J Cerebrovasc Endovasc Neurosurg.
2022 Dec;24(4):356-365. 10.7461/jcen.2022.E2022.05.004.
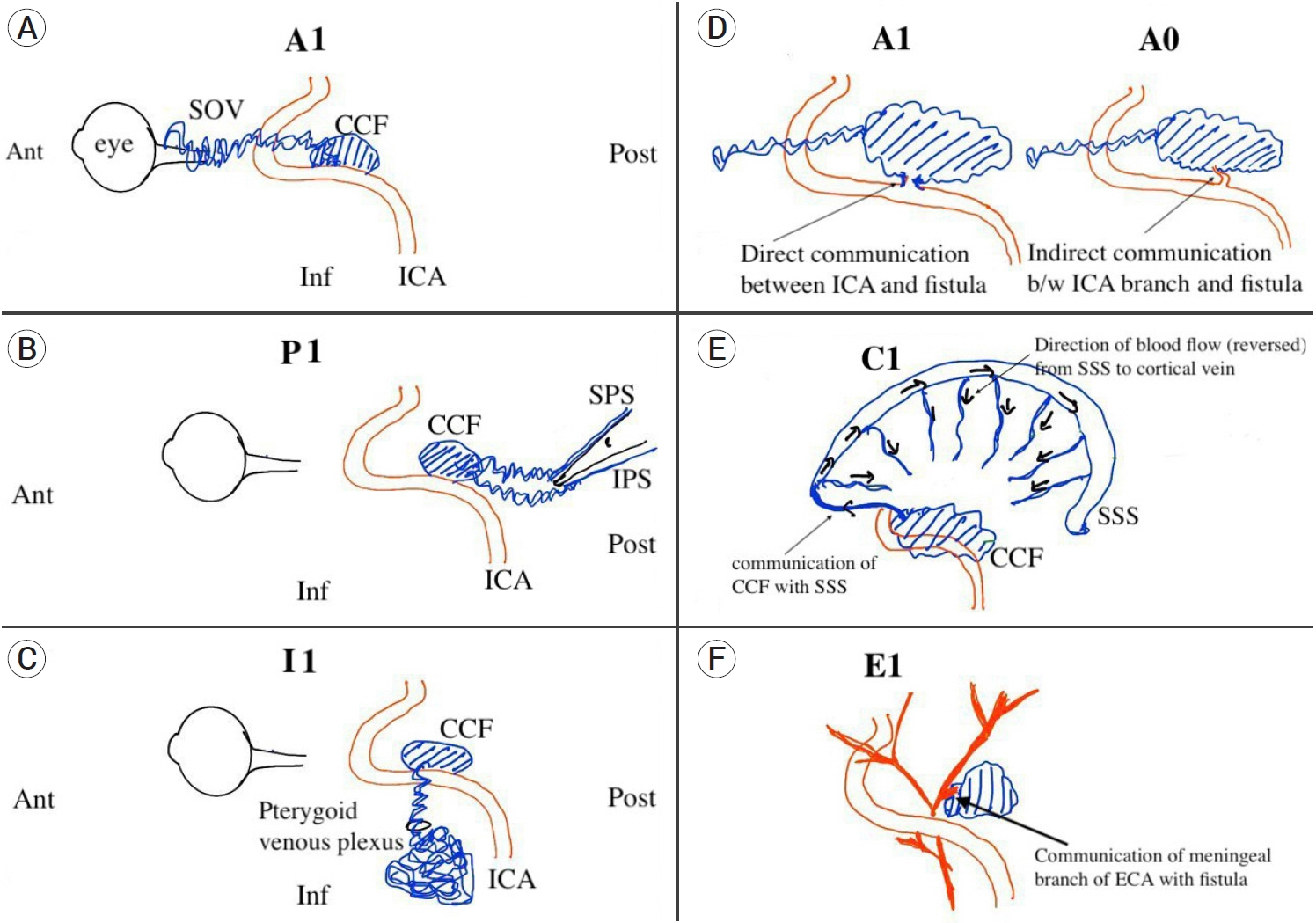
Carotid cavernous fistula: Redefining the angioarchitecture
- Affiliations
-
- 1Fellow Skull Based Surgeon, PGIMER Chandigarh, Haryana, India
- 2Department of Neurosurgery, Pt. B. D. Sharma, PGIMS Rohtak. Haryana, India
- 3Department of Community Medicine, Pt. B. D. Sharma, PGIMS Rohtak. Haryana, India
- 4Department of Neurosurgery, SMS Medical College and Hospital, Jaipur, Rajasthan, India
- 5Department of Neurology, SMS Medical College and Hospital, Jaipur, Rajasthan, India
- KMID: 2537320
- DOI: http://doi.org/10.7461/jcen.2022.E2022.05.004
Abstract
Objective
Numerous classification schemes have been used for carotid cavernous fistula (CCF), each describing some aspect of the disease process but none of them provides a complete description of the fistula including its clinical features, natural history, arterial and venous architecture.
