J Korean Med Sci.
2022 Dec;37(50):e347. 10.3346/jkms.2022.37.e347.
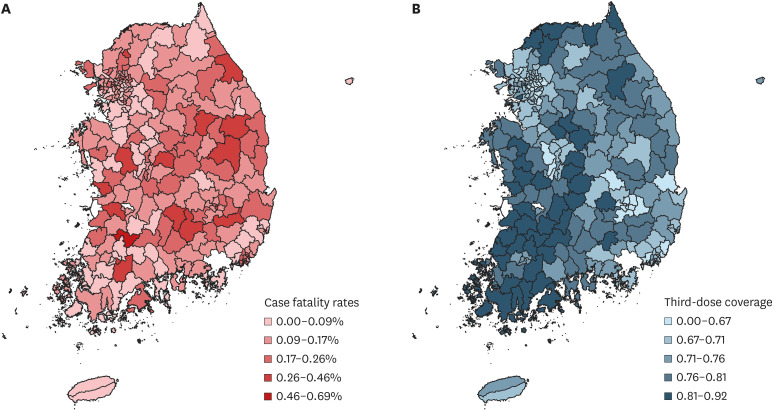
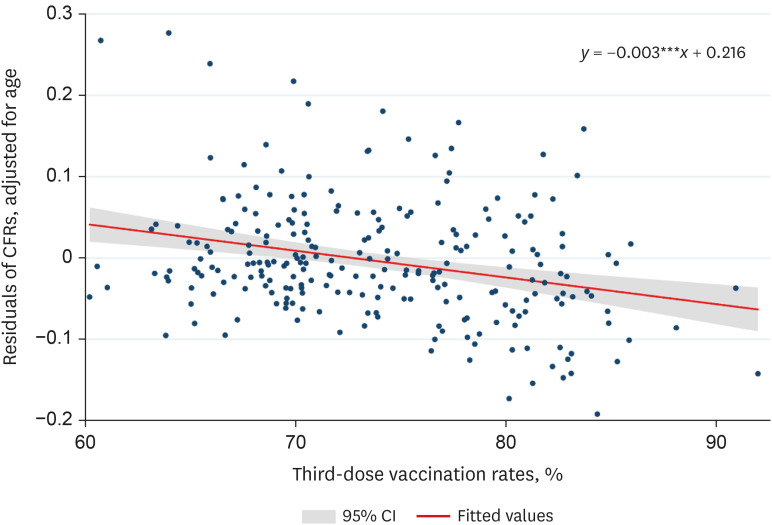
Correlation Between Third Dose of COVID-19 Vaccines and Regional Case Fatality Rates During the Omicron Wave in Korea
- Affiliations
-
- 1Center for Area Studies, Korea Institute for International Economic Policy, Sejong, Korea
- 2Department of Pathology, Labcorp Drug Development, Greenfield, IN, USA
- 3Division of Viral Diseases, Centers for Disease Control and Prevention, Atlanta, GA, USA
- 4Division of Infectious Disease, Department of Internal Medicine, Korea University Anam Hospital, Seoul, Korea
- 5Division of Infectious Disease, Department of Internal Medicine, Hallym University Kangnam Sacred Heart Hospital, Seoul, Korea
- KMID: 2537050
- DOI: http://doi.org/10.3346/jkms.2022.37.e347
Abstract
- This study seeks to find the correlation between case fatality rates (CFRs) and third-dose vaccination coverage in 244 counties (si/gun/gu) of South Korea during the omicron variant wave. Multivariate regression analyses report that the higher third-dose vaccination rates were correlated with lower regional CFRs, when controlling for age structure. If the thirddose vaccination rate of a county is higher by 10%, it would have a CFR lower by 0.05% (95% confidence interval, 0.03–0.08%). As the number of cumulative confirmed cases in South Korea was 16,353,495 as of April 20, 2022, a lower CFR by 0.03–0.08% is equivalent to 4,394–12,448 lives (8.6–24.4 per 100,000) spared. County-specific characteristics, such as age structure, intensive care unit availability, and the level of non-pharmaceutical interventions may also affect the extent of this correlation. The conclusion implicates the potential role of coronavirus disease 2019 vaccines in reducing the pressure on the regional healthcare capacity.
