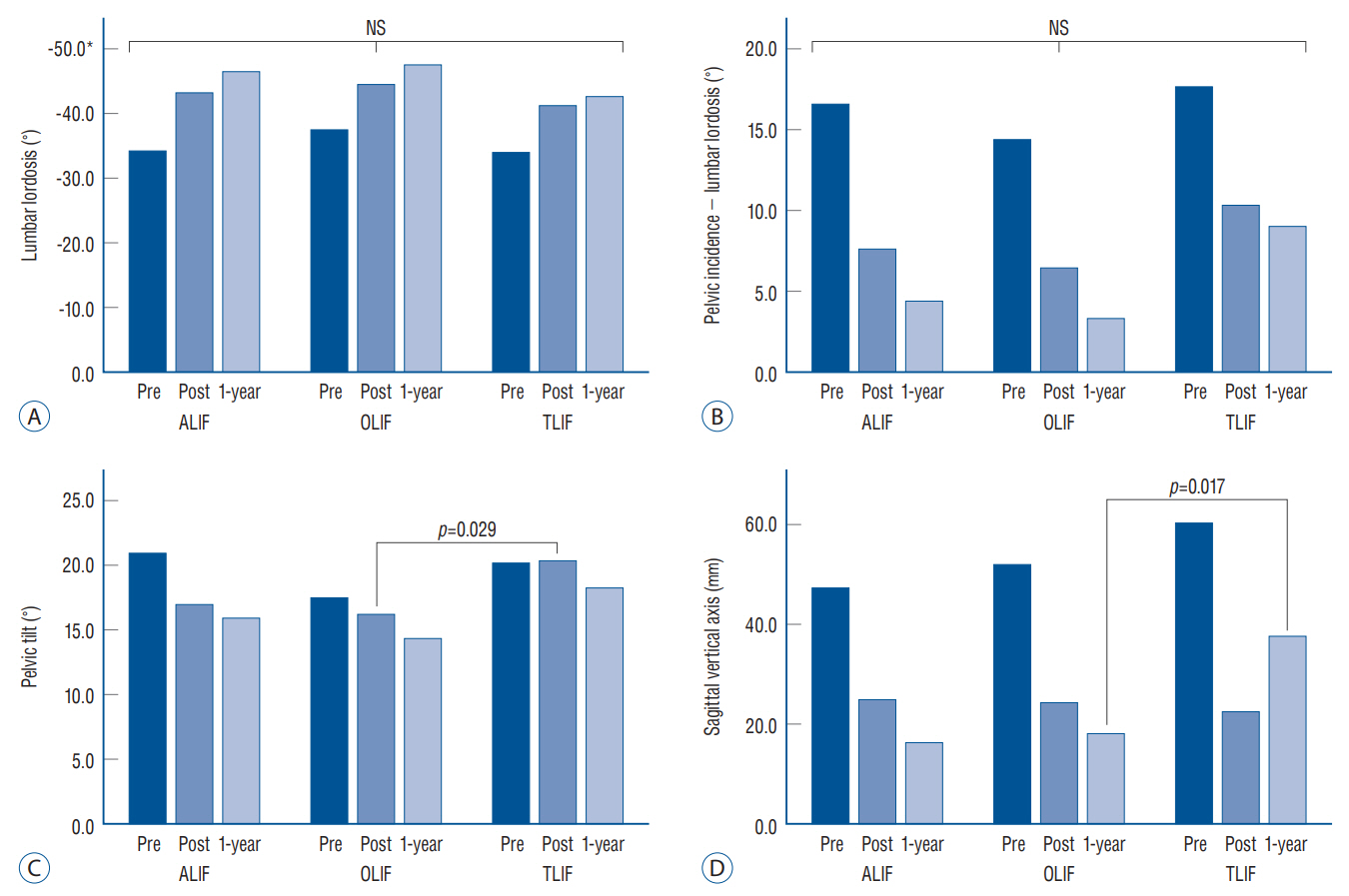
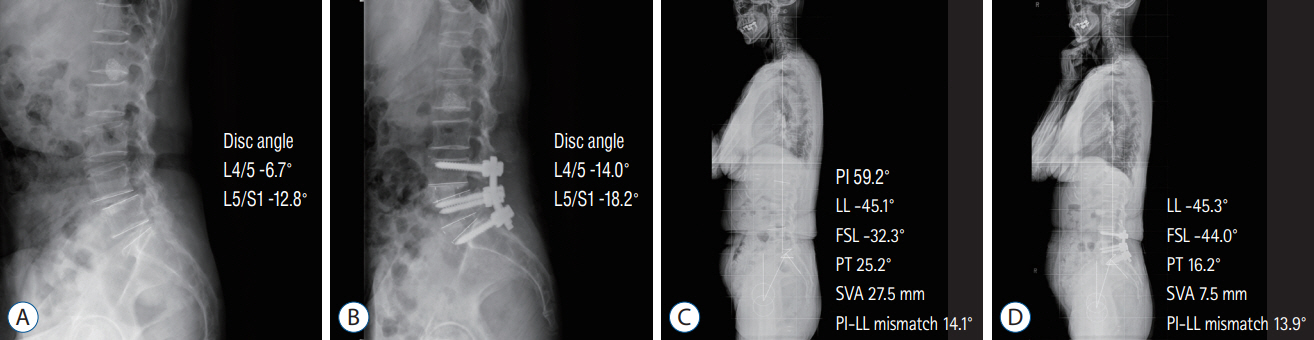
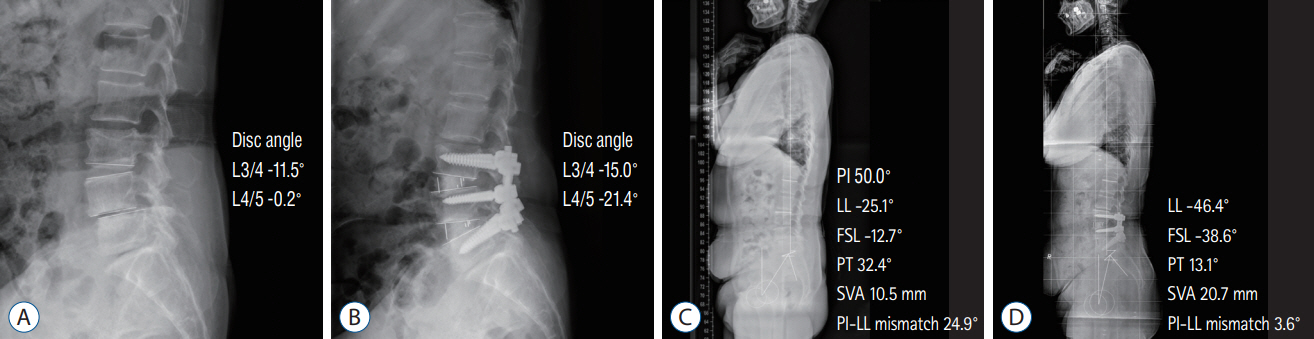
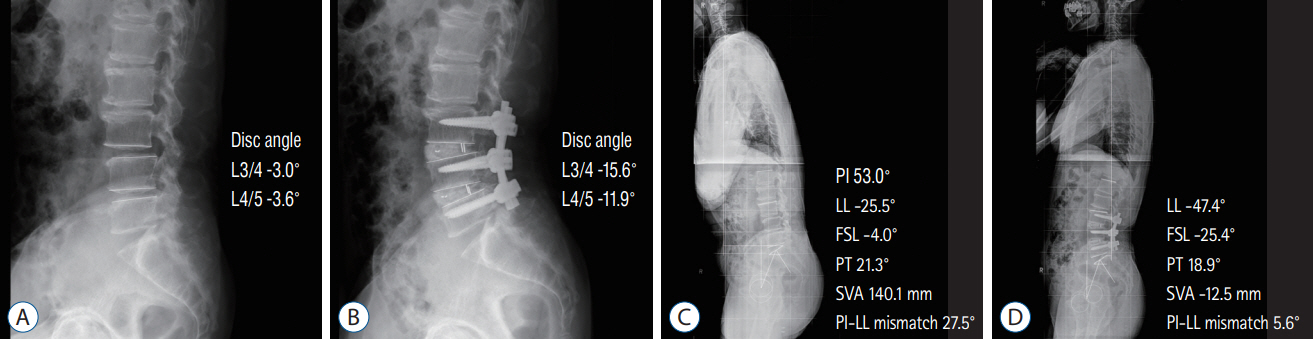
: Regarding local radiographic parameters, ALIF and OLIF were superior to TLIF in terms of the change in the anterior disc height (7.6±4.5 mm vs. 6.9±3.2 mm vs. 4.7±2.9 mm, p=0.000), disc angle (-10.0°±6.3° vs. -9.2°±5.2° vs. -5.1°±5.1°, p=0.000), and fused segment lordosis (-14.5°±11.3° vs. -13.8°±7.5° vs. -7.4°±9.1°, p=0.000). However, regarding global sagittal alignment, postoperative lumbar lordosis (-42.5°±9.6° vs. -44.4°±11.6° vs. -40.6°±12.3°, p=0.210), pelvic incidence-lumbar lordosis mismatch (7.9°±11.3° vs. 6.7°±11.6° vs. 11.5°±13.0°, p=0.089), and the sagittal vertical axis (24.3±28.5 mm vs. 24.5±34.0 mm vs. 25.2±36.6 mm, p=0.990) did not differ between the groups.
