Korean J Sports Med.
2022 Dec;40(4):259-262. 10.5763/kjsm.2022.40.4.259.
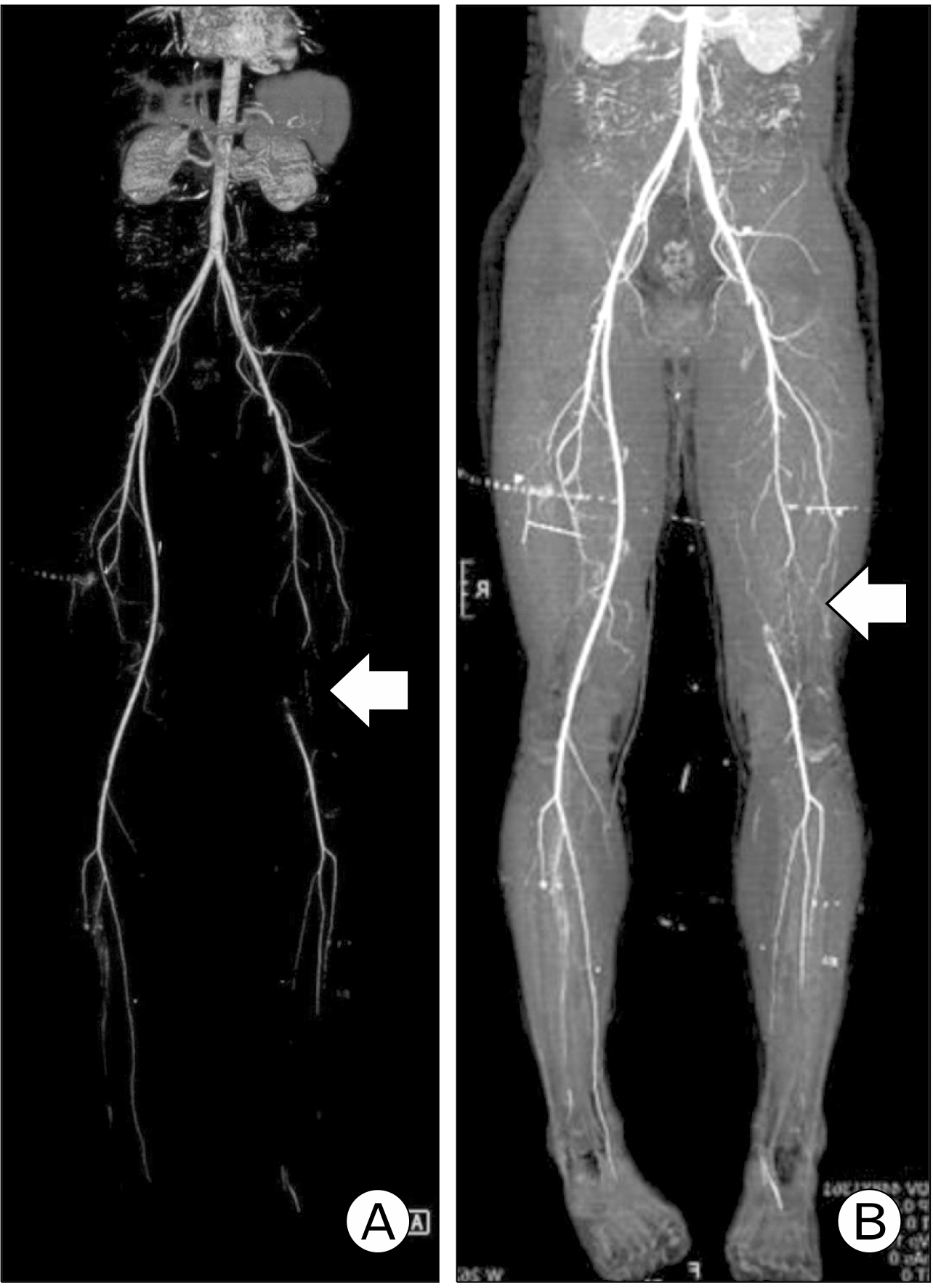
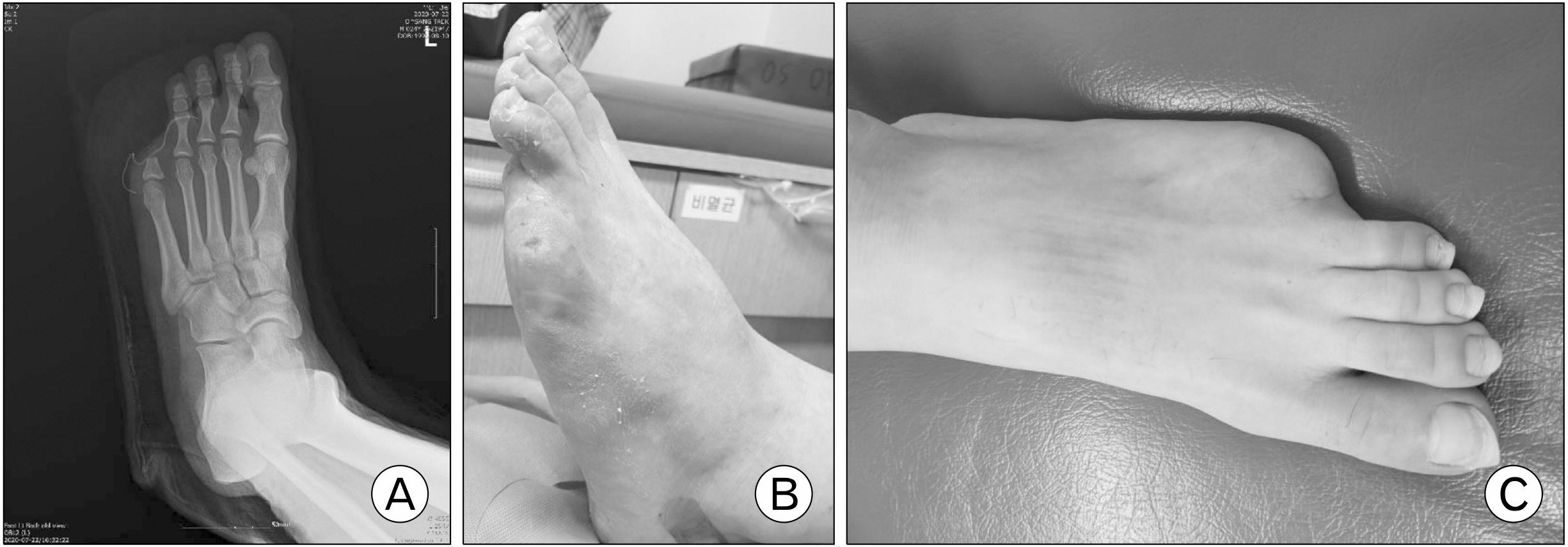
Premature Peripheral Arterial Disease with the 5th Toe Necrotizing Lesion after Workout: A Case Report
- Affiliations
-
- 1Busan Gunwoo Orthopedic Clinic, Busan, Korea
- 2Department of Orthopedic Surgery, Inje University Busan Paik Hospital, Busan, Korea
- KMID: 2536677
- DOI: http://doi.org/10.5763/kjsm.2022.40.4.259
Abstract
- Premature peripheral arterial disease is characterized by onset of peripheral arterial occlusion before age of 50 years. Its prevalence is rare. To the best of the authors’ knowledge, there is rare research of premature peripheral arterial disease in Korea. The authors encountered a case of necrotic toe caused by premature peripheral arterial disease after soccer workout. This paper reports this case with a review of the relevant literature.
Keyword
Figure
Reference
-
1. Hirsch AT, Haskal ZJ, Hertzer NR, et al. 2006; ACC/AHA 2005 Practice Guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease): endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; Trans-Atlantic Inter-Society Consensus; and Vascular Disease Foundation. Circulation. 113:e463–654. DOI: 10.1161/CIRCULATIONAHA.106.173994.2. Valentine RJ, Jackson MR, Modrall JG, McIntyre KE, Clagett GP. 1999; The progressive nature of peripheral arterial disease in young adults: a prospective analysis of white men referred to a vascular surgery service. J Vasc Surg. 30:436–44. DOI: 10.1016/S0741-5214(99)70070-4. PMID: 10477636.
Article3. Barretto S, Ballman KV, Rooke TW, Kullo IJ. 2003; Early-onset peripheral arterial occlusive disease: clinical features and determinants of disease severity and location. Vasc Med. 8:95–100. DOI: 10.1191/1358863x03vm475oa. PMID: 14518611.
Article4. Norgren L, Hiatt WR, Dormandy JA, et al. 2007; Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II). J Vasc Surg. 45 Suppl S:S5–67. DOI: 10.1016/j.jvs.2006.12.037. PMID: 17223489.