Keyword
Figure
Reference
-
1. Kim J, Choe YJ, Jang EJ, Lim DS, Kim YY, Kim RK, et al. Effectiveness of booster mRNA vaccines against SARS-CoV-2 infection in an elderly population, South Korea, October 2021-January 2022. Clin Infect Dis. 2022; 75(5):920–921. PMID: 35439294.2. Thompson MG, Natarajan K, Irving SA, Rowley EA, Griggs EP, Gaglani M, et al. Effectiveness of a third dose of mRNA vaccines against COVID-19-associated emergency department and urgent care encounters and hospitalizations among adults during periods of delta and omicron variant predominance - VISION Network, 10 States, August 2021-January 2022. MMWR Morb Mortal Wkly Rep. 2022; 71(4):139–145. PMID: 35085224.3. Andrews N, Stowe J, Kirsebom F, Toffa S, Sachdeva R, Gower C, et al. Effectiveness of COVID-19 booster vaccines against COVID-19-related symptoms, hospitalization and death in England. Nat Med. 2022; 28(4):831–837. PMID: 35045566.4. Asian Development Bank. The Republic of Korea’s Coronavirus Disease Pandemic Response and Health System Preparedness. Metro Manila, Philippines: Asian Development Bank;2021. p. 66.5. Korea Disease Control and Prevention Agency. COVID-19 vaccination. Accessed April 21, 2022. https://ncv.kdca.go.kr/ .6. Ministry of Health and Welfare. Coronavirus (COVID-19), Republic of Korea. Accessed April 21, 2022. https://ncov.kdca.go.kr/ .7. Dong E, Du H, Gardner L. COVID-19 Content Portal. Accessed April 20, 2022. https://systems.jhu.edu/research/public-health/ncov/ .8. Cho HJ. Equity in health care: current situation in South Korea. J Korean Med Assoc. 2013; 56(3):184–194.9. Pažitný P, Kandilaki D, Mužik R, Benková B. COVID-19 case fatality rate in the context of healthcare system organization and EHCI performance: focus on the Visegrad (V4) countries. Acta Oecon. 2021; 71(S1):35–52.10. Lee SH, Park SY, Seon JY, Jeon WH, Nam SI, Park JH, et al. Intensive care unit capacity and its associated risk factors during the COVID-19 surge in the Republic of Korea: analysis using nationwide health claims data. Risk Manag Healthc Policy. 2020; 13:2571–2581. PMID: 33209067.11. Kim JH, Hong SK, Kim Y, Ryu HG, Park CM, Lee YS, et al. Experience of augmenting critical care capacity in Daegu during COVID-19 incident in South Korea. Acute Crit Care. 2020; 35(2):110–114. PMID: 32506876.12. Jo Y, Shrestha S, Radnaabaatar M, Park H, Jung J. Optimal social distancing policy for COVID-19 control in Korea: a model-based analysis. J Korean Med Sci. 2022; 37(23):e189. PMID: 35698839.13. Park IN, Yum HK. Stepwise strategy of social distancing in Korea. J Korean Med Sci. 2020; 35(28):e264. PMID: 32686376.14. Ministry of Health and Welfare Press Release. Adjustment of social distancing levels considering regional situation. Updated July 14, 2021. Accessed October 10, 2022. http://www.mohw.go.kr/react/al/sal0301vw.jsp?PAR_MENU_ID=04&MENU_ID=0403&page=1&CONT_SEQ=366435 .15. McLaughlin JM, Khan F, Pugh S, Swerdlow DL, Jodar L. County-level vaccination coverage and rates of COVID-19 cases and deaths in the United States: an ecological analysis. Lancet Reg Health Am. 2022; 9:100191. PMID: 35128511.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of the Clinical and Laboratory Features of COVID-19 in Children During All Waves of the Epidemic: A Single Center Retrospective Study
- Mathematical modeling of the impact of Omicron variant on the COVID-19 situation in South Korea
- Seizure Incidence among Children Hospitalized with COVID-19 during the Omicron Wave
- mRNA COVID-19 Vaccine-Associated Subserosal Eosinophilic Gastroenteritis: A Case Report
- The Impact of Omicron Wave on Pediatric Febrile Seizure