J Korean Med Sci.
2022 Dec;37(50):e346. 10.3346/jkms.2022.37.e346.
Demographic and Genome Wide Association Analyses According to Muscle Mass Using Data of the Korean Genome and Epidemiology Study
- Affiliations
-
- 1Medical Science Research Center, College of Medicine, Korea University, Seoul, Korea
- 2Department of Biomedical Research Institute, Gyeongsang National University Hospital, Jinju, Korea
- 3Department of Theriogenology and Biotechnology, College of Veterinary Medicine, Gyeongsang National University, Jinju, Korea
- 4Department of Biostatistics Cooperation Center, Gyeongsang National University Hospital, Jinju, Korea
- 5Department of Physical Education, Gyeongsang National University, Jinju, Korea
- 6Research Institute of Pharmaceutical Sciences, Gyeongsang National University, Jinju, Korea
- 7Department of Orthopaedic Surgery, Gyeongsang National University Hospital, Jinju, Korea
- KMID: 2537049
- DOI: http://doi.org/10.3346/jkms.2022.37.e346
Abstract
- Background
Sarcopenia is commonly found in the elderly due to a decline in muscle mass. Many researchers have performed genome-wide association studies (GWAS) to find genetic risk factors of sarcopenia. Although many studies have discovered sarcopenia associated single nucleotide polymorphisms (SNPs), most of them are studies targeting Caucasians. The purpose of this study was to evaluate genetic correlation according to muscle mass in middle aged Koreans using data of the Korean Genome and Epidemiology Study (KOGES), a large population-based genomic cohort study.
Methods
Baseline participants were 10,030 subjects aged 40 to 69 years who were from Ansan or Anseong in Gyeonggi-do, South Korea. Among them, 9,351 subjects with laboratory data available were included in this study. To identify sarcopenia associated variants, those in the top 30% and bottom 30% of muscle mass index (MMI) were compared. A total of 7,452 people with an MMI of 30-70% were excluded. A total of 1,004 people were also excluded due to missing data. Finally, 895 people were selected for this study. The Korea Biobank Array generated 500,568 SNPs for this dataset.
Results
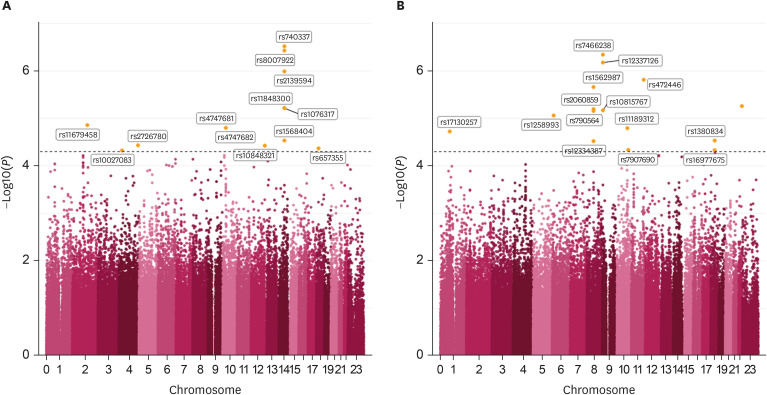
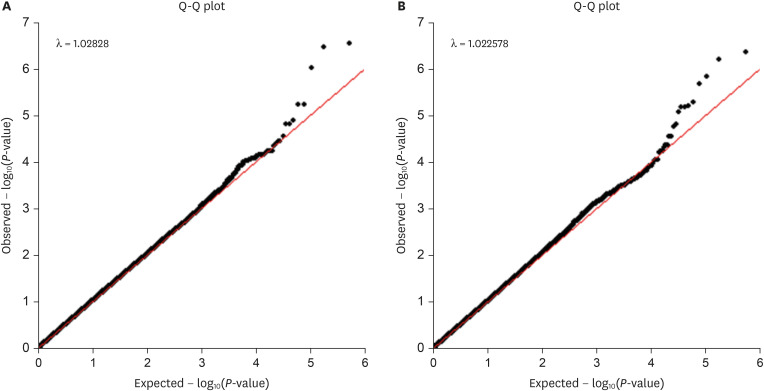
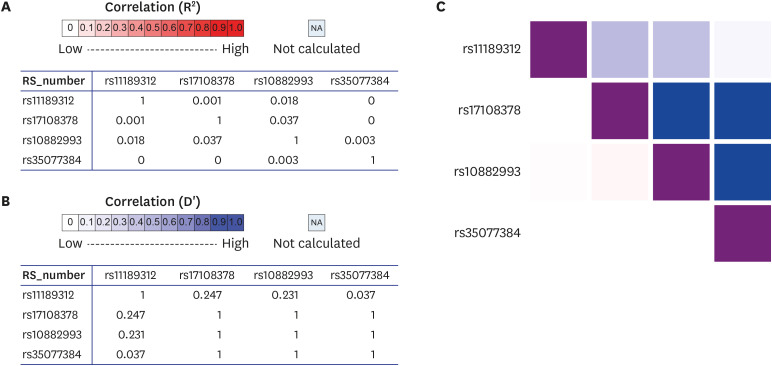
When subjects were divided into top 30% and bottom 30% of MMI, the top 30% had 169 men and 308 women and the bottom 30% had 220 men and 198 women. In men, age, body mass index (BMI), waist and hip were significantly (P < 0.005) different between top 30% and bottom 30% MMI groups. In women, age, BMI, waist, hip, and hypertension history were significantly different between the two MMI groups. There were 13 significant SNPs in men and 14 significant SNPs in women. Genes associated with variants in men based on the single-nucleotide polymorphism database (dbSNP) were LRP1B containing rs11679458 and RGS6 containing rs11848300. A gene associated with variants in women was Pi4K2A, which contained rs1189312 as a variant. In addition, rs11189312 was associated with expression quantitative trait loci (eQTL) of ZFYVE27 in skeletal muscles and other SNPs of ZFYVE27 (rs10882883, rs17108378, rs35077384) known to be associated with spastic paraplegia. The eQTL analysis revealed that rs11189312 was a variant associated with SNPs of ZFYVE27.
Conclusions
In the demographic study, significant results were found in BMI, waist, hip, history of hyperlipidemia, and sedentary life status in male group, and significant results were found in BMI, waist, hip, and hypertension history in female group. Variant rs11189312 was found to be a novel variant affecting ZFYVE27 expressed in skeletal muscles, suggesting that rs11189312 might be related to sarcopenia as a novel discovery of this study. Further study is needed to determine the association between sarcopenia and ZFYVE27 known to be associated with spastic paraplegia.
Keyword
Figure
Reference
-
1. Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019; 48(1):16–31. PMID: 30312372.2. Bijlsma AY, Meskers CG, Ling CH, Narici M, Kurrle SE, Cameron ID, et al. Defining sarcopenia: the impact of different diagnostic criteria on the prevalence of sarcopenia in a large middle aged cohort. Age (Dordr). 2013; 35(3):871–881. PMID: 22314402.3. Ryan AS, Ivey FM, Serra MC, Hartstein J, Hafer-Macko CE. Sarcopenia and physical function in middle-aged and older stroke survivors. Arch Phys Med Rehabil. 2017; 98(3):495–499. PMID: 27530769.4. Walrand S, Guillet C, Salles J, Cano N, Boirie Y. Physiopathological mechanism of sarcopenia. Clin Geriatr Med. 2011; 27(3):365–385. PMID: 21824553.5. Meng SJ, Yu LJ. Oxidative stress, molecular inflammation and sarcopenia. Int J Mol Sci. 2010; 11(4):1509–1526. PMID: 20480032.6. Pereira RA, Cordeiro AC, Avesani CM, Carrero JJ, Lindholm B, Amparo FC, et al. Sarcopenia in chronic kidney disease on conservative therapy: prevalence and association with mortality. Nephrol Dial Transplant. 2015; 30(10):1718–1725. PMID: 25999376.7. Umegaki H. Sarcopenia and diabetes: hyperglycemia is a risk factor for age-associated muscle mass and functional reduction. J Diabetes Investig. 2015; 6(6):623–624.8. Cesari M, Kritchevsky SB, Baumgartner RN, Atkinson HH, Penninx BW, Lenchik L, et al. Sarcopenia, obesity, and inflammation--results from the Trial of Angiotensin Converting Enzyme Inhibition and Novel Cardiovascular Risk Factors study. Am J Clin Nutr. 2005; 82(2):428–434. PMID: 16087989.9. Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, et al. Sarcopenia: European consensus on definition and diagnosis: report of the European Working Group on Sarcopenia in Older People. Age Ageing. 2010; 39(4):412–423. PMID: 20392703.10. Kim TN, Choi KM. Sarcopenia: definition, epidemiology, and pathophysiology. J Bone Metab. 2013; 20(1):1–10. PMID: 24524049.11. Gensous N, Bacalini MG, Franceschi C, Meskers CG, Maier AB, Garagnani P. Age-related DNA methylation changes: potential impact on skeletal muscle aging in humans. Front Physiol. 