J Korean Med Sci.
2022 Dec;37(49):e354. 10.3346/jkms.2022.37.e354.
Effects of Socioeconomic Status and Residence Areas on Long-Term Survival in Patients With Early-Onset Dementia: The Korean National Health Insurance Service Database Study
- Affiliations
-
- 1Department of Rehabilitation Medicine, Pohang Stroke and Spine Hospital, Pohang, Korea
- 2Department of Medical Science and Engineering, School of Convergence Science and Technology, Pohang University of Science and Technology, Pohang, Korea
- 3Department of Research and Analysis, National Health Insurance Service Ilsan Hospital, Goyang, Korea
- 4Department of Biostatistics and Computing, Yonsei University Graduate School, Seoul, Korea
- 5Department of Neurology, Pohang Stroke and Spine Hospital, Pohang, Korea
- 6Department of Neurology, National Health Insurance Service Ilsan Hospital, Goyang, Korea
- 7Department of Physical Medicine and Rehabilitation, National Health Insurance Service Ilsan Hospital, Goyang, Korea
- KMID: 2537048
- DOI: http://doi.org/10.3346/jkms.2022.37.e354
Abstract
- Background
Early-onset dementia (EOD) is still insufficiently considered for healthcare policies. We investigated the effect of socio-environmental factors on the long-term survival of patients with EOD.
Methods
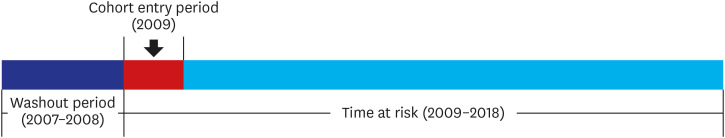
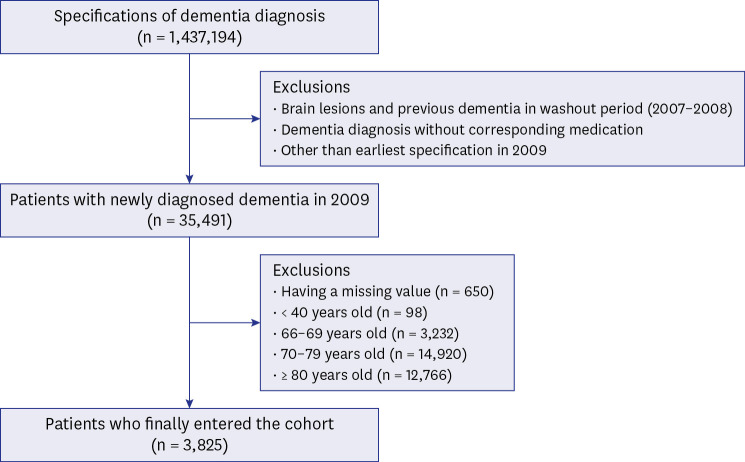
This retrospective cohort study utilized the Korean National Health Insurance Database from 2007 to 2018. We enrolled 3,825 patients aged 40 to 65 years old with all types of dementia newly diagnosed in 2009 as EOD cases. We defined socioeconomic status using the national health insurance premium (NHIP) levels. Residential areas were classified into capital, metropolitan, city, and county levels. All-cause mortality was the primary outcome. Kaplan-Meier curves and log-rank tests were employed. Further, Cox-proportional hazards models were established.
Results
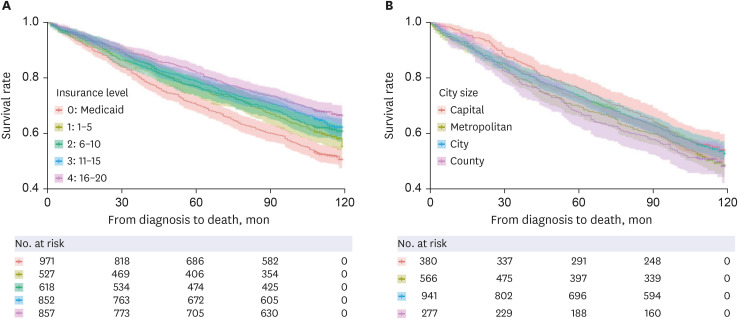
The mean survival of the fourth NHIP level group was 96.31 ± 1.20 months, whereas that of the medical-aid group was 85.53 ± 1.30 months (P < 0.001). The patients living in the capital had a mean survival of 95.73 ± 1.34 months, whereas those living in the county had 89.66 ± 1.75 months (P = 0.035). In the Cox-proportional hazards model, the medical-aid (adjusted hazard ratio [aHR], 1.67; P < 0.001), first NHIP level (aHR, 1.26; P = 0.012), and second NHIP level (aHR, 1.26; P = 0.008) groups were significantly associated with a higher long-term mortality risk. The capital residents exhibited a significantly lower long-term mortality risk than did the county residents (aHR, 0.82; P = 0.041).
