Ann Hepatobiliary Pancreat Surg.
2022 Nov;26(4):401-406. 10.14701/ahbps.22-031.
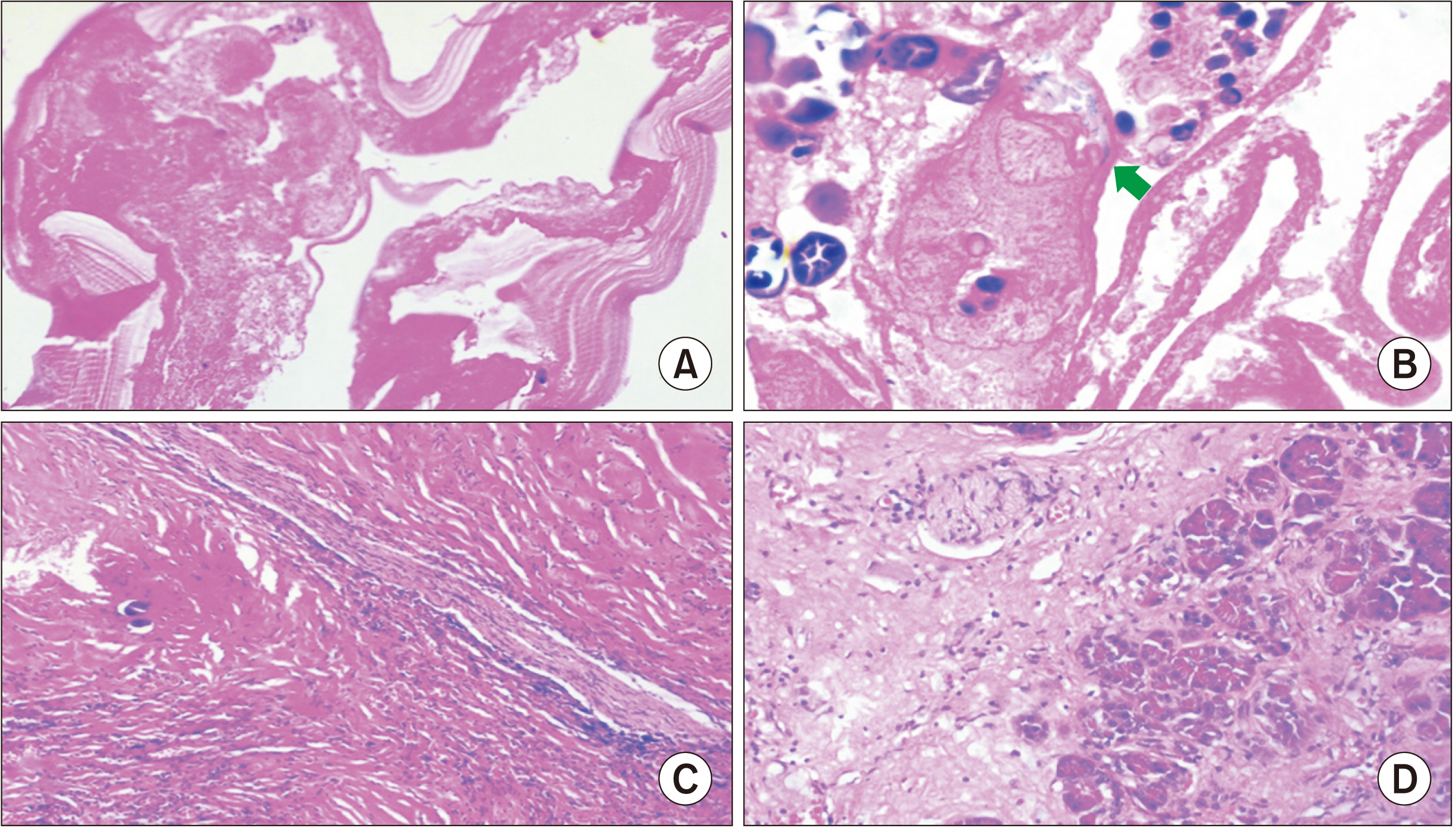
Isolated primary hydatid cyst of the pancreas: Management challenges of a cystic masquerade
- Affiliations
-
- 1Department of Surgical Gastroenterology, All India Institute of Medical Sciences (AIIMS), Bhopal, Madhya Pradesh, India
- 2Department of Radiodiagnosis, All India Institute of Medical Sciences (AIIMS), Bhopal, Madhya Pradesh, India
- 3Departments of Pathology and Laboratory Medicine, All India Institute of Medical Sciences (AIIMS), Bhopal, Madhya Pradesh, India
- KMID: 2536391
- DOI: http://doi.org/10.14701/ahbps.22-031
Abstract
- Abdominal hydatid cyst disease mostly involves the liver. Involvement of the pancreas as an isolated primary organ is rare accounting for < 2% of all systemic echinococcosis cases. It mostly involves the head of the pancreas. Symptoms depend on the location, size, and associated complications; therefore, it can have varied presentations including acute pancreatitis. On imaging, it can mimic other common pancreatic cystic lesions like pseudocyst or cystic neoplasm. Accurate preoperative diagnosis is usually difficult and requires a very high index of suspicion even in endemic areas. Herein, a case of primary isolated hydatid cyst of the pancreas that was initially diagnosed and managed as acute pancreatic pseudocyst is reported.