2019; 10:996. PMID: 31427991.12. Sun G, Gagnon J, Chagnon YC, Pérusse L, Després JP, Leon AS, et al. Association and linkage between an insulin-like growth factor-1 gene polymorphism and fat free mass in the HERITAGE Family Study. Int J Obes. 1999; 23(9):929–935.13. Huygens W, Thomis MA, Peeters MW, Aerssens J, Janssen R, Vlietinck RF, et al. Linkage of myostatin pathway genes with knee strength in humans. Physiol Genomics. 2004; 17(3):264–270. PMID: 15026560.14. Windelinckx A, De Mars G, Huygens W, Peeters MW, Vincent B, Wijmenga C, et al. Comprehensive fine mapping of chr12q12-14 and follow-up replication identify activin receptor 1B (ACVR1B) as a muscle strength gene. Eur J Hum Genet. 2011; 19(2):208–215. PMID: 21063444.15. Hopkinson NS, Nickol AH, Payne J, Hawe E, Man WD, Moxham J, et al. Angiotensin converting enzyme genotype and strength in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2004; 170(4):395–399. PMID: 15117739.16. Wagner H, Thaller S, Dahse R, Sust M. Biomechanical muscle properties and angiotensin-converting enzyme gene polymorphism: a model-based study. Eur J Appl Physiol. 2006; 98(5):507–515. PMID: 17006713.17. Yoshihara A, Tobina T, Yamaga T, Ayabe M, Yoshitake Y, Kimura Y, et al. Physical function is weakly associated with angiotensin-converting enzyme gene I/D polymorphism in elderly Japanese subjects. Gerontology. 2009; 55(4):387–392. PMID: 19478476.18. Pescatello LS, Kostek MA, Gordish-Dressman H, Thompson PD, Seip RL, Price TB, et al. ACE ID genotype and the muscle strength and size response to unilateral resistance training. Med Sci Sports Exerc. 2006; 38(6):1074–1081. PMID: 16775548.19. Rodríguez-Romo G, Ruiz JR, Santiago C, Fiuza-Luces C, González-Freire M, Gómez-Gallego F, et al. Does the ACE I/D polymorphism, alone or in combination with the ACTN3 R577X polymorphism, influence muscle power phenotypes in young, non-athletic adults? Eur J Appl Physiol. 2010; 110(6):1099–1106. PMID: 20734058.20. Bustamante-Ara N, Santiago C, Verde Z, Yvert T, Gómez-Gallego F, Rodríguez-Romo G, et al. ACE and ACTN3 genes and muscle phenotypes in nonagenarians. Int J Sports Med. 2010; 31(4):221–224. PMID: 20148371.21. Yang N, MacArthur DG, Gulbin JP, Hahn AG, Beggs AH, Easteal S, et al. ACTN3 genotype is associated with human elite athletic performance. Am J Hum Genet. 2003; 73(3):627–631. PMID: 12879365.22. Roth SM, Walsh S, Liu D, Metter EJ, Ferrucci L, Hurley BF. The ACTN3 R577X nonsense allele is under-represented in elite-level strength athletes. Eur J Hum Genet. 2008; 16(3):391–394. PMID: 18043716.23. Geusens P, Vandevyver C, Vanhoof J, Cassiman JJ, Boonen S, Raus J. Quadriceps and grip strength are related to vitamin D receptor genotype in elderly nonobese women. J Bone Miner Res. 1997; 12(12):2082–2088. PMID: 9421241.24. Wang P, Ma LH, Wang HY, Zhang W, Tian Q, Cao DN, et al. Association between polymorphisms of vitamin D receptor gene ApaI, BsmI and TaqI and muscular strength in young Chinese women. Int J Sports Med. 2006; 27(3):182–186. PMID: 