Korean J Health Promot.
2022 Dec;22(4):175-182. 10.15384/kjhp.2022.22.4.175.
Changes of Body Mass Index and the Incidence of Hypertension in Late Middle Age: A Nationwide Cohort Study in South Korea
- Affiliations
-
- 1Department of Family Medicine, Seoul National University Bundang Hospital, Seongnam, Korea
- 2Department of Digital Healthcare, Seoul National University Bundang Hospital, Seongnam, Korea
- 3Health Promotion Center, Seoul National University Bundang Hospital, Seongnam, Korea
- KMID: 2537437
- DOI: http://doi.org/10.15384/kjhp.2022.22.4.175
Abstract
- Background
Previous studies revealed weight gain is an independent risk factor for hypertension. Hypertension in late middle age increases the risks of dementia and cardiovascular diseases. We aimed to analyze the difference in the risk of hypertension in the late middle age according to the change of body mass index (BMI) using nationwide cohort data of South Korea.
Methods
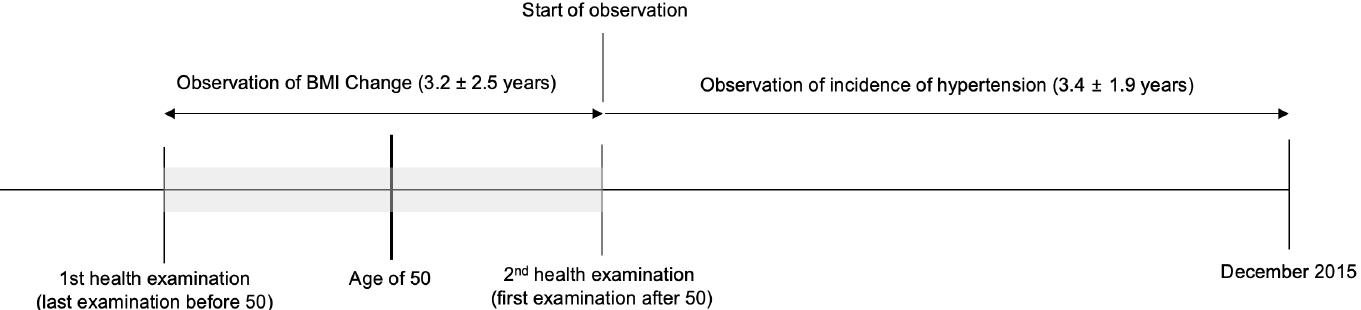
We used 64,136 individuals from National Health Insurance Service-Health Screening Cohort in South Korea. The primary endpoint is newly diagnosed hypertension after observation start date, which was defined as the date of first examination after 50. BMI changes were measured between two consecutive health examinations before and after 50. Cox proportional hazard regression analysis was performed to evaluate the association between the change of BMI and the risk of hypertension.
Results
During the mean follow-up period of 3.4±1.9 years, 8,676 individuals were diagnosed with hypertension. Both normal-to-obese group and obese-to-obese group had 19% higher risk for hypertension, and obese-to normal group had 10% higher risk for hypertension in late middle age, compared to normal-to-normal group.
Conclusions
We confirmed becoming obese and maintaining obese increase the risk of hypertension in late middle age. Thus, clinicians need to assess obese patients regularly for the possibility of new onset hypertension and take preventive measure to reduce the risk by losing weights before late middle age.
Keyword
Figure
Reference
-
1. Xie YJ, Ho SC, Su X, Liu ZM. Changes in body weight from young adulthood to middle age and its association with blood pressure and hypertension: a cross-sectional study in Hong Kong Chinese women. J Am Heart Assoc. 2016; 5(1):e002361.
Article2. Qu Y, Niu H, Li L, Li M, Yan S, Li M, et al. Analysis of dose-response relationship between BMI and hypertension in northeastern China using restricted cubic spline functions. Sci Rep. 2019; 9(1):18208.
Article3. Shihab HM, Meoni LA, Chu AY, Wang NY, Ford DE, Liang KY, et al. Body mass index and risk of incident hypertension over the life course: the Johns Hopkins precursors study. Circulation. 2012; 126(25):2983–9.
Article4. Ren Q, Su C, Wang H, Wang Z, Du W, Zhang B. Change in body mass index and its impact on incidence of hypertension in 18-65-year-old Chinese adults. Int J Environ Res Public Health. 2016; 13(3):257.
Article5. Rodriguez BL, Labarthe DR, Huang B, Lopez-Gomez J. Rise of blood pressure with age. New evidence of population differences. Hypertension. 1994; 24(6):779–85.
Article6. Lee JH, Yang DH, Park HS, Cho Y, Jun JE, Park WH, et al. Incidence of hypertension in Korea: 5-year follow-up study. J Korean Med Sci. 2011; 26(10):1286–92.
Article7. Beunza JJ, Martínez-González MA, Serrano-Martínez M, Alonso A. Incidence of hypertension in a cohort of Spanish university graduates: the SUN study. Rev Esp Cardiol. 2006; 59(12):1331–4.
