Ann Hepatobiliary Pancreat Surg.
2022 Nov;26(4):318-324. 10.14701/ahbps.22-019.
Initial United Kingdom experience of endoscopic ultrasound-directed transgastric endoscopic retrograde cholangiopancreatography
- Affiliations
-
- 1Department of Gastroenterology, Calderdale and Huddersfield Foundation Trust, Huddersfield, United Kingdom
- 2Department of Gastroenterology, Leeds Teaching Hospitals NHS Trust, Leeds, United Kingdom
- 3Biomedical Communications, University of Toronto, Toronto, Ontario, Canada
- 4Department of Interventional Endoscopy, University Hospital Southampton NHS Foundation Trust, Southampton, United Kingdom
- KMID: 2536381
- DOI: http://doi.org/10.14701/ahbps.22-019
Abstract
- Backgrounds/Aims
Gallstone disease is a recognized complication of bariatric surgery. Subsequent management of choledocholithiasis may be challenging due to altered anatomy which may include Roux-en-Y gastric bypass (RYGB). We conducted a retrospective service evaluation study to assess the safety and efficacy of endoscopic ultrasound-directed transgastric endoscopic retrograde cholangiopancreatography (EDGE) in patients with RYGB anatomy.
Methods
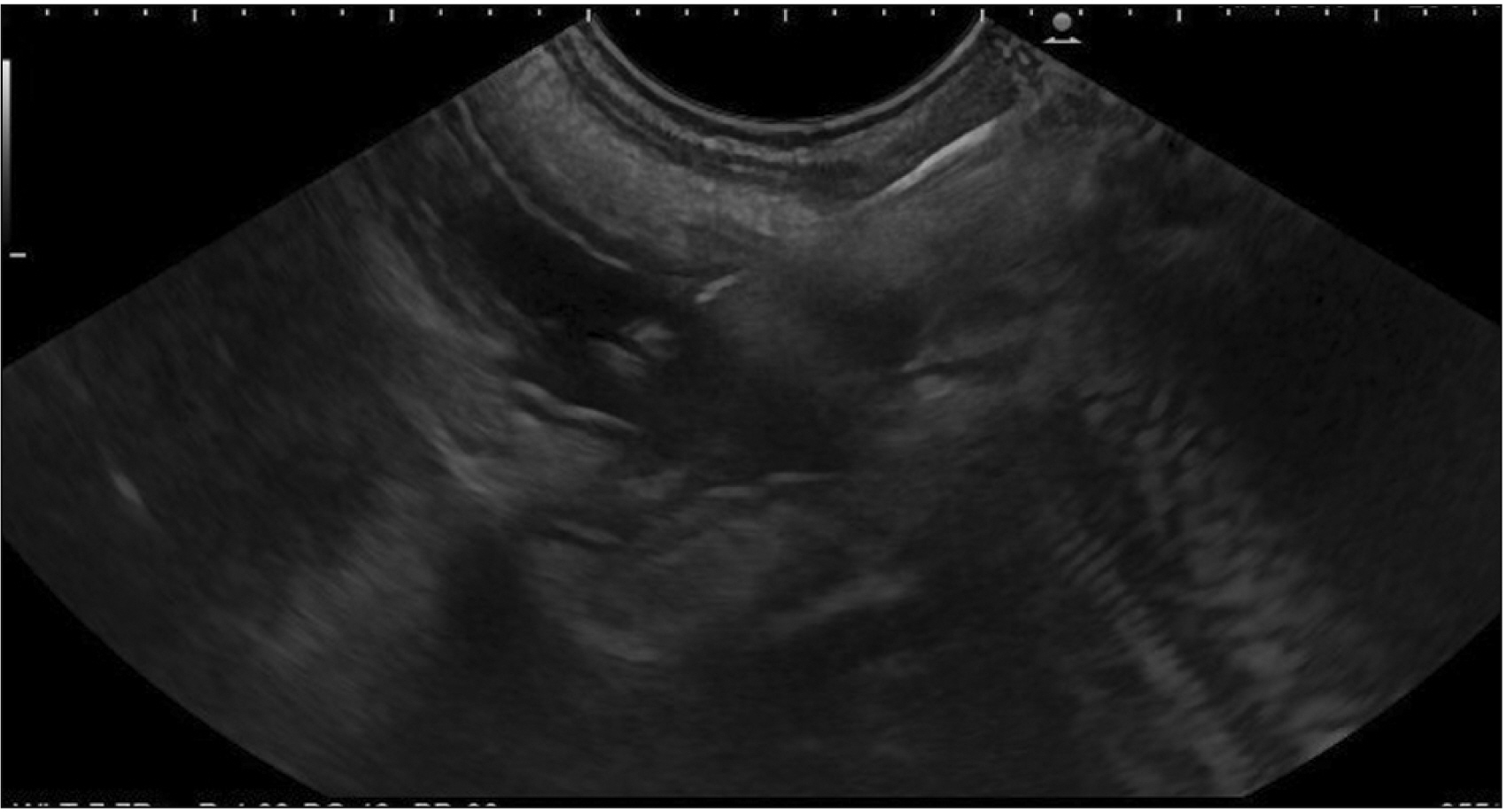
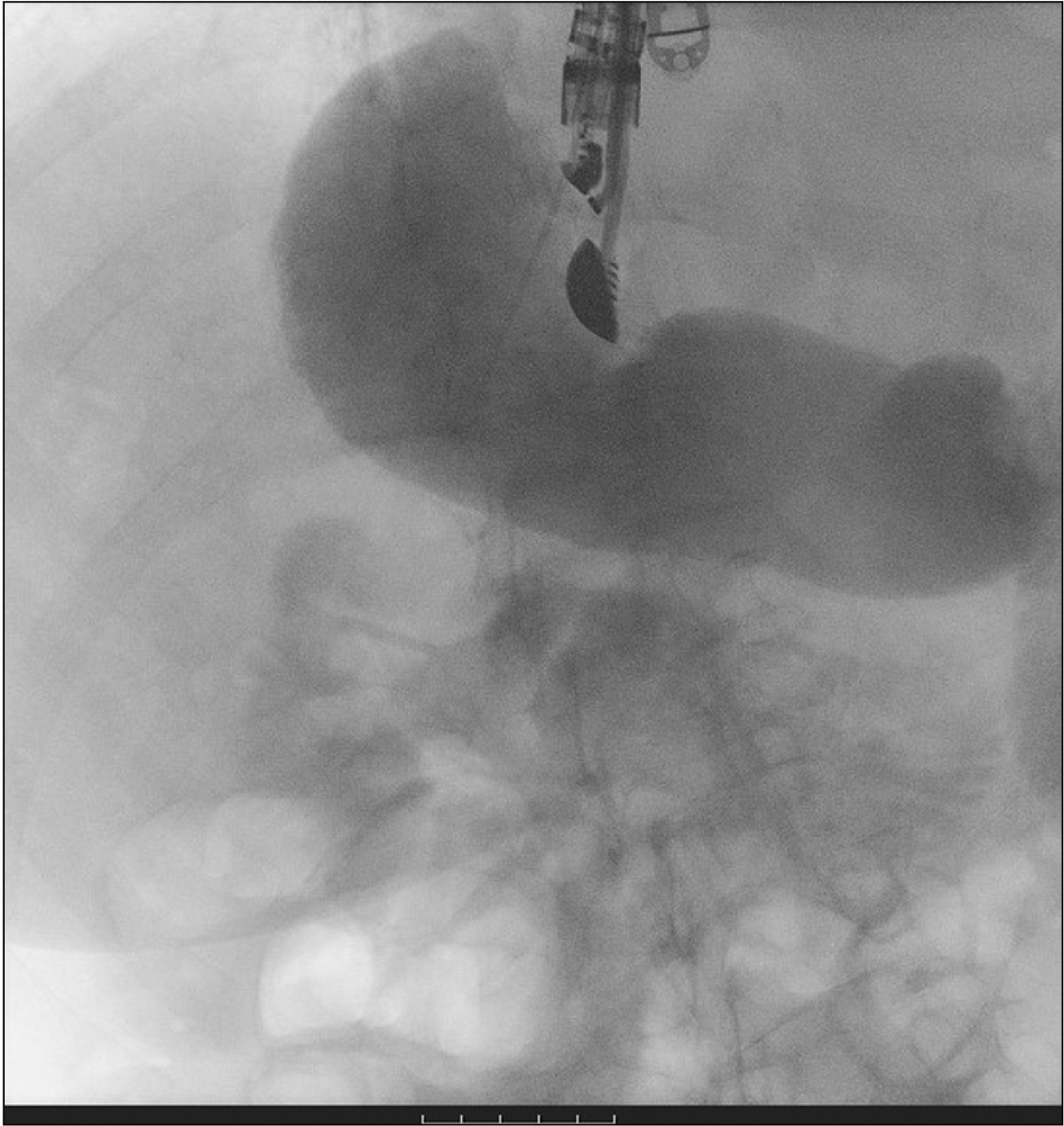
All the patients who underwent EDGE for endoscopic retrograde cholangiopancreatography after RYGB at two tertiary care centers in the United Kingdom between January 2020 and October 2021 were included in the study. Clinical and demographic details were recorded for all patients. The primary outcome measures were technical and clinical success. Adverse events were recorded. Hot Axios lumen apposing metal stents measuring 20 mm in diameter and 10 mm in length were used in all the patients for creation of a gastro-gastric or gastro-jejunal fistula.
