Anat Cell Biol.
2022 Dec;55(4):399-405. 10.5115/acb.22.062.
Congenital malformations in the vertebral column: associations and possible embryologic origins
- Affiliations
-
- 1Department of Anatomy, Health Science Campus, University of Pretoria, South Africa
- 2Department Anatomy, School of Medicine, University of Namibia, Windhoek, Namibia
- 3Department of Anatomy and Cellular Biology, College of Medicine and Health Sciences, Khalifa University, Abu Dhabi, United Arab Emirates
- KMID: 2537458
- DOI: http://doi.org/10.5115/acb.22.062
Abstract
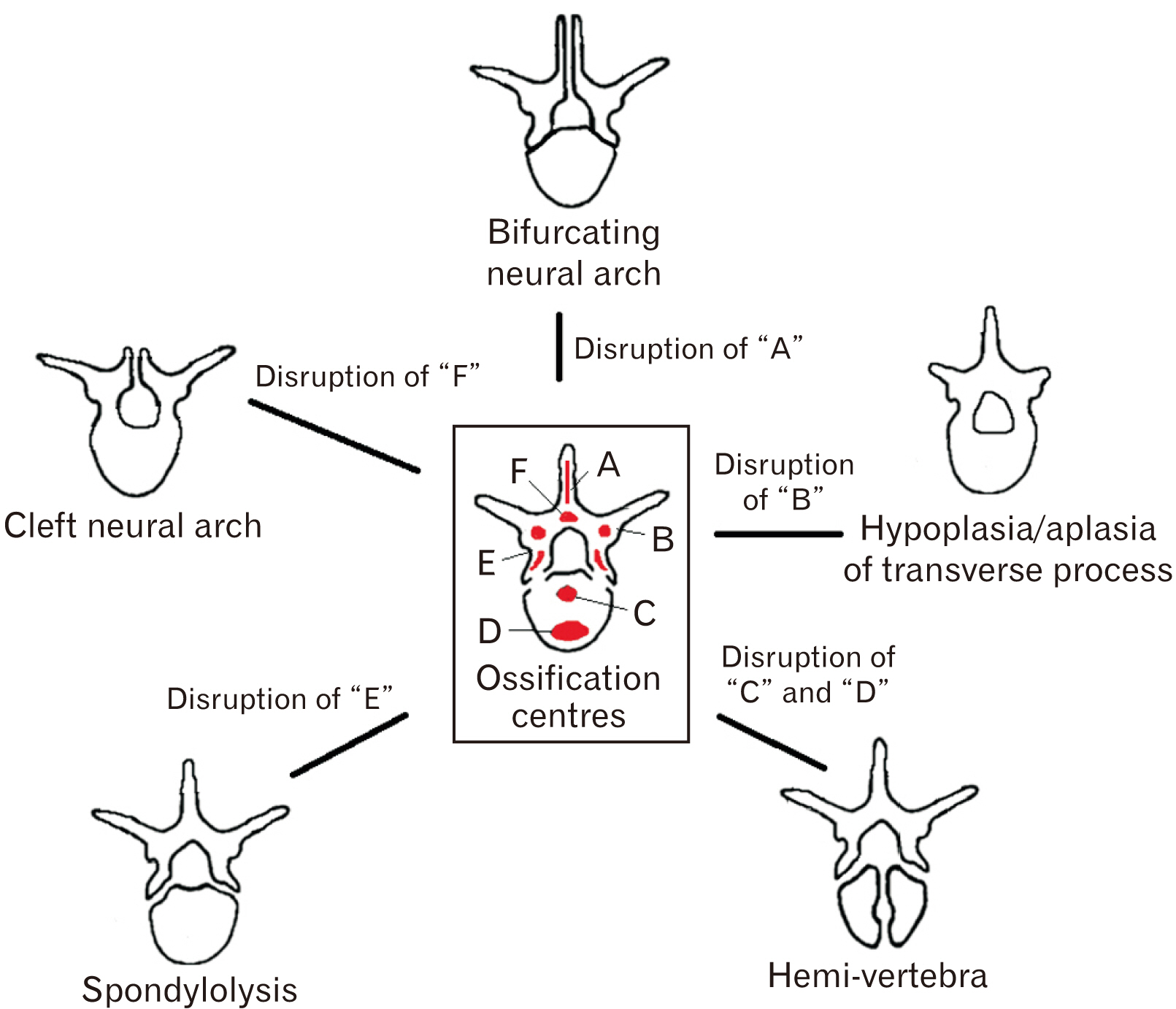
- Cases of associations between random spinal congenital defects have previously been reported, yet several questions remain unanswered. Firstly, why are associations between what seems to be random combinations of vertebral malformations observed? Secondly, is there a common event or pattern that connects the associated defects? Therefore, this study aimed to identify congenital defects in the vertebral column and also to determine whether any associations, if present, between vertebral malformations exist. This article consequently discusses the possible embryological disruptions that may lead to the formation of various defects in the vertebral column. A random skeletal sample (n=187) was selected from the Pretoria Bone Collection housed in the Department of Anatomy, University of Pretoria (Ethics 678/2018). The sample was evaluated to determine the frequencies of spinal congenital defects in each set of remains. Identifiable congenital malformations were observed in 48.1% (n=90/187) of the sample. The results demonstrated a high probability of association between the different defects observed in the vertebral column. Findings are of value as they provide a reasonable explanation to why seemingly random cases of associations have been reported by several authors. This study is clinically relevant as severe spinal defects have been shown to have high morbidity in patients and mortality in infants.
Keyword
Figure
Reference
-
References
1. Greene ND, Stanier P, Copp AJ. 2009; Genetics of human neural tube defects. Hum Mol Genet. 18(R2):R113–29. DOI: 10.1093/hmg/ddp347. PMID: 19808787. PMCID: PMC2758708.2. Puvirajesinghe TM, Borg JP. 2015; Neural tube defects: from a proteomic standpoint. Metabolites. 5:164–83. DOI: 10.3390/metabo5010164. PMID: 25789708. PMCID: PMC4381295.3. Farruggia SP, Han C, Watson L, Moss TP, Bottoms BL. 2018; Noncognitive factors and college student success. J Coll Stud Retent Res Theory Pract. 20:308–27. DOI: 10.1177/1521025116666539.4. Dias MS. 2007; Normal and abnormal development of the spine. Neurosurg Clin N Am. 18:415–29. DOI: 10.1016/j.nec.2007.05.003. PMID: 17678747.5. Rawls A, Fisher RE. Kusumi K, Dunwoodie SL, editors. 2010. Development and functional anatomy of the spine. The Genetics and Development of Scoliosis. Springer-Verlag;New York: p. 21–46. DOI: 10.1007/978-1-4419-1406-4_2.6. Thawait GK, Chhabra A, Carrino JA. 2012; Spine segmentation and enumeration and normal variants. Radiol Clin North Am. 50:587–98. DOI: 10.1016/j.rcl.2012.04.003. PMID: 22643386.7. Greene ND, Copp AJ. 2009; Development of the vertebrate central nervous system: formation of the neural tube. Prenat Diagn. 29:303–11. DOI: 10.1002/pd.2206. PMID: 19206138.8. Copp AJ, Stanier P, Greene ND. 2013; Neural tube defects: recent advances, unsolved questions, and controversies. Lancet Neurol. 12:799–810. DOI: 10.1016/S1474-4422(13)70110-8. PMID: 23790957. PMCID: PMC4023229.9. Byrd SE, Comiskey EM. 2007; Postnatal maturation and radiology of the growing spine. Neurosurg Clin N Am. 18:431–61. DOI: 10.1016/j.nec.2007.05.002. PMID: 17678748.10. Masnicová S, Beňuš R. 2003; Developmental anomalies in skeletal remains from the Great Moravia and Middle Ages cemeteries at Devín (Slovakia). Int J Osteoarchaeol. 13:266–74. DOI: 10.1002/oa.684.11. Savage C. 2005. Lumbosacral transitional vertebrae: classification of variation and association with low back pain [thesis]. University of Missouri;Columbia:12. Oostra RJ, Hennekam RC, de Rooij L, Moorman AF. 2005; Malformations of the axial skeleton in Museum Vrolik I: homeotic transformations and numerical anomalies. Am J Med Genet A. 134:268–81. DOI: 10.1002/ajmg.a.30639. PMID: 15732082.13. Krishnamurthy A, Adibatti M. 2016; Study on incidence of sacralisation of fifth lumbar vertebra in South Indian population. Ital J Anat Embryol. 121:60–5. PMID: 28872798.14. Moore KL, Agur AMR, Dalley AF. 2012. Essential clinical anatomy. 4th ed. Lippincott Williams & Wilkins;Philadelphia:15. Drake R, Vogl W, Mitchell A. 2012. Gray's anatomy for students. 2nd ed. Churchill Livingstone;Philadelphia: p. 160.16. Khairnar KB, Rajale MB. 2013; Sacralization of lumbar vertebra. Indian J Basic Appl Med Res. 2:510–4.17. Wilson RD, Wilson RD, Audibert F, Brock JA, Carroll J, Cartier L, Gagnon A, Johnson JA, Langlois S, Murphy-Kaulbeck L, Okun N, Pastuck M, Deb-Rinker P, Dodds L, Leon JA, Lowel HL, Luo W, MacFarlane A, McMillan R, Moore A, Mundle W, O'Connor D, Ray J, Van den Hof M. 2015; Pre-conception folic acid and multivitamin supplementation for the primary and secondary prevention of neural tube defects and other folic acid-sensitive congenital anomalies. J Obstet Gynaecol Can. 37:534–52. DOI: 10.1016/S1701-2163(15)30230-9. PMID: 26334606.18. Kaplan KM, Spivak JM, Bendo JA. 2005; Embryology of the spine and associated congenital abnormalities. Spine J. 5:564–76. DOI: 10.1016/j.spinee.2004.10.044. PMID: 16153587.19. Kumar A, Tubbs RS. 2011; Spina bifida: a diagnostic dilemma in paleopathology. Clin Anat. 24:19–33. DOI: 10.1002/ca.21058. PMID: 20949487.20. Greene ND, Copp AJ. 2014; Neural tube defects. Annu Rev Neurosci. 37:221–42. DOI: 10.1146/annurev-neuro-062012-170354. PMID: 25032496. PMCID: PMC4486472.21. Gillis CC, Eichholz K, Thoman WJ, Fessler RG. 2015; A minimally invasive approach to defects of the pars interarticularis: restoring function in competitive athletes. Clin Neurol Neurosurg. 139:29–34. DOI: 10.1016/j.clineuro.2015.08.024. PMID: 26363364.22. Wright J, Balaji V, Montgomery AS. 2013; (ii) Spondylolysis & spondylolisthesis. Orthop Trauma. 27:195–200. DOI: 10.1016/j.mporth.2013.07.002.23. Alton TB, Patel AM, Lee MJ, Chapman JR. 2014; Pediatric cervical spondylolysis and American football. Spine J. 14:e1–5. DOI: 10.1016/j.spinee.2013.09.037. PMID: 24345471.24. Haukipuro K, Keränen N, Koivisto E, Lindholm R, Norio R, Punto L. 1978; Familial occurrence of lumbar spondylolysis and spondylolisthesis. Clin Genet. 13:471–6. DOI: 10.1111/j.1399-0004.1978.tb01200.x. PMID: 668183.25. Kim HK, Laor T. 2010; Bilateral congenital cervical spondylolysis. Pediatr Radiol. 40:132. DOI: 10.1007/s00247-009-1349-8. PMID: 19629464.26. Bots J, Wijnaendts LC, Delen S, Van Dongen S, Heikinheimo K, Galis F. 2011; Analysis of cervical ribs in a series of human fetuses. J Anat. 219:403–9. DOI: 10.1111/j.1469-7580.2011.01400.x. PMID: 21689099. PMCID: PMC3171776.27. Bateson W. 2014; Materials for the study of variation treated with especial regard to discontinuity in the origin of species. Mater Study Var Treat with Espec Regard to Discontinuity Orig Species. 28:53–4. DOI: 10.5962/bhl.title.17250.28. Deepa T, John MK. 2014; A study of lumbarisation of first sacral vertebra among the South Indians. Int J Med Res Health Sci. 3:1–4. DOI: 10.5958/j.2319-5886.3.1.001.29. Jacob M, Agrawal N, Paul D. 2017; Study of additive effect of Dexmedetomidine added to epidural Ropivacaine for orthopedic lower limb procedures. Int J Biomed Res. 8:699–703.30. Konin GP, Walz DM. 2010; Lumbosacral transitional vertebrae: classification, imaging findings, and clinical relevance. AJNR Am J Neuroradiol. 31:1778–86. DOI: 10.3174/ajnr.A2036. PMID: 20203111. PMCID: PMC7964015.31. Mahato NK. 2011; Relationship of sacral articular surfaces and gender with occurrence of lumbosacral transitional vertebrae. Spine J. 11:961–5. DOI: 10.1016/j.spinee.2011.08.007. PMID: 21924685.32. Uçar BY, Uçar DE, Bulut M, Azboy İ, Demirtaş A. 2013; Lumbosacral transitional vertebrae in low back pain population. J Spine. 2:1000125. DOI: 10.4172/2165-7939.1000125.33. Sekharappa V, Amritanand R, Krishnan V, David KS. 2014; Lumbosacral transition vertebra: prevalence and its significance. Asian Spine J. 8:51–8. DOI: 10.4184/asj.2014.8.1.51. PMID: 24596605. PMCID: PMC3939369.34. Du Plessis A, Greyling L, Page B. 2018; Differentiation and classification of thoracolumbar transitional vertebrae. J Anat. 232:850–6. DOI: 10.1111/joa.12781. PMID: 29363131. PMCID: PMC5879990.35. Du Plessis A, Van Schoor A, Wessels Q, Murphy P, Van Schouwenburg F, Ihuhua P, Kehrmann J, Scholtz M, Keough N. 2022; Vertebrae at the thoracolumbar junction: a quantitative assessment using CT scans. J Anat. 240:1179–86. DOI: 10.1111/joa.13619. PMID: 34958488. PMCID: PMC9119610.36. Vasava PKG, Chaudhary SM. 2017; Lumbarization of first sacral vertebra: a case report. J Anat Soc India. 66(Suppl 1):S109. DOI: 10.1016/j.jasi.2017.08.345.37. George P, Maria T, Panagiotis K. 2013; Lumbosacral transitional vertebra associated with sacral spina bifida occulta: a case report. Acta Medica (Hradec Kralove). 56:126–9. DOI: 10.14712/18059694.2014.21. PMID: 24592751.38. Chen L, Battié MC, Yuan Y, Yang G, Chen Z, Wang Y. 2020; Lumbar vertebral endplate defects on magnetic resonance images: prevalence, distribution patterns, and associations with back pain. Spine J. 20:352–60. DOI: 10.1016/j.spinee.2019.10.015. PMID: 31669615.39. Carrino JA, Campbell PD Jr, Lin DC, Morrison WB, Schweitzer ME, Flanders AE, Eng J, Vaccaro AR. 2011; Effect of spinal segment variants on numbering vertebral levels at lumbar MR imaging. Radiology. 259:196–202. DOI: 10.1148/radiol.11081511. PMID: 21436097.40. Tague RG. 2011; Sacralization is not associated with elongated cervical costal process and cervical rib. Clin Anat. 24:209–17. DOI: 10.1002/ca.21087. PMID: 21322043.41. Tague RG. 2011; Fusion of coccyx to sacrum in humans: prevalence, correlates, and effect on pelvic size, with obstetrical and evolutionary implications. Am J Phys Anthropol. 145:426–37. DOI: 10.1002/ajpa.21518. PMID: 21541925.42. Nathan ST, Fisher BE, Roberts CS. 2010; Coccydynia: a review of pathoanatomy, aetiology, treatment and outcome. J Bone Joint Surg Br. 92:1622–7. DOI: 10.1302/0301-620X.92B12.25486. PMID: 21119164.43. Peer KS, Fascione JM. 2007; Spondylolysis: a review and treatment approach. Orthop Nurs. 26:104–11. quiz 112–3. DOI: 10.1097/01.NOR.0000265867.70479.cb. PMID: 17414379.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Arteriovenous Malformation at Cerebellopontine Angle Associated with a Fenestration of the Vertebral Artery
- Anomalous Origins of the Bilateral Vertebral Arteries Arising from the Aortic Arch: A Case Report
- Combined Anatomical Anomalies of Direct Aortic Arch Origins of the Left Internal Carotid, Left External Carotid, and Left Vertebral Arteries: A Case Report
- Spontaneous Vertebral Column Dislocation in Neurofibromatosis: A Case Report
- Embryologic Discission of the Median Raphe Cyst: Two Cases Report