Article5. Mehta A, Dhindsa DS, Hooda A, et al. 2021; Premature atherosclerotic peripheral artery disease: an underrecognized and undertreated disorder with a rising global prevalence. Trends Cardiovasc Med. 31:351–8. DOI: 10.1016/j.tcm.2020.06.005. PMID: 32565142.
Article6. Ridker PM, Stampfer MJ, Rifai N. 2001; Novel risk factors for systemic atherosclerosis: a comparison of C-reactive protein, fibrinogen, homocysteine, lipoprotein(a), and standard cholesterol screening as predictors of peripheral arterial disease. JAMA. 285:2481–5. DOI: 10.1001/jama.285.19.2481. PMID: 11368701.7. Conte MS, Pomposelli FB, et al. Society for Vascular Surgery Lower Extremity Guidelines Writing Group. 2015; Society for Vascular Surgery practice guidelines for atherosclerotic occlusive disease of the lower extremities: management of asymptomatic disease and claudication. J Vasc Surg. 61(3 Suppl):2S–41S. DOI: 10.1016/j.jvs.2014.12.009. PMID: 25638515.
Article8. Gerhard-Herman MD, Gornik HL, Barrett C, et al. 2017; 2016 AHA/ACC Guideline on the management of patients with lower extremity peripheral artery disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 69:1465–508. DOI: 10.1016/j.jacc.2016.11.008. PMID: 27851991.9. Cho S, Lee SH, Joh JH. 2019; Risk factors for asymptomatic peripheral arterial disease in Korean population: lessons from a community-based screening. Ann Surg Treat Res. 97:210–6. DOI: 10.4174/astr.2019.97.4.210. PMID: 31620395. PMCID: PMC6779951.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Food Protein-induced Enterocolitis Mimic king Necrotizing Enterocolitis in a Premature Infant: Case Report
- Two-Phalanged Fifth Toe in Korean
- Two Cases of Necrotizing Enterocolitis Associated with Rotavirus Infection in Premature Infants
- Necrotizing Enterocolitis Associated with Norovirus Infection in a Preterm Infant
- Entero-colonic Fistula Secondary to Necrotizing Enterocolitis in Premature Infant: A Case Report