Results
A total of 14 patients underwent EDGE during the study period. The majority of the patients were female (85.7%) and the mean age of patients was 65.8 ± 9.8 years. Technical success was achieved in all but one patient at the first attempt (92.8%) and clinical success was achieved in 100% of the patients. Complications arose in 3 patients with 1 patient experiencing persistent fistula and weight gain.
Conclusions
In patients with RYGB anatomy, EDGE facilitated biliary access has a high rate of clinical success with an acceptable safety profile. Adverse events are uncommon and can be managed endoscopically.
Keyword
Figure
Reference
-
1. NHS Digital. Statistics on obesity, physical activity and diet: England, 2020. Leeds: NHS Digital;2020.2. Chang SH, Stoll CR, Song J, Varela JE, Eagon CJ, Colditz GA. 2014; The effectiveness and risks of bariatric surgery: an updated systematic review and meta-analysis, 2003-2012. JAMA Surg. 149:275–287. DOI: 10.1001/jamasurg.2013.3654. PMID: 24352617. PMCID: PMC3962512.3. Shenoy SS, Gilliam A, Mehanna A, Kanakala V, Bussa G, Gill T, et al. 2020; Laparoscopic sleeve gastrectomy versus laparoscopic Roux-en-Y gastric bypass in elderly bariatric patients: safety and efficacy-a systematic review and meta-analysis. Obes Surg. 30:4467–4473. DOI: 10.1007/s11695-020-04819-3. PMID: 32594469.4. Stender S, Nordestgaard BG, Tybjaerg-Hansen A. 2013; Elevated body mass index as a causal risk factor for symptomatic gallstone disease: a Mendelian randomization study. Hepatology. 58:2133–2141. DOI: 10.1002/hep.26563. PMID: 23775818.5. Shiffman ML, Sugerman HJ, Kellum JM, Brewer WH, Moore EW. 1991; Gallstone formation after rapid weight loss: a prospective study in patients undergoing gastric bypass surgery for treatment of morbid obesity. Am J Gastroenterol. 86:1000–1005.6. Li VK, Pulido N, Fajnwaks P, Szomstein S, Rosenthal R, Martinez-Duartez P. 2009; Predictors of gallstone formation after bariatric surgery: a multivariate analysis of risk factors comparing gastric bypass, gastric banding, and sleeve gastrectomy. Surg Endosc. 23:1640–1644. Erratum in: Surg Endosc 2009;23:1645. DOI: 10.1007/s00464-008-0204-6. PMID: 19057954.7. Ayoub F, Brar TS, Banerjee D, Abbas AM, Wang Y, Yang D, et al. 2020; Laparoscopy-assisted versus enteroscopy-assisted endoscopic retrograde cholangiopancreatography (ERCP) in Roux-en-Y gastric bypass: a meta-analysis. Endosc Int Open. 8:E423–E436. DOI: 10.1055/a-1070-9132. PMID: 32118116. PMCID: PMC7035133.8. Fuente I, Beskow A, Wright F, Uad P, de Santibañes M, Palavecino M, et al. 2021; Laparoscopic transcystic common bile duct exploration as treatment for choledocholithiasis after Roux-en-Y gastric bypass. Surg Endosc. 35:6913–6920. DOI: 10.1007/s00464-020-08201-3. PMID: 33398581.9. Kedia P, Tarnasky PR, Nieto J, Steele SL, Siddiqui A, Xu MM, et al. 2019; EUS-directed transgastric ERCP (EDGE) versus laparoscopy-assisted ERCP (LA-ERCP) for Roux-en-Y gastric bypass (RYGB) anatomy: a multicenter early comparative experience of clinical outcomes. J Clin Gastroenterol. 53:304–308. DOI: 10.1097/MCG.0000000000001037. PMID: 29668560.10. Skinner M, Popa D, Neumann H, Wilcox CM, Mönkemüller K. 2014; ERCP with the overtube-assisted enteroscopy technique: a systematic review. Endoscopy. 46:560–572. DOI: 10.1055/s-0034-1365698. PMID: 24839188.11. Schreiner MA, Chang L, Gluck M, Irani S, Gan SI, Brandabur JJ, et al. 2012; Laparoscopy-assisted versus balloon enteroscopy-assisted ERCP in bariatric post-Roux-en-Y gastric bypass patients. Gastrointest Endosc. 