16541372.25. Bahat G, Saka B, Erten N, Ozbek U, Coskunpinar E, Yildiz S, et al. BsmI polymorphism in the vitamin D receptor gene is associated with leg extensor muscle strength in elderly men. Aging Clin Exp Res. 2010; 22(3):198–205. PMID: 20634643.26. Ran S, He X, Jiang ZX, Liu Y, Zhang YX, Zhang L, et al. Whole-exome sequencing and genome-wide association studies identify novel sarcopenia risk genes in Han Chinese. Mol Genet Genomic Med. 2020; 8(8):e1267. PMID: 32478482.27. Singh AN, Gasman B. Disentangling the genetics of sarcopenia: prioritization of NUDT3 and KLF5 as genes for lean mass & HLA-DQB1-AS1 for hand grip strength with the associated enhancing SNPs & a scoring system. BMC Med Genet. 2020; 21(1):40. PMID: 32093658.28. Wannamethee SG, Atkins JL. Muscle loss and obesity: the health implications of sarcopenia and sarcopenic obesity. Proc Nutr Soc. 2015; 74(4):405–412. PMID: 25913270.29. Nagano A, Wakabayashi H, Maeda K, Kokura Y, Miyazaki S, Mori T, et al. Respiratory sarcopenia and sarcopenic respiratory disability: concepts, diagnosis, and treatment. J Nutr Health Aging. 2021; 25(4):507–515. PMID: 33786569.30. Benz IG, Trajanoska K, Schoufour J, Lahousse L, Roos ED, Terzikhan N, et al. Sarcopenia in elderly population with chronic respiratory diseases: a population-based study. Eur Respir J. 2018; 52(Suppl 62):PA1174.31. Narici MV, Maffulli N. Sarcopenia: characteristics, mechanisms and functional significance. Br Med Bull. 2010; 95(1):139–159. PMID: 20200012.32. Larsson L, Degens H, Li M, Salviati L, Lee YI, Thompson W, et al. Sarcopenia: aging-related loss of muscle mass and function. Physiol Rev. 2019; 99(1):427–511. PMID: 30427277.33. Shorter E, Sannicandro AJ, Poulet B, Goljanek-Whysall K. Skeletal muscle wasting and its relationship with osteoarthritis: a mini-review of mechanisms and current interventions. Curr Rheumatol Rep. 2019; 21(8):40. PMID: 31203463.34. Tanaga K, Bujo H, Zhu Y, Kanaki T, Hirayama S, Takahashi K, et al. LRP1B attenuates the migration of smooth muscle cells by reducing membrane localization of urokinase and PDGF receptors. Arterioscler Thromb Vasc Biol. 2004; 24(8):1422–1428. PMID: 15166012.35. Ahlers-Dannen KE, Yang J, Spicer MM, Maity B, Stewart A, Koland JG, et al. Protein profiling of RGS6, a pleiotropic gene implicated in numerous neuropsychiatric disorders, reveals multi-isoformic expression and a novel brain-specific isoform. eNeuro. 2022; 9(1):ENEURO.0379-21.2021.36. Simons JP, Al-Shawi R, Minogue S, Waugh MG, Wiedemann C, Evangelou S, et al. Loss of phosphatidylinositol 4-kinase 2α activity causes late onset degeneration of spinal cord axons. Proc Natl Acad Sci U S A. 2009; 106(28):11535–11539. PMID: 19581584.37. Deschenes MR, Roby MA, Eason MK, Harris MB. Remodeling of the neuromuscular junction precedes sarcopenia related alterations in myofibers. Exp Gerontol. 2010; 45(5):389–393. PMID: 20226849.38. Tamaki T, Hirata M, Uchiyama Y. Qualitative alteration of peripheral motor system begins prior to appearance of typical sarcopenia syndrome in middle-aged rats. Front Aging Neurosci. 