Neurointervention.
2022 Nov;17(3):174-182. 10.5469/neuroint.2022.00199.
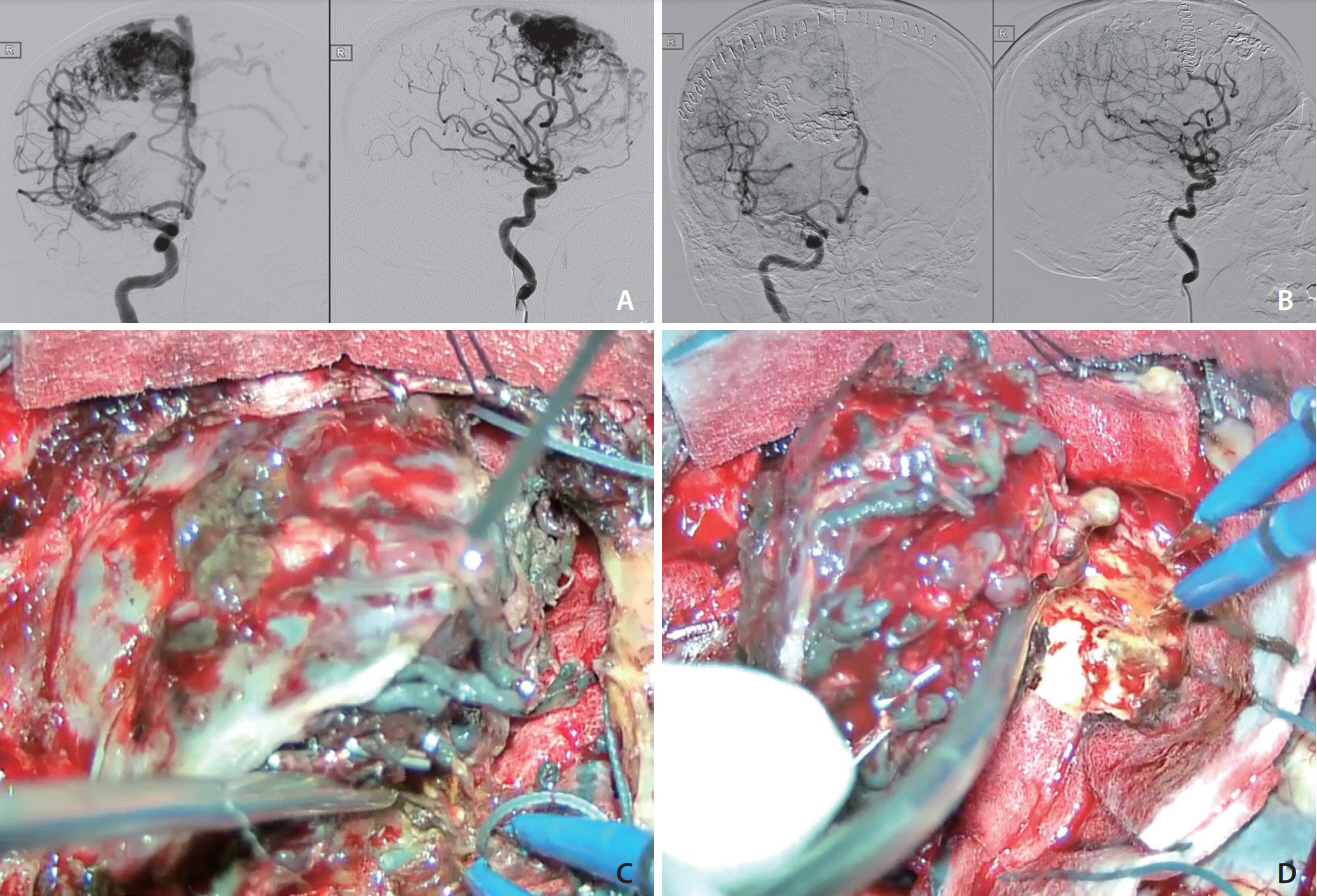
PHIL and Squid Embolization of Cerebral Arteriovenous Malformation: A Retrospective Case Series of 23 Patients
- Affiliations
-
- 1Division of Neurosurgery, Department of Surgery, Prince of Wales Hospital, The Chinese University of Hong Kong, Hong Kong, China
- 2Department of Neurosurgery, Pamela Youde Nethersole Eastern Hospital, Hong Kong, China
- 3Department of Imaging and Interventional Radiology, Prince of Wales Hospital, The Chinese University of Hong Kong, Hong Kong, China
- 4Department of Neurosurgery, Queen Mary Hospital, Hong Kong, China
- KMID: 2535953
- DOI: http://doi.org/10.5469/neuroint.2022.00199
Abstract
- Precipitating hydrophobic injectable liquid (PHIL; MicroVention, Aliso Viejo, CA, USA) and Squid (Balt, Irvine, CA, USA) are 2 newer liquid embolic agents used in endovascular embolization of cerebral arteriovenous malformation (AVM). This study aims to investigate and compare the effectiveness and safety profile of the 2 newer liquid embolic agents in the embolization of cerebral AVM. This is a retrospective study on all patients diagnosed with cerebral AVM undergoing endovascular embolization with liquid embolic agents PHIL and Squid admitted to the Division of Neurosurgery, Department of Surgery in Prince of Wales Hospital from January 2014 to June 2021. Twenty-three patients with cerebral AVM were treated with 34 sessions of endovascular embolization with either PHIL or Squid (17 sessions each) liquid embolic agents with a male to female ratio of 2.3:1 (male 16; female 7) and mean age of 44.6 (range, 12 to 67). The mean total nidus obliteration rate per session was 57% (range, 5% to 100%). Twenty-one patients (91.3%) received further embolization, stereotactic radiosurgery, or surgical excision after initial endovascular embolization. There were 2 morbidities (1 neurological and 1 non-neurological, 6%) and no mortalities (0%). All patients had static or improvement in modified Rankