Arch Hand Microsurg.
2022 Dec;27(4):320-328. 10.12790/ahm.22.0021.
Microsurgical reconstruction for traumatic hand defects in pediatric patients
- Affiliations
-
- 1Department of Plastic and Reconstructive Surgery, Gwangmyeong Sungae General Hospital, Gwangmyeong, Korea
- KMID: 2536220
- DOI: http://doi.org/10.12790/ahm.22.0021
Abstract
- Purpose
Microsurgery in pediatric patients remains challenging because of technical difficulties in small-vessel anastomosis and flap dissection. Few reports have focused exclusively on the microsurgical reconstruction of traumatic hand defects in children. Herein, we share our experience of posttraumatic hand reconstruction with free tissue transfer in pediatric patients and compare the treatment outcomes with adults.
Methods
A single-institution retrospective review of trauma-induced microsurgical hand reconstruction cases was performed. Pediatric patients below 17 years old and adults who underwent microsurgical reconstruction of traumatic hand defects between 2011 and 2021 were included. Patient demographics, flap type, use of vein grafts, operative time, flap survival, and postoperative complications were documented. A subgroup analysis of patients younger than 8 years was also performed. Data of pediatric patients were statistically compared with those of adults who underwent free flap surgery using nearly identical surgical procedures by four senior surgeons at our medical center.
Results
Forty-one flaps in 39 pediatric patients and 184 flaps in 184 adult patients were analyzed. Fasciocutaneous flaps were predominantly used in both groups. In pediatric patients, all flaps survived, while 170 adults (92.4%) survived. No statistically significant between-group differences in treatment outcomes were found. However, pediatric patients (22.0%) had significantly fewer secondary operations than adults (67.4%, p<0.001).
Conclusion
Microsurgical reconstruction for trauma-induced hand defects in pediatric patients has a high success rate and low complication rate, just as with adults. Pediatric patients may be more resistant to partial necrotic flap changes, thereby requiring fewer secondary operations than adults.
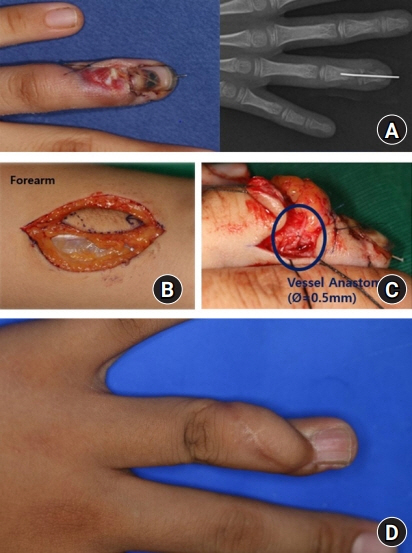
Figure
Reference
-
References
1. Momeni A, Lanni M, Levin LS, Kovach SJ. Microsurgical reconstruction of traumatic lower extremity defects in the pediatric population. Plast Reconstr Surg. 2017; 139:998–1004.
Article2. Gupta A, Lakhiani C, Lim BH, et al. Free tissue transfer to the traumatized upper extremity: risk factors for postoperative complications in 282 cases. J Plast Reconstr Aesthet Surg. 2015; 68:1184–90.
Article3. Aboelatta YA, Aly HM. Free tissue transfer and replantation in pediatric patients: technical feasibility and outcome in a series of 28 patients. J Hand Microsurg. 2013; 5:74–80.
Article4. Devaraj VS, Kay SP, Batchelor AG, Yates A. Microvascular surgery in children. Br J Plast Surg. 1991; 44:276–80.
Article5. Duteille F, Lim A, Dautel G. Free flap coverage of upper and lower limb tissue defects in children: a series of 22 patients. Ann Plast Surg. 2003; 50:344–9.
Article6. El-Gammal TA, El-Sayed A, Kotb MM, et al. Dorsal foot resurfacing using free anterolateral thigh (ALT) flap in children. Microsurgery. 2013; 33:259–64.
Article7. Mast BA, Newton ED. Aggressive use of free flaps in children for burn scar contractures and other soft-tissue deficits. Ann Plast Surg. 1996; 36:569–75.
Article8. Arslan H, Çinar C, Bingöl UA, Yücel OA. Subacute and delayed period microsurgical management of traumatic extremity injuries in pediatric population. Microsurgery. 2012; 32:527–32.
Article9. Shapiro J, Akbarnia BA, Hanel DP. Free tissue transfer in children. J Pediatr Orthop. 1989; 9:590–5.
Article10. Konttila E, Koljonen V, Kauhanen S, Kallio P, Tukiainen E. Microvascular reconstruction in children-a report of 46 cases. J Trauma. 2010; 68:548–52.
Article11. Chen C, Wang ZT, Hao LW, Liu LF. Microsurgical tissue transfer in complex upper extremity trauma. Clin Plast Surg. 2020; 47:521–34.
Article12. Arnez ZM, Hanel DP. Free tissue transfer for reconstruction of traumatic limb injuries in children. Microsurgery. 1991; 12:207–15.
Article13. van Bekkum S, de Jong T, Zuidam M, Mureau MA. Long-term quality of life after free flap upper extremity reconstruction for traumatic injuries. J Reconstr Microsurg. 2020; 36:213–22.
Article14. Upton J, Guo L. Pediatric free tissue transfer: a 29-year experience with 433 transfers. Plast Reconstr Surg. 2008; 121:1725–37.
Article15. Wei FC, el-Gammal TA, Chen HC, Chuang DC, Chiang YC, Chen SH. Toe-to-hand transfer for traumatic digital amputations in children and adolescents. Plast Reconstr Surg. 1997; 100:605–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Microsurgical Reconstruction of the Thumb
- Microsurgical Reconstruction in Pediatric Patients
- Reconstruction of a Mangled Hand with a Thoracodorsal Artery Perforator Free Flap: A Report of Two Cases
- Reconstruction of Traumatic Orbital Defects Using Porous Polyethylene Sheet
- Microsurgical Distal Thumb Reconstruction Using a Mini Wrap-around Free Flap