J Cerebrovasc Endovasc Neurosurg.
2022 Dec;24(4):386-392. 10.7461/jcen.2022.E2021.11.002.
Right cerebellar stroke with a right vertebral artery occlusion following an embolization of the right glomus tympanicum tumor: Case report with literature review
- Affiliations
-
- 1Department of Neurology, National Neurosciences Institute, King Fahad Medical City, Riyadh, KSA
- 2Medical Imaging Administration, Neurointervention Radiology, King Fahad Medical City, Riyadh, KSA
- 3Physical Medicine, Audiology Department, King Fahad Medical City, Riyadh, KSA
- 4Critical Care Department, Neuro Critical Care Unit, King Fahad Medical City, Riyadh, KSA
- 5Department of Neurosurgery, National Neurosciences Institute, King Fahad Medical City, Riyadh, KSA
- KMID: 2537324
- DOI: http://doi.org/10.7461/jcen.2022.E2021.11.002
Abstract
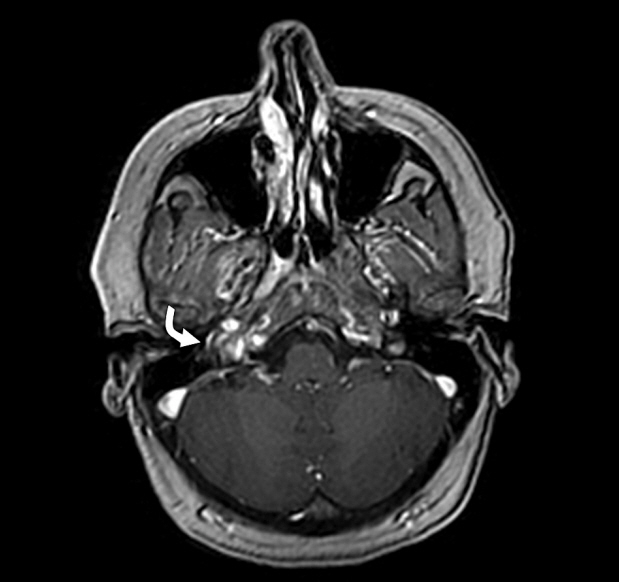
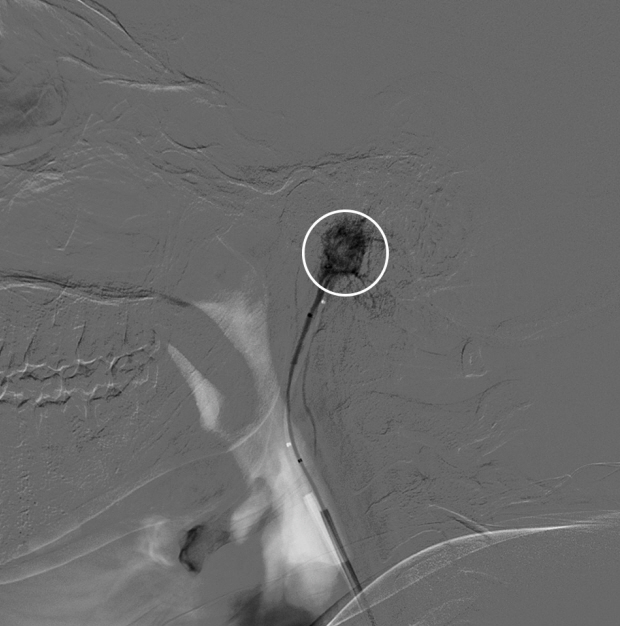
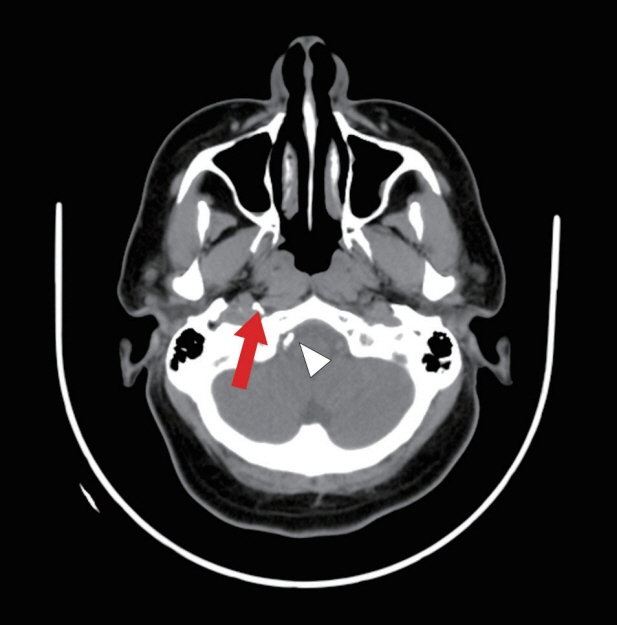
- A 35-year-old female presented with episodes of frequent dizziness, ear fullness, and right ear tinnitus for 12 months. Head imaging revealed a right glomus tympanicum tumor. She underwent pre-operative endovascular embolization of the glomus tympanicum tumor with surgical, cyanoacrylate-based glue. Immediately after the procedure, she developed drowsiness and severe pain in the right temporal region. Further investigations revealed a right cerebellar stroke in the posterior inferior cerebellar artery territory. She was treated with intravenous heparin, followed by one year of oral anticoagulation. With rehabilitation, she significantly recovered from her post embolization stroke. However, the tumor was resected at another institution. Ten years later, follow-up imaging indicated a gradual increase in the size of the glomus jugulare tumor compressing the nearby critical vascular structures. She subsequently received radiation therapy to treat the residual tumor. Currently, she has no neurological deficit, but her mild dizziness, right ear tinnitus, and hearing impairment persist.