Article8. Park E, Kim H. Experience of late-middle-aged women who reside in small and medium-sized cities in becoming psychologically mature women. Osong Public Health Res Perspect. 2015; 6(3):159–63.
Article9. Cockerham WC, D Wolfe J, Bauldry S. Health lifestyles in late middle age. Res Aging. 2020; 42(1):34–46.
Article10. Woolf SH, Chapman DA, Buchanich JM, Bobby KJ, Zimmerman EB, Blackburn SM. Changes in midlife death rates across racial and ethnic groups in the United States: systematic analysis of vital statistics. BMJ. 2018; 362:k3096.
Article11. Chooi YC, Ding C, Magkos F. The epidemiology of obesity. Metabolism. 2019; 92:6–10.
Article12. Walker KA, Sharrett AR, Wu A, Schneider ALC, Albert M, Lutsey PL, et al. Association of midlife to late-life blood pressure patterns with incident dementia. JAMA. 2019; 322(6):535–45.
Article13. Hughes D, Judge C, Murphy R, Loughlin E, Costello M, Whiteley W, et al. Association of blood pressure lowering with incident dementia or cognitive impairment: a systematic review and meta-analysis. JAMA. 2020; 323(19):1934–44.
Article14. Wang C, Yuan Y, Zheng M, Pan A, Wang M, Zhao M, et al. Association of age of onset of hypertension with cardiovascular diseases and mortality. J Am Coll Cardiol. 2020; 75(23):2921–30.15. Quan H, Chen G, Walker RL, Wielgosz A, Dai S, Tu K, et al. Incidence, cardiovascular complications and mortality of hypertension by sex and ethnicity. Heart. 2013; 99(10):715–21.
Article16. Zhang M, Zhao Y, Sun H, Luo X, Wang C, Li L, et al. Effect of dynamic change in body mass index on the risk of hypertension: results from the rural Chinese cohort study. Int J Cardiol. 2017; 238:117–22.
Article17. Lee HY, Lee JY, Shin HG, Cho SH, Park KI, Oh GC, et al. The Korean hypertension cohort study: design and baseline characteristics. Korean J Intern Med. 2021; 36(5):1115–25.
Article18. World Health Organization (WHO) Western Pacific Region. The Asia-pacific perspective: redefining obesity and its treatment [Internet]. Geneva: WHO Western Pacific Region;2000. [cited Nov 9, 2022]. Available from: https://apps.who.int/iris/bitstream/handle/10665/206936/0957708211_eng.pdf.19. Li W, Fang W, Huang Z, Wang X, Cai Z, Chen G, et al. Association between age at onset of overweight and risk of hypertension across adulthood. Heart. 2022; 108(9):683–8.
Article20. Forman JP, Stampfer MJ, Curhan GC. Diet and lifestyle risk factors associated with incident hypertension in women. JAMA. 2009; 302(4):401–11.
Article21. Hayashi T, Boyko EJ, Leonetti DL, McNeely MJ, Newell-Morris L, Kahn SE, et al. Visceral adiposity is an independent predictor of incident hypertension in Japanese Americans. Ann Intern Med. 2004; 140(12):992–1000.
Article22. Zhao Y, Zhang M, Luo X, Wang C, Li L, Zhang L, et al. Association of 6-year waist circumference gain and incident hypertension. Heart. 2017; 103(17):1347–52.
Article23. Jayedi A, Rashidy-Pour A, Khorshidi M, Shab-Bidar S. Body mass index, abdominal adiposity, weight gain and risk of developing hypertension: a systematic review and dose-response meta-analysis of more than 2.3 million participants. Obes Rev. 2018; 19(5):654–67.
Article24. Adair LS. Dramatic rise in overweight and obesity in adult Filipino women and risk of hypertension. Obes Res. 2004; 12(8):1335–41.
Article25. Huang Z, Willett WC, Manson JE, Rosner B, Stampfer MJ, Speizer FE, et al. Body weight, weight change, and risk for hypertension in women. Ann Intern Med. 1998; 128(2):81–8.
Article26. Diaz KM, Shimbo D. Physical activity and the prevention of hypertension. Curr Hypertens Rep. 2013; 15(6):659–68.
Article27. Lee DC, Sui X, Church TS, Lavie CJ, Jackson AS, Blair SN. Changes in fitness and fatness on the development of cardiovascular disease risk factors hypertension, metabolic syndrome, and hypercholesterolemia. J Am Coll Cardiol. 2012; 59(7):665–72.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Hypertension Prediction Analysis Using Waist Measurement and Body Mass Index by Age Group
- The Incidence and Risk Factors of Hypertension that Developed in a Male-workers' Cohort for 3 Years
- A Retrospective Cohort Study on Obesity and Hypertension Risk among Korean Adults
- Timing of Menarche and Physical Growth during Childhood and Adolescence: The Kangwha Study
- A Nested Case-Control Study on the High Normal Blood Pressure as a Risk Factor of Hypertension in Korean Middle-aged Men