2014; 6:296. PMID: 25400579.39. Tintignac LA, Brenner HR, Rüegg MA. Mechanisms regulating neuromuscular junction development and function and causes of muscle wasting. Physiol Rev. 2015; 95(3):809–852. PMID: 26109340.40. Qiu J. A new role for spastin. Nat Rev Neurosci. 2004; 5(9):673.41. Andrews HK, Zhang YQ, Trotta N, Broadie K. Drosophila sec10 is required for hormone secretion but not general exocytosis or neurotransmission. Traffic. 2002; 3(12):906–921. PMID: 12453153.42. Vemu A, Szczesna E, Zehr EA, Spector JO, Grigorieff N, Deaconescu AM, et al. Severing enzymes amplify microtubule arrays through lattice GTP-tubulin incorporation. Science. 2018; 361(6404):eaau1504. PMID: 30139843.43. Kuo YW, Trottier O, Mahamdeh M, Howard J. Spastin is a dual-function enzyme that severs microtubules and promotes their regrowth to increase the number and mass of microtubules. Proc Natl Acad Sci U S A. 2019; 116(12):5533–5541. PMID: 30837315.44. Park SH, Zhu PP, Parker RL, Blackstone C. Hereditary spastic paraplegia proteins REEP1, spastin, and atlastin-1 coordinate microtubule interactions with the tubular ER network. J Clin Invest. 2010; 120(4):1097–1110. PMID: 20200447.45. Errico A, Ballabio A, Rugarli EI. Spastin, the protein mutated in autosomal dominant hereditary spastic paraplegia, is involved in microtubule dynamics. Hum Mol Genet. 2002; 11(2):153–163. PMID: 11809724.46. Sanderson CM, Connell JW, Edwards TL, Bright NA, Duley S, Thompson A, et al. Spastin and atlastin, two proteins mutated in autosomal-dominant hereditary spastic paraplegia, are binding partners. Hum Mol Genet. 2006; 15(2):307–318. PMID: 16339213.47. Mannan AU, Krawen P, Sauter SM, Boehm J, Chronowska A, Paulus W, et al. ZFYVE27 (SPG33), a novel spastin-binding protein, is mutated in hereditary spastic paraplegia. Am J Hum Genet. 2006; 79(2):351–357. PMID: 16826525.48. Stenmark H, Aasland R, Driscoll PC. The phosphatidylinositol 3-phosphate-binding FYVE finger. FEBS Lett. 2002; 513(1):77–84. PMID: 11911884.49. Stenmark H, Aasland R. FYVE-finger proteins--effectors of an inositol lipid. J Cell Sci. 1999; 112(Pt 23):4175–4183. PMID: 10564636.50. Jung Y, Huang JZ, Hu J. Biomarker detection in association studies: modeling SNPs simultaneously via logistic ANOVA. J Am Stat Assoc. 2014; 109(508):1355–1367. PMID: 25642005.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Short History of the Genome-Wide Association Study: Where We Were and Where We Are Going
- Gene Set Analyses of Genome-Wide Association Studies on 49 Quantitative Traits Measured in a Single Genetic Epidemiology Dataset
- IVAG: An Integrative Visualization Application for Various Types of Genomic Data Based on R-Shiny and the Docker Platform
- Genome-Wide Association Study of Hepatitis in Korean Populations
- Genome-Wide Architecture of East Asian Patients With Migraine: A Genome-Wide Association Study Based on Familial History