Conclusion
Socioeconomic status and residential area are associated with long-term survival in patients with EOD. This study provides a rational basis for establishing a healthcare policy for patients with EOD.
Figure
Reference
-
1. Giannakopoulos P, Hof PR, Savioz A, Guimon J, Antonarakis SE, Bouras C. Early-onset dementias: clinical, neuropathological and genetic characteristics. Acta Neuropathol. 1996; 91(5):451–465. PMID: 8740225.2. Harvey RJ, Rossor MN. Does early-onset Alzheimer disease constitute a distinct subtype? The contribution of molecular genetics. Alzheimer Dis Assoc Disord. 1995; 9(Suppl 1):S7–13. PMID: 7546599.3. Moschetti K, Barragan N, Basurto-Dávila R, Cummings PL, Sorvillo F, Kuo T. Mortality and productivity losses from Alzheimer disease among US adults aged 40 to 64 years, 1999 to 2010. Alzheimer Dis Assoc Disord. 2015; 29(2):165–168. PMID: 24445567.4. Vieira RT, Caixeta L, Machado S, Silva AC, Nardi AE, Arias-Carrión O, et al. Epidemiology of early-onset dementia: a review of the literature. Clin Pract Epidemol Ment Health. 2013; 9(1):88–95.5. Kelley BJ, Boeve BF, Josephs KA. Young-onset dementia: demographic and etiologic characteristics of 235 patients. Arch Neurol. 2008; 65(11):1502–1508. PMID: 19001170.6. Werner P, Stein-Shvachman I, Korczyn AD. Early onset dementia: clinical and social aspects. Int Psychogeriatr. 2009; 21(4):631–636. PMID: 19470199.7. Koedam EL, Pijnenburg YA, Deeg DJ, Baak MM, van der Vlies AE, Scheltens P, et al. Early-onset dementia is associated with higher mortality. Dement Geriatr Cogn Disord. 2008; 26(2):147–152. PMID: 18679029.8. Schott JM, Ridha BH, Crutch SJ, Healy DG, Uphill JB, Warrington EK, et al. Apolipoprotein e genotype modifies the phenotype of Alzheimer disease. Arch Neurol. 2006; 63(1):155–156. PMID: 16401755.9. Mendez MF. Early-onset Alzheimer disease. Neurol Clin. 2017; 35(2):263–281. PMID: 28410659.10. Kay DW, Forster DP, Newens AJ. Long-term survival, place of death, and death certification in clinically diagnosed pre-senile dementia in northern England. Follow-up after 8-12 years. Br J Psychiatry. 2000; 177(2):156–162. PMID: 11026956.11. Samuel LJ, Szanton SL, Wolff JL, Ornstein KA, Parker LJ, Gitlin LN. Socioeconomic disparities in six-year incident dementia in a nationally representative cohort of U.S. older adults: an examination of financial resources. BMC Geriatr. 2020; 20(1):156. PMID: 32370792.12. Woods LM, Rachet B, Coleman MP. Origins of socio-economic inequalities in cancer survival: a review. Ann Oncol. 2006; 17(1):5–19. PMID: 16143594.13. Korhonen K, Einiö E, Leinonen T, Tarkiainen L, Martikainen P. Midlife socioeconomic position and old-age dementia mortality: a large prospective register-based study from Finland. BMJ Open. 2020; 10(1):e033234.14. van de Vorst IE, Koek HL, Stein CE, Bots ML, Vaartjes I. Socioeconomic disparities and mortality after a diagnosis of dementia: results from a nationwide registry linkage study. Am J Epidemiol. 2016; 184(3):219–226. PMID: 27380760.15. Chen R, Hu Z, Wei L, Wilson K. Socioeconomic status and survival among older adults with dementia and depression. Br J Psychiatry. 2014; 204(6):436–440. PMID: 24526747.16. Thomas BM, McGonigal G, McQuade CA, Starr JM, Whalley LJ. Survival in early onset dementia: effects of urbanization and socio-economic deprivation. Neuroepidemiology. 