J Rhinol.
2022 Nov;29(3):167-171. 10.18787/jr.2022.00409.
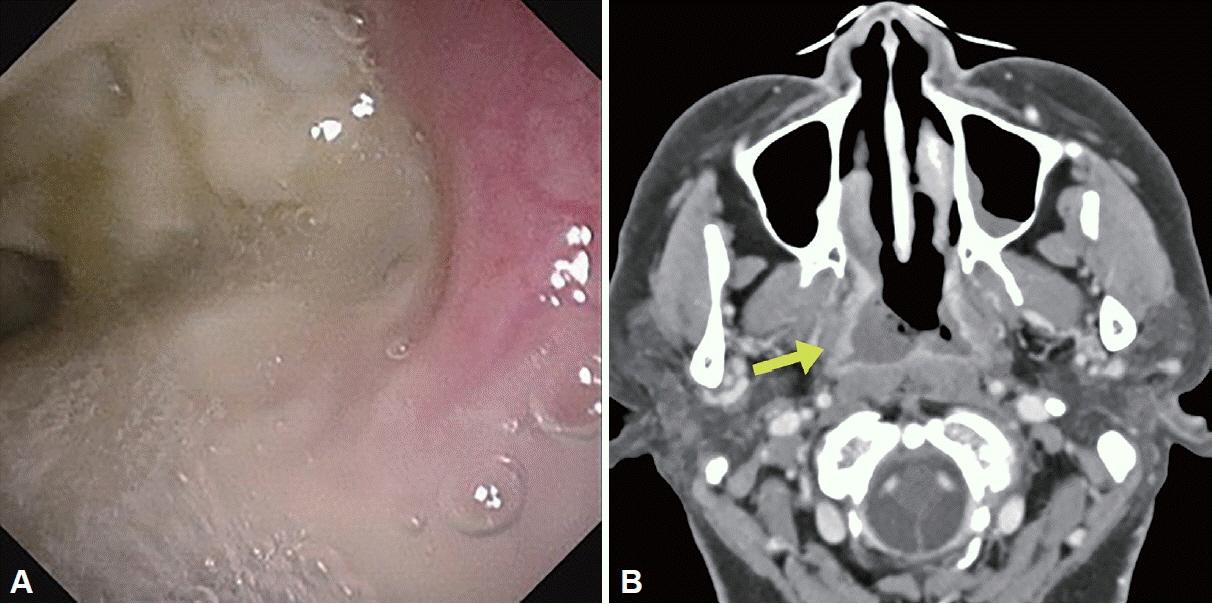
Two Cases of Primary Nasopharyngeal Tuberculosis
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, Hanyang University College of Medicine, Seoul, Republic of Korea
- KMID: 2536586
- DOI: http://doi.org/10.18787/jr.2022.00409
Abstract
- Nasopharyngeal tuberculosis can arise from both a primary infection and a secondary spread via the lymphatic or hematogenous system from a primary pulmonary lesion. Primary nasopharyngeal tuberculosis is rare and difficult to detect earlier because of the nonspecific presentations of the disease. As upper airway tuberculosis can be contagious, early initial diagnosis and suspicion of the physicians are needed in clinical practice. Recently, we successfully diagnosed and treated the disease by antitubercular medications of two cases of primary nasopharyngeal tuberculosis. Herein, we report our experience with a literature review.
Keyword
Figure
Reference
-
References
1. Kim HJ. Current status of tuberculosis in Korea. Korean J Med. 2012; 82(3):257–62.
Article2. Lee JK, Cho HP, Lee YM, Park JH. Four cases of primary nasopharyngeal tuberculosis presenting as extra pulmonary tuberculosis. J Clin Otolaryngol Head Neck Surg. 2013; 24(2):255–60.
Article3. Srirompotong S, Yimtae K, Jintakanon D. Nasopharyngeal tuberculosis: manifestations between 1991 and 2000. Otolaryngol Head Neck Surg. 2004; 131(5):762–4.
Article4. Cho YS, Choi N, Kim HY. A two cases of primary tuberculosis at the nasopharynx. J Rhinol. 2015; 22(2):123–7.
Article5. Park HS, Boo SH, Son JY. A case of primary nasopharyngeal tuberculosis. J Clin Otolaryngol Head Neck Surg. 2001; 12(1):118–21.
Article6. Jang DH, Kim HC, Hong YO, Kim JS. A case of nasopharyngeal tuberculosis which was difficult to differentiate from sarcoidosis. Korean J Otorhinolaryngol-Head Neck Surg. 2022; 65(4):231–6.
Article7. Kawamura I, Kudo T, Tsukahara M, Kurai H. Infection control for extrapulmonary tuberculosis at a tertiary care cancer center. Am J Infect Control. 2014; 42(10):1133–5.
Article8. Cai PQ, Li YZ, Zeng RF, Xu JH, Xie CM, Wu YP, et al. Nasopharyngeal tuberculosis: CT and MRI findings in thirty-six patients. Eur J Radiol. 2013; 82(9):e448–54.
Article9. Chan AB, Ma TK, Yu BK, King AD, Ho FN, Tse GM. Nasopharyngeal granulomatous inflammation and tuberculosis complicating undifferentiated carcinoma. Otolaryngol Head Neck Surg. 2004; 130(1):125–30.
Article10. Darouassi Y, Chihani M, Elktaibi A, Touati MM, Nadour K, Benjelloun A, et al. Association of laryngeal and nasopharyngeal tuberculosis: a case report. J Med Case Rep. 2015; 9:2.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Two Cases of Primary Tuberculosis at the Nasopharynx
- Primary Nasopharyngeal Tuberculosis without Cervical Lymphadenopathy: Report of a Case and Review of the Literature
- A case of primary nasopharyngeal tuberculosis with cervical lymphadenitis of immigrant woman from Vietnam
- A Case of Nasopharyngeal Tuberculosis Which Was Difficult to Differentiate From Sarcoidosis
- A Case of Incidentally Detected Nasopharyngeal Tuberculosis on F-18 FDG PET/CT