Methods
Retrospective clinical and radiological review was done for all the patients diagnosed with CCF and treated at our institute. The CCF were classified according to the proposed API-ACE classification along with Barrow and Thomas classification.
Results
Overall 28 patients (M=21, F=7) were diagnosed and treated during the 6-year period. 89.2% of CCF developed following an episode of head injury. Orbital symptoms were the most common presenting complaints. Barrows type A was the most predominant subtype (n=24) and most of the patients (n=23) demonstrated decreased ipsilateral carotid filling. Combined anterior and posterior drainage pattern was the most common drainage pattern and anterior drainage was more commonly observed than posterior drainage.
Conclusions
API-ACE classification helps to better understand and classify the angioarchitecture of CCF which could help better understand the clinical manifestations and guide in appropriate endovascular approach selection for treatment.
Figure
Reference
-
1. Abecassis IJ, Morton RP, Kim LJ, Ghodke BV, Levitt MR. Combined direct and indirect traumatic carotid-cavernous fistula (CCF): case report and review of the literature. J Clin Neurosci. 2017; Oct. 44:240–42.
Article2. Alam MS, Jain M, Mukherjee B, Sharma T, Halbe S, Jaisankar D, et al. Visual impairment in high flow and low flow carotid cavernous fistula. Sci Rep. 2019; 9(1):12872.
Article3. Barrow DL, Spector RH, Braun IF, Landman JA, Tindall SC, Tindall GT. Classification and treatment of spontaneous carotid-cavernous sinus fistulas. J Neurosurg. 1985; Feb. 62(2):248–56.
Article4. Borden JA, Wu JK, Shucart WA. A proposed classification for spinal and cranial dural arteriovenous fistulous malformations and implications for treatment. J Neurosurg. 1995; Feb. 82(2):166–79.
Article5. Chi CT, Nguyen D, Duc VT, Chau HH, Son VT. Direct traumatic carotid cavernous fistula: angiographic classification and treatment strategies. Study of 172 cases. Interv Neuroradiol. 2014; Jul-Aug. 20(4):461–75.
Article6. Cognard C, Gobin YP, Pierot L, Bailly AL, Houdart E, Casasco A, et al. Cerebral dural arteriovenous fistulas: clinical and angiographic correlation with a revised classification of venous drainage. Radiology. 1995; Mar. 194(3):671–80.
Article7. Debrun GM. Angiographic workup of a carotid cavernous sinus fistula (CCF) or what information does the interventionalist need for treatment? Surg Neurol. 1995; Jul. 44(1):75–9.
Article8. Francis PM, Khayata MH, Zabramski JM, Spetzler RF. Carotid cavernous fistulae. Part 1: Presentation and features, in Carter LP, Spetzler RF (ed.) Neurovascular Surgery. New York: McGraw-Hill 1995. p. 1049-59.9. Jung KH, Kwon BJ, Chu K, Noh Y, Lee ST, Cho YD, et al. Clinical and angiographic factors related to the prognosis of cavernous sinus dural arteriovenous fistula. Neuroradiology. 2011; 53(12):983–92.
Article10. Leone G, Renieri L, Enriquez-Marulanda A, Dmytriw AA, Nappini S, Laiso A, et al. Carotid cavernous fistulas and dural arteriovenous fistulas of the cavernous sinus: validation of a new classification according to venous drainage. World Neurosurg. 2019; Aug. 128:e621–31.
Article11. Malan J, Lefeuvre D, Mngomezulu V, Taylor A. Angioarchitecture and treatment modalities in posttraumatic carotid cavernous fistulae. Interv Neuroradiol. 2012; Jun. 18(2):178–86.
Article12. Ringer AJ, Salud L, Tomsick TA. Carotid cavernous fistulas: anatomy, classification, and treatment. Neurosurg Clin N Am. 2005; Apr. 16(2):279–95. viii.
Article13. Thomas AJ, Chua M, Fusco M, Ogilvy CS, Tubbs RS, Harrigan MR, et al. Proposal of venous drainage-based classification system for carotid cavernous fistulae with validity assessment in a multicenter cohort. Neurosurgery. 2015; Sep. 77(3):380–5. discussion 385.
Article14. Winn HR. Youmans and Winn Neurological Surgery. Philadelpia: Elsevier;2017. p. 3525–29.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Bilateral Traumatic Carotid-Cavernous Fistula
- Traumatic Carotid-cavernous Fistula Bringing about Intracerebral Hemorrhage
- A Case of Dural Carotid-Cavernous Sinus Fistula Associated with Ophthalmic Manifestations
- Dural Carotid-Cavernous Sinus Fistula
- A Case of Spontaneous of Traumatic Carotid Cavernous Fistula After Carotid Angiography