Figure
Reference
-
1. Burdick TR, Hoffer EK, Kooy T, Ghodke B, Starnes BW, Valji K, et al. Which arteries are expendable? The practice and pitfalls of embolization throughout the body. Semin Intervent Radiol. 2008; Sep. 25(3):191–203.
Article2. Capps FCW. Glomus jugulare tumours of the middle ear. J Laryngol Otol. 1952; Jul. 66(7):302–14.
Article3. Erickson D, Kudva YC, Ebersold MJ, Thompson GB, Grant CS, van Heerden JA, et al. Benign Paragangliomas: clinical presentation and treatment outcomes in 236 patients. J Clin Endocrinol Metab. 2001; Nov. 86(11):5210–6.
Article4. Guild SR. A hitherto unrecognized structure, the glomus jugularis, in man. Anat Rec. 1941; 79(2 Suppl):28–107.5. Gupta R, Thomas AJ, Horowitz M. Intracranial head and neck tumors: endovascular considerations, present and future. Neurosurgery. 2006; Nov. 59(5 Suppl 3):S251–60. discussion S3-13.
Article6. Larson TC, Reese DF, Baker HL, McDonald TJ. Glomus tympanicum chemodectomas: radiographic and clinical characteristics. Radiology. 1987; Jun. 163(3):801–6.
Article7. Mulligan RM, Chemodectoma in the dog. Am J Pathol. 1950; 26:680–1.8. Noujaim SE, Pattekar MA, Cacciarelli A, Sanders WP, Wang AM. Paraganglioma of the temporal bone: role of magnetic resonance imaging versus computed tomography. Top Magn Reson Imaging. 2000; Apr. 11(2):108–22.
Article9. Oldring D, Fisch U. Glomus tumors of the temporal region: surgical therapy. Am J Otol. 1979; Jul. 1(1):7–18.10. Olsen WL, Dillon WP, Kelly WM, Norman D, Brant-Zawadzki M, Newton TH. MR imaging of paragangliomas. AJR Am J Roentgenol. 1987; Jan. 148(1):201–4.
Article11. Rosenwasser H. Carotid body tumor of the middle ear and mastoid. Arch Otolaryngol. 1945; 41(1):64–7.
Article12. Winship T, Godwin B, van Creveld E. Glomus jugulare tumors. Arch Chir Neerl. 1952; 4:249–54.