75:748–756. DOI: 10.1016/j.gie.2011.11.019. PMID: 22301340.12. Banerjee N, Parepally M, Byrne TK, Pullatt RC, Coté GA, Elmunzer BJ. 2017; Systematic review of transgastric ERCP in Roux-en-Y gastric bypass patients. Surg Obes Relat Dis. 13:1236–1242. DOI: 10.1016/j.soard.2017.02.005. PMID: 28336200.13. Abbas AM, Strong AT, Diehl DL, Brauer BC, Lee IH, Burbridge R, et al. 2018; Multicenter evaluation of the clinical utility of laparoscopy-assisted ERCP in patients with Roux-en-Y gastric bypass. Gastrointest Endosc. 87:1031–1039. DOI: 10.1016/j.gie.2017.10.044. PMID: 29129525.14. Grimes KL, Maciel VH, Mata W, Arevalo G, Singh K, Arregui ME. 2015; Complications of laparoscopic transgastric ERCP in patients with Roux-en-Y gastric bypass. Surg Endosc. 29:1753–1759. DOI: 10.1007/s00464-014-3901-3. PMID: 25318366.15. May D, Vogels E, Parker D, Petrick A, Diehl D, Gabrielsen J. 2019; Overall outcomes of laparoscopic-assisted ERCP after Roux-en-Y gastric bypass and sphincter of Oddi dysfunction subgroup analysis. Endosc Int Open. 7:E1276–E1280. DOI: 10.1055/a-0832-1898. PMID: 31579709. PMCID: PMC6773570.16. Yang D, Draganov PV. 2019; ERCP in patients with Roux-en-Y gastric bypass: one size does not fit all. Gastrointest Endosc. 89:646. DOI: 10.1016/j.gie.2018.09.014. PMID: 30784505.17. James HJ, James TW, Wheeler SB, Spencer JC, Baron TH. 2019; Cost-effectiveness of endoscopic ultrasound-directed transgastric ERCP compared with device-assisted and laparoscopic-assisted ERCP in patients with Roux-en-Y anatomy. Endoscopy. 51:1051–1058. DOI: 10.1055/a-0938-3918. PMID: 31242509.18. Dhindsa BS, Dhaliwal A, Mohan BP, Mashiana HS, Girotra M, Singh S, et al. 2020; EDGE in Roux-en-Y gastric bypass: how does it compare to laparoscopy-assisted and balloon enteroscopy ERCP: a systematic review and meta-analysis. Endosc Int Open. 8:E163–E171. DOI: 10.1055/a-1067-4411. PMID: 32010749. PMCID: PMC6976316.19. Tucker O, Soriano I, Szomstein S, Rosenthal R. 2008; Management of choledocholithiasis after laparoscopic Roux-en-Y gastric bypass. Surg Obes Relat Dis. 4:674–678. DOI: 10.1016/j.soard.2008.01.014. PMID: 18539541.20. Barclay RL, Jain A, Ferland ASB, Chen YI, Donnellan F. 2022; Living on the EDGE: Canadian experience with EUS-directed transgastric ERCP (EDGE) in patients with roux-en-Y gastric bypass anatomy. J Can Assoc Gastroenterol. 5:116–120. DOI: 10.1093/jcag/gwab035. PMID: 35669842. PMCID: PMC9157288.21. Runge TM, Chiang AL, Kowalski TE, James TW, Baron TH, Nieto J, et al. 2021; Endoscopic ultrasound-directed transgastric ERCP (EDGE): a retrospective multicenter study. Endoscopy. 53:611–618. DOI: 10.1055/a-1254-3942. PMID: 32882722.22. Tyberg A, Kedia P, Tawadros A, Tarnasky PR, Gaidhane M, Nieto J, et al. 2020; EUS-directed transgastric endoscopic retrograde cholangiopancreatography (EDGE): the first learning curve. J Clin Gastroenterol. 54:569–572. DOI: 10.1097/MCG.0000000000001326. PMID: 32149820.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic ultrasound-directed transgastric endoscopic retrograde cholangiopancreatography for patients with Roux-en-Y gastric bypass anatomy: technical overview
- Commentary on “Endoscopic Ultrasound (EUS)-Directed Transgastric Endoscopic Retrograde Cholangiopancreatography or EUSâ€
- Endoscopic Ultrasound (EUS)-Directed Transgastric Endoscopic Retrograde Cholangiopancreatography or EUS: Mid-Term Analysis of an Emerging Procedure
- Training in Endoscopy: Endoscopic Retrograde Cholangiopancreatography
- Successful endoscopic closure of an esophageal leak after endoscopic ultrasound-guided hepaticoesophagostomy by using n-butyl-2 cyanoacrylate