Figure
Reference
-
1. Akbulut S, Yavuz R, Sogutcu N, Kaya B, Hatipoglu S, Senol A, et al. 2014; Hydatid cyst of the pancreas: report of an undiagnosed case of pancreatic hydatid cyst and brief literature review. World J Gastrointest Surg. 6:190–200. DOI: 10.4240/wjgs.v6.i10.190. PMID: 25346801. PMCID: PMC4208043.2. Ahmed Z, Chhabra S, Massey A, Vij V, Yadav R, Bugalia R, et al. 2016; Primary hydatid cyst of pancreas: case report and review of literature. Int J Surg Case Rep. 27:74–77. DOI: 10.1016/j.ijscr.2016.07.054. PMID: 27552034. PMCID: PMC4995534.3. Wu Y, Gong J, Xiong W, Yu X, Lu X. 2021; Primary pancreatic hydatid cyst: a case report and literature review. BMC Gastroenterol. 21:164. DOI: 10.1186/s12876-021-01753-1. PMID: 33849455. PMCID: PMC8045313.4. Chinya A, Khanolkar A, Kumar J, Sinha SK. 2015; Isolated hydatid cyst of the pancreas masquerading as pancreatic pseudocyst. BMJ Case Rep. 2015:bcr2015211307. DOI: 10.1136/bcr-2015-211307. PMID: 26264949. PMCID: PMC4533679.5. Cankorkmaz L, Gümüş C, Celiksöz A, Köylüoğlu G. 2011; Primary hydatid disease of the pancreas mimicking pancreatic pseudo-cyst in a child: case report and review of the literature. Turkiye Parazitol Derg. 35:50–52. DOI: 10.5152/tpd.2011.13. PMID: 21618194.6. WHO Informal Working Group. 2003; International classification of ultrasound images in cystic echinococcosis for application in clinical and field epidemiological settings. Acta Trop. 85:253–261. DOI: 10.1016/S0001-706X(02)00223-1. PMID: 12606104.7. Stojkovic M, Rosenberger K, Kauczor HU, Junghanss T, Hosch W. 2012; Diagnosing and staging of cystic echinococcosis: how do CT and MRI perform in comparison to ultrasound? PLoS Negl Trop Dis. 6:e1880. DOI: 10.1371/journal.pntd.0001880. PMID: 23145199. PMCID: PMC3493391.8. Javed A, Agarwal G, Aravinda PS, Manipadam JM, Puri SK, Agarwal AK. 2020; Hydatid cyst of the pancreas: a diagnostic dilemma. Trop Gastroenterol. 41:73–81.9. Kısaoğlu A, Özoğul B, Atamanalp SS, Pirimoğlu B, Aydınlı B, Korkut E. 2015; Incidental isolated pancreatic hydatid cyst. Turkiye Parazitol Derg. 39:75–77. DOI: 10.5152/tpd.2015.3293. PMID: 25917590.10. Makni A, Jouini M, Kacem M, Safta ZB. 2012; Acute pancreatitis due to pancreatic hydatid cyst: a case report and review of the literature. World J Emerg Surg. 7:7. DOI: 10.1186/1749-7922-7-7. PMID: 22445170. PMCID: PMC3325852.11. Mandelia A, Wahal A, Solanki S, inivas M Sr, Bhatnagar V. 2012; Pancreatic hydatid cyst masquerading as a choledochal cyst. J Pediatr Surg. 47:e41–e44. DOI: 10.1016/j.jpedsurg.2012.07.054. PMID: 23164030.12. Ibis C, Albayrak D, Altan A. 2009; Primary hydatid disease of pancreas mimicking cystic neoplasm. South Med J. 102:529–530. DOI: 10.1097/SMJ.0b013e31819c3bef. PMID: 19373169.13. Dziri C, Dougaz W, Bouasker I. 2017; Surgery of the pancreatic cystic echinococcosis: systematic review. Transl Gastroenterol Hepatol. 2:105. DOI: 10.21037/tgh.2017.11.13. PMID: 29354762. PMCID: PMC5763016.14. Imam A, Khoury T, Weis D, Khalayleh H, Adeleh M, Khalaileh A. 2019; Laparoscopic cystectomy for pancreatic echinococcosis: a case report and literature review. Ann Hepatobiliary Pancreat Surg. 23:87–90. DOI: 10.14701/ahbps.2019.23.1.87. PMID: 30863816. PMCID: PMC6405372.15. Vasilescu A, Tarcoveanu E, Crumpei F, Blaj M, Bejan V, Bradea C. 2020; Laparoscopic approach of primary hydatid cyst of the pancreas - case report and literature review. Chirurgia (Bucur). 115:261–266. DOI: 10.21614/chirurgia.115.2.261. PMID: 32369731.16. Suryawanshi P, Khan AQ, Jatal S. 2011; Primary hydatid cyst of pancreas with acute pancreatitis. Int J Surg Case Rep. 2:122–124. DOI: 10.1016/j.ijscr.2011.02.011. PMID: 22096702. PMCID: PMC3199727.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- US and CT Findings of Splenic Hydatid Cyst: A Case Report
- Primary Giant Splenic and Hepatic Echinococcal Cysts Treated by Laparoscopy
- Laparoscopic management of giant hepatic hydatid cyst in a 12-year-old boy: a case report
- Overview of cystic lesion of the pancreas
- Pathologic Features of Pancreatic Cystic Neoplasms