1997; 16(3):134–140. PMID: 9159768.17. Laver K, Dyer S, Whitehead C, Clemson L, Crotty M. Interventions to delay functional decline in people with dementia: a systematic review of systematic reviews. BMJ Open. 2016; 6(4):e010767.18. van Vliet D, de Vugt ME, Bakker C, Pijnenburg YA, Vernooij-Dassen MJ, Koopmans RT, et al. Time to diagnosis in young-onset dementia as compared with late-onset dementia. Psychol Med. 2013; 43(2):423–432. PMID: 22640548.19. van der Flier WM, Pijnenburg YA, Fox NC, Scheltens P. Early-onset versus late-onset Alzheimer’s disease: the case of the missing APOE \xc9\x9b allele. Lancet Neurol. 2011; 10(3):280–288. PMID: 21185234.20. Tellechea P, Pujol N, Esteve-Belloch P, Echeveste B, García-Eulate MR, Arbizu J, et al. Early- and late-onset Alzheimer disease: are they the same entity? Neurologia (Engl Ed). 2018; 33(4):244–253. PMID: 26546285.21. Ha R, Jung-Choi K. Area-based inequalities and distribution of healthcare resources for managing diabetes in South Korea: a cross-sectional multilevel analysis. BMJ Open. 2022; 12(2):e055360.22. Yoo KH, Shin DW, Cho MH, Kim SH, Bahk HJ, Kim SH, et al. Regional variations in frequency of glycosylated hemoglobin (HbA1c) monitoring in Korea: a multilevel analysis of nationwide data. Diabetes Res Clin Pract. 2017; 131:61–69. PMID: 28689084.23. Kyriopoulos II, Zavras D, Skroumpelos A, Mylona K, Athanasakis K, Kyriopoulos J. Barriers in access to healthcare services for chronic patients in times of austerity: an empirical approach in Greece. Int J Equity Health. 2014; 13(1):54. PMID: 25062725.24. Roh CG, Kim J. What are more efficient transportation services in a rural area? A case study in Yangsan city, South Korea. Int J Environ Res Public Health. 2022; 19(18):11263. PMID: 36141536.25. Jeon B, Choi SM, Kim CY. Socioeconomic equity in regional distribution of health care resources in Korea. Health Policy Manag. 2012; 22(1):85–108.26. Youn HM, Yun C, Kang SH, Kwon J, Lee HJ, Park EC, et al. A study on regional differences in healthcare in Korea: Using position value for relative comparison index. Health Policy Manag. 2021; 31(4):491–507.27. Chang KJ, Hong CH, Lee KS, Kang DR, Lee JD, Choi SH, et al. Mortality risk after diagnosis of early-onset Alzheimer’s disease versus late-onset Alzheimer’s disease: a propensity score matching analysis. J Alzheimers Dis. 2017; 56(4):1341–1348. PMID: 28157103.28. Lee DW. What is needed for the success of national responsibility for dementia. J Korean Med Assoc. 2017; 60(8):618.29. National Assembly Research Service. Problems of Korean Dementia Care Center’s general dementia screening project and its future policy tasks. Updated 2019. Accessed February 28, 2022. https://www.nars.go.kr/eng/report/view.do?cmsCode=CM0146&brdSeq=26574 .30. Ueki A, Shinjo H, Shimode H, Nakajima T, Morita Y. Factors associated with mortality in patients with early-onset Alzheimer’s disease: a five-year longitudinal study. Int J Geriatr Psychiatry. 2001; 16(8):810–815. PMID: 11536348.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Long-term Care of Dementia
- Health Status and Utilization of Long-term Care Facility in the Urban and Rural Aged
- Factors Related to Institutionalization in Elderly With Dementia: Analysis of Nationwide Population-Based Data
- Clinical Approaches to the Long-term Care Service focused on Dementia
- Analysis of the incidence of dementia in complete edentulous patients using the National Health Insurance Service-Elderly Cohort Database (NHIS-ECD)