J Korean Med Sci.
2022 Nov;37(46):e326. 10.3346/jkms.2022.37.e326.
Long COVID-19 and Health-Related Quality of Life of Mild Cases in Korea: 3-Months Follow-up of a Single Community Treatment Center
- Affiliations
-
- 1Department of Family Medicine, Seoul National University Hospital, Seoul, Korea
- 2Department of Clinical Sciences, Seoul National University College of Medicine, Seoul, Korea
- 3Department of Family Medicine, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
- 4Institute on Aging, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2536133
- DOI: http://doi.org/10.3346/jkms.2022.37.e326
Abstract
- Background
Severe acute respiratory syndrome coronavirus 2 (coronavirus disease 2019 [COVID-19]) survivors mount as the pandemic continues. To date, studies on persistent symptoms and their effects on health-related quality of life (HRQoL) in mild COVID-19 cases have been limited.
Methods
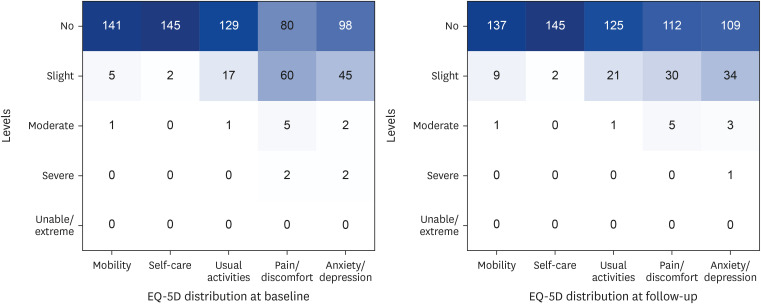
A prospective online survey was conducted in COVID-19 patients who were admitted to Seongnam Community Treatment Center, an isolation center in South Korea, from November 23rd 2021 to January 2nd 2022. Patients above the age of 19 with no or mild symptoms were included in the study. Total of 147 patients returned to the follow-up survey 3 months after discharge. Baseline demographics, clinical characteristics, symptoms, and EuroQol-5 dimensions-5 levels (EQ-5D-5L) measures were investigated.
Results
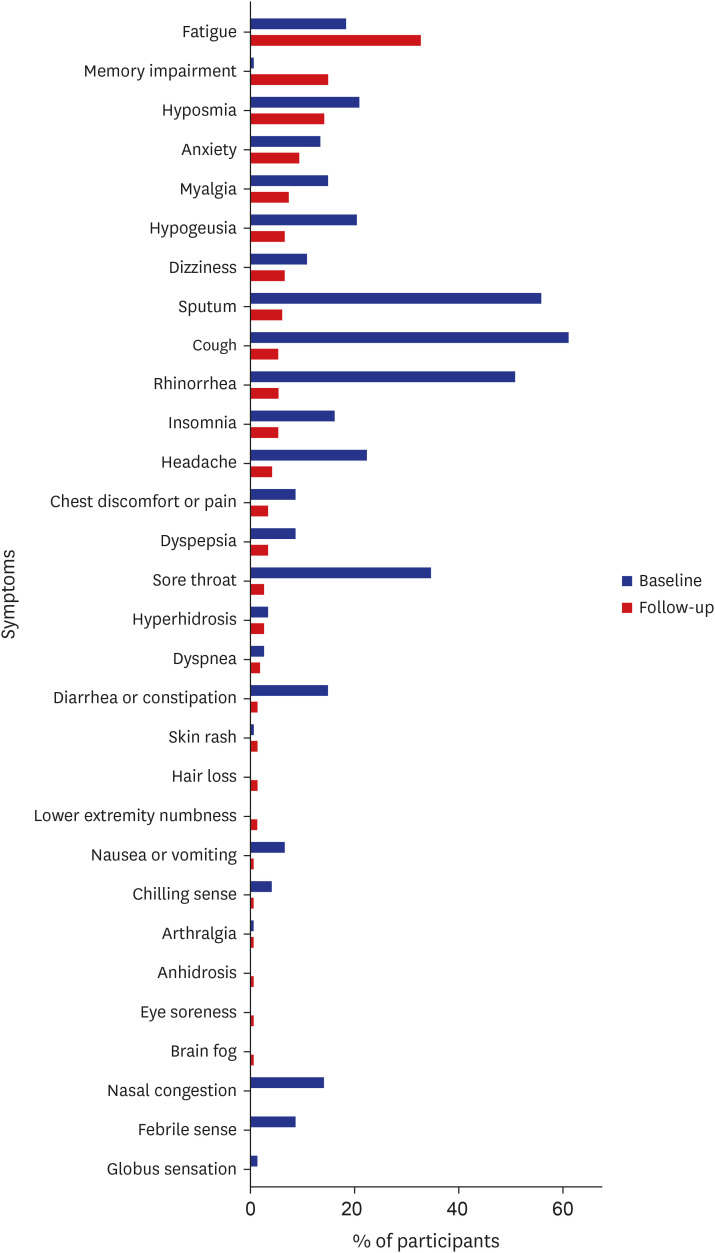
The median (interquartile range [IQR]) interval period between the initial and follow-up survey was 96.0 (93.0–98.0) days. The median (IQR) age of participants was 51.0 (43.0–61.0). During isolation, 131 (89.1%) patients manifested symptoms. On follow-up, 82 (55.8%) participants remained symptomatic. Common symptoms were constitutional (fatigue, myalgia), neurological (memory impairment, hyposmia, hypogeusia, dizziness), and neuropsychiatric (anxiety) symptoms. Participants with remaining neuropsychiatric symptoms reported the lowest EQ-5D-5L index values. Factors associated with persistent symptoms and diminished HRQoL were identified as female sex, metabolic disease, and anxiety during acute COVID-19 phase.
Conclusions
Cardiopulmonary symptoms improved over time but constitutional, neurological, neuropsychiatric symptoms remained. Patients with neuropsychiatric symptoms (anxiety and insomnia) reported the worst HRQoL. Female sex, metabolic disease, and anxiety during the acute COVID-19 phase were associated with long COVID. Observations of long-term symptoms of COVID-19 with decline in HRQoL and integrated research in COVID-19 survivors are warranted.
Keyword
Figure
Reference
-
1. Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020; 20(5):533–534. PMID: 32087114.2. Our World in Data. Daily new confirmed COVID-19 deaths per million people. Updated 2022. Accessed May 5, 2022. https://ourworldindata.org/explorers/coronavirus-data-explorer .3. Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020; 323(11):1061–1069. PMID: 32031570.4. Kim MK, Lee B, Choi YY, Um J, Lee KS, Sung HK, et al. Clinical characteristics of 40 patients infected with the SARS-CoV-2 omicron variant in Korea. J Korean Med Sci. 2022; 37(3):e31. PMID: 35040299.5. Mehandru S, Merad M. Pathological sequelae of long-haul COVID. Nat Immunol. 2022; 23(2):194–202. PMID: 35105985.6. Al-Aly Z, Xie Y, Bowe B. High-dimensional characterization of post-acute sequelae of COVID-19. Nature. 2021; 594(7862):259–264. PMID: 33887749.7. Salamanna F, Veronesi F, Martini L, Landini MP, Fini M. Post-COVID-19 syndrome: the persistent symptoms at the post-viral stage of the disease. A systematic review of the current data. Front Med (Lausanne). 2021; 8:653516. PMID: 34017846.8. Blomberg B, Mohn KG, Brokstad KA, Zhou F, Linchausen DW, Hansen BA, et al. Long COVID in a prospective cohort of home-isolated patients. Nat Med. 2021; 27(9):1607–1613. PMID: 34163090.9. Johns Hopkins Coronavirus Resource Center. COVID-19 dashboard. Updated 2022. Accessed May 2, 2022. https://coronavirus.jhu.edu/map.html .10. Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res. 2011; 20(10):1727–1736. PMID: 21479777.11. Finch AP, Brazier JE, Mukuria C. What is the evidence for the performance of generic preference-based measures? A systematic overview of reviews. Eur J Health Econ. 2018; 19(4):557–570. PMID: 28560520.12. Kim SH, Ahn J, Ock M, Shin S, Park J, Luo N, et al. The EQ-5D-5L valuation study in Korea. Qual Life Res. 2016; 25(7):1845–1852. PMID: 26961008.13. Ding H, Yin S, Cheng Y, Cai Y, Huang W, Deng W. Neurologic manifestations of nonhospitalized patients with COVID-19 in Wuhan, China. MedComm (2020). 2020; 1(2):253–256. PMID: 34172986.14. Cénat JM, Blais-Rochette C, Kokou-Kpolou CK, Noorishad PG, Mukunzi JN, McIntee SE, et al. Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder, and psychological distress among populations affected by the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatry Res. 2021; 295:113599. PMID: 33285346.15. Song E, Kweon Y, Hwang Y, An M. Health-related quality of life and its related factors among cancer survivors and general adults: focusing on lifestyle behaviors and mental health. Korean J Adult Nurs. 2020; 32(4):385–398.16. Sudre CH, Murray B, Varsavsky T, Graham MS, Penfold RS, Bowyer RC, et al. Attributes and predictors of long COVID. Nat Med. 2021; 27(4):626–631. PMID: 33692530.17. Tenforde MW, Self WH, Adams K, Gaglani M, Ginde AA, McNeal T, et al. Association between mRNA vaccination and COVID-19 hospitalization and disease severity. JAMA. 2021; 326(20):2043–2054. PMID: 34734975.18. Self WH, Tenforde MW, Rhoads JP, Gaglani M, Ginde AA, Douin DJ, et al. Comparative effectiveness of Moderna, Pfizer-BioNTech, and Janssen (Johnson & Johnson) vaccines in preventing COVID-19 hospitalizations among adults without immunocompromising conditions - United States, March-August 2021. MMWR Morb Mortal Wkly Rep. 2021; 70(38):1337–1343. PMID: 34555004.19. Baker HA, Safavynia SA, Evered LA. The ‘third wave’: impending cognitive and functional decline in COVID-19 survivors. Br J Anaesth. 2021; 126(1):44–47. PMID: 33187638.20. Ahmad I, Rathore FA. Neurological manifestations and complications of COVID-19: a literature review. J Clin Neurosci. 2020; 77:8–12. PMID: 32409215.21. Rybak LP. Metabolic disorders of the vestibular system. Otolaryngol Head Neck Surg. 1995; 112(1):128–132. PMID: 7816447.22. Singh P, Jain A, Kaur G. Impact of hypoglycemia and diabetes on CNS: correlation of mitochondrial oxidative stress with DNA damage. Mol Cell Biochem. 2004; 260(1-2):153–159. PMID: 15228097.23. Mauro C, De Rosa V, Marelli-Berg F, Solito E. Metabolic syndrome and the immunological affair with the blood-brain barrier. Front Immunol. 2015; 5:677. PMID: 25601869.24. Singh MV, Chapleau MW, Harwani SC, Abboud FM. The immune system and hypertension. Immunol Res. 2014; 59(1-3):243–253. PMID: 24847766.25. Gerges Harb J, Noureldine HA, Chedid G, Eldine MN, Abdallah DA, Chedid NF, et al. SARS, MERS and COVID-19: clinical manifestations and organ-system complications: a mini review. Pathog Dis. 2020; 78(4):ftaa033. PMID: 32633327.26. Kim HC, Yoo SY, Lee BH, Lee SH, Shin HS. Psychiatric findings in suspected and confirmed Middle East respiratory syndrome patients quarantined in hospital: a retrospective chart analysis. Psychiatry Investig. 2018; 15(4):355–360.27. Lam MH, Wing YK, Yu MW, Leung CM, Ma RC, Kong AP, et al. Mental morbidities and chronic fatigue in severe acute respiratory syndrome survivors: long-term follow-up. Arch Intern Med. 2009; 169(22):2142–2147. PMID: 20008700.28. Ahmed H, Patel K, Greenwood DC, Halpin S, Lewthwaite P, Salawu A, et al. Long-term clinical outcomes in survivors of severe acute respiratory syndrome and Middle East respiratory syndrome coronavirus outbreaks after hospitalisation or ICU admission: a systematic review and meta-analysis. J Rehabil Med. 2020; 52(5):jrm00063. PMID: 32449782.29. Helms J, Kremer S, Merdji H, Clere-Jehl R, Schenck M, Kummerlen C, et al. Neurologic features in severe SARS-CoV-2 infection. N Engl J Med. 2020; 382(23):2268–2270. PMID: 32294339.30. World Health Organization. Middle East Respiratory Syndrome. Geneva, Switzerland: World Health Organization;2022.31. World Health Organization. Summary of probable SARS cases with onset of illness from 1 November 2002 to 31 July 2003. Updated 2015. Accessed April 29, 2022. https://www.who.int/publications/m/item/summary-of-probable-sars-cases-with-onset-of-illness-from-1-november-2002-to-31-july-2003 .32. Garrigues E, Janvier P, Kherabi Y, Le Bot A, Hamon A, Gouze H, et al. Post-discharge persistent symptoms and health-related quality of life after hospitalization for COVID-19. J Infect. 