Conclusion
: Although the anterior approaches were superior in terms of local radiographic parameters, TLIF achieved adequate global sagittal alignment, comparable to the anterior approaches.
Keyword
Figure
Reference
-
References
1. Champagne PO, Walsh C, Diabira J, Plante MÉ, Wang Z, Boubez G, et al. Sagittal balance correction following lumbar interbody fusion: a comparison of the three approaches. Asian Spine J. 13:450–458. 2019.2. Chung HW, Lee HD, Jeon CH, Chung NS. Comparison of surgical outcomes between oblique lateral interbody fusion (OLIF) and anterior lumbar interbody fusion (ALIF). Clin Neurol Neurosurg. 209:106901. 2021.3. Han SH, Hyun SJ, Jahng TA, Kim KJ. A comparative radiographic analysis of fusion rate between L4-5 and L5-S1 in a single level posterior lumbar interbody fusion. Korean J Spine. 12:60–67. 2015.4. Hsieh PC, Koski TR, O’Shaughnessy BA, Sugrue P, Salehi S, Ondra S, et al. Anterior lumbar interbody fusion in comparison with transforaminal lumbar interbody fusion: implications for the restoration of foraminal height, local disc angle, lumbar lordosis, and sagittal balance. J Neurosurg Spine. 7:379–386. 2007.5. Hyun SJ, Yoon SH, Kim JH, Oh JK, Lee CH, Shin JJ, et al. A prospective, multi-center, double-blind, randomized study to evaluate the efficacy and safety of the synthetic bone graft material DBM gel with rhBMP-2 versus DBM gel used during the TLIF procedure in patients with lumbar disc disease. J Korean Neurosurg Soc. 64:562–574. 2021.6. Jo DJ, Seo EM. Efficacy and radiographic analysis of oblique lumbar interbody fusion in treating adult spinal deformity. PLoS One. 16:e0257316. 2021.7. Koike Y, Kotani Y, Terao H, Iwasaki N. Comparison of outcomes of oblique lateral interbody fusion with percutaneous posterior fixation in ateral position and minimally invasive transforaminal lumbar interbody fusion for degenerative spondylolisthesis. Asian Spine J. 15:97–106. 2021.8. Kono Y, Gen H, Sakuma Y, Koshika Y. Comparison of clinical and radiologic results of mini-open transforaminal lumbar interbody fusion and extreme lateral interbody fusion indirect decompression for degenerative lumbar spondylolisthesis. Asian Spine J. 12:356–364. 2018.9. Lee N, Kim KN, Yi S, Ha Y, Shin DA, Yoon DH, et al. Comparison of outcomes of anterior, posterior, and transforaminal lumbar interbody fusion surgery at a single lumbar level with degenerative spinal disease. World Neurosurg. 101:216–226. 2017.10. Li R, Shao X, Li X, Liu Y, Jiang W. Comparison of clinical outcomes and spino-pelvic sagittal balance in degenerative lumbar spondylolisthesis: minimally invasive oblique lumbar interbody fusion (OLIF) versus transforaminal lumbar interbody fusion (TLIF). Medicine (Baltimore). 100:e23783. 2021.11. Mobbs RJ, Phan K, Malham G, Seex K, Rao PJ. Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg. 1:2–18. 2015.12. Moses ZB, Razvi S, Oh SY, Platt A, Keegan KC, Hamati F, et al. A retrospective comparison of radiographic and clinical outcomes in single-level degenerative lumbar disease undergoing anterior versus transforaminal lumbar interbody fusion. J Spine Surg. 7:170–180. 2021.13. Nakashima H, Kanemura T, Satake K, Ishikawa Y, Ouchida J, Segi N, et al. Changes in sagittal alignment following short-level lumbar interbody fusion: comparison between posterior and lateral lumbar interbody fusions. Asian Spine J. 13:904–912. 2019.14. Patel DV, Yoo JS, Karmarkar SS, Lamoutte EH, Singh K. Interbody options in lumbar fusion. J Spine Surg. 5(Suppl 1):S19–S24. 2019.15. Phan K, Thayaparan GK, Mobbs RJ. Anterior lumbar interbody fusion versus transforaminal lumbar interbody fusion--systematic review and meta-analysis. Br J Neurosurg. 29:705–711. 2015.16. Potter BK, Lenke LG, Kuklo TR. Prevention and management of iatrogenic flatback deformity. J Bone Joint Surg Am. 86:1793–1808. 2004.17. Reisener MJ, Pumberger M, Shue J, Girardi FP, Hughes AP. Trends in lumbar spinal fusion-a literature review. J Spine Surg. 6:752–761. 2020.18. Saadeh YS, Joseph JR, Smith BW, Kirsch MJ, Sabbagh AM, Park P. Comparison of segmental lordosis and global spinopelvic alignment after single-level lateral lumbar interbody fusion or transforaminal lumbar interbody fusion. World Neurosurg. 126:e1374–e1378. 2019.19. Schwab F, Patel A, Ungar B, Farcy JP, Lafage V. Adult spinal deformity-postoperative standing imbalance: how much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine (Phila Pa 1976). 35:2224–2231. 2010.20. Schwab F, Ungar B, Blondel B, Buchowski J, Coe J, Deinlein D, et al. Scoliosis Research Society-Schwab adult spinal deformity classification: a validation study. Spine (Phila Pa 1976). 37:1077–1082. 2012.21. Schwab FJ, Blondel B, Bess S, Hostin R, Shaffrey CI, Smith JS, et al. Radiographical spinopelvic parameters and disability in the setting of adult spinal deformity: a prospective multicenter analysis. Spine (Phila Pa 1976). 38:E803–E812. 2013.22. Sembrano JN, Yson SC, Horazdovsky RD, Santos ER, Polly DW Jr. Radiographic comparison of lateral lumbar interbody fusion versus traditional fusion approaches: analysis of sagittal contour change. Int J Spine Surg. 9:16. 2015.23. Takaoka H, Inage K, Eguchi Y, Shiga Y, Furuya T, Maki S, et al. Comparison between intervertebral oblique lumbar interbody fusion and transforaminal lumbar interbody fusion: a multicenter study. Sci Rep. 11:16673. 2021.24. Villavicencio AT, Burneikiene S, Nelson EL, Bulsara KR, Favors M, Thramann J. Safety of transforaminal lumbar interbody fusion and intervertebral recombinant human bone morphogenetic protein-2. J Neurosurg Spine. 3:436–443. 2005.25. Watkins RG 4th, Hanna R, Chang D, Watkins RG 3rd. Sagittal alignment after lumbar interbody fusion: comparing anterior, lateral, and transforaminal approaches. J Spinal Disord Tech. 27:253–256. 2014.26. Wu PK, Wu MH, Shih CM, Lin YK, Chen KH, Pan CC, et al. Comparison of incidence of adjacent segment pathology between anterior lumbar interbody fusion and transforaminal lumbar interbody fusion treatments for lumbosacral junction. Tomography. 7:855–865. 2021.27. Xu DS, Walker CT, Godzik J, Turner JD, Smith W, Uribe JS. Minimally invasive anterior, lateral, and oblique lumbar interbody fusion: a literature review. Ann Transl Med. 6:104. 2018.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Lumbopelvic Sagittal Alignment and Foraminal Height from Single Interbody Cage in L5-S1 Segment: Comparison between Anterior Cage for OLIF (Oblique Lumbar Interbody Fusion) and Curvilinear Cage for TLIF (Transforaminal Interbody Fusion)
- Uniportal Endoscopic Lumbar Interbody Fusion
- Minimally Invasive Strategy for Uniportal Full-Endoscopic Transforaminal Lumbar Interbody Fusion Using a Large Cage Utilized in Oblique Lumbar Interbody Fusion
- Using Lordotic Cages at the L5–S1 Level Does Not Guarantee the Improvement of Sagittal Alignment in Patients Who Underwent Posterior Lumbar Interbody Fusion
- Intraoperative Anteropulsion of an Interbody Fusion Cage During Minimally Invasive Transforaminal Lumbar Interbody Fusion: A Case Report