2020; 81(6):e4–e6. PMID: 32853602.33. Arab-Zozani M, Hashemi F, Safari H, Yousefi M, Ameri H. Health-related quality of life and its associated factors in COVID-19 patients. Osong Public Health Res Perspect. 2020; 11(5):296–302. PMID: 33117634.34. Moreno-Pérez O, Merino E, Leon-Ramirez JM, Andres M, Ramos JM, Arenas-Jiménez J, et al. Post-acute COVID-19 syndrome. Incidence and risk factors: a Mediterranean cohort study. J Infect. 2021; 82(3):378–383. PMID: 33450302.35. Carfì A, Bernabei R, Landi F. Gemelli Against COVID-19 Post-Acute Care Study Group. Persistent symptoms in patients after acute COVID-19. JAMA. 2020; 324(6):603–605. PMID: 32644129.36. Jacobson KB, Rao M, Bonilla H, Subramanian A, Hack I, Madrigal M, et al. Patients with uncomplicated coronavirus disease 2019 (COVID-19) have long-term persistent symptoms and functional impairment similar to patients with severe COVID-19: a cautionary tale during a global pandemic. Clin Infect Dis. 2021; 73(3):e826–e829. PMID: 33624010.37. Méndez R, Balanzá-Martínez V, Luperdi SC, Estrada I, Latorre A, González-Jiménez P, et al. Short-term neuropsychiatric outcomes and quality of life in COVID-19 survivors. J Intern Med. 2021; 290(3):621–631. PMID: 33533521.38. Fernández-de-Las-Peñas C, Palacios-Ceña D, Gómez-Mayordomo V, Florencio LL, Cuadrado ML, Plaza-Manzano G, et al. Prevalence of post-COVID-19 symptoms in hospitalized and non-hospitalized COVID-19 survivors: a systematic review and meta-analysis. Eur J Intern Med. 2021; 92:55–70. PMID: 34167876.39. Goërtz YMJ, Van Herck M, Delbressine JM, Vaes AW, Meys R, Machado FVC, et al. Persistent symptoms 3 months after a SARS-CoV-2 infection: the post-COVID-19 syndrome? ERJ Open Res. 2020; 6(4):00542-2020. PMID: 33257910.40. Malik P, Patel K, Pinto C, Jaiswal R, Tirupathi R, Pillai S, et al. Post-acute COVID-19 syndrome (PCS) and health-related quality of life (HRQoL)-a systematic review and meta-analysis. J Med Virol. 2022; 94(1):253–262. PMID: 34463956.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- One Year Follow-Up of COVID-19 Related Symptoms and Patient Quality of Life: A Prospective Cohort Study
- Balance Ability and Quality of Life in Older Adult with Recovery from Mild COVID-19
- Evaluation and follow-up of pain, fatigue, and quality of life in COVID-19 patients
- Factors Affecting on the Quality of Life of the Elderly with Mild Dementia Living in Some Rural Community in Korea
- Factors affecting depression and health-related quality of life in the elderly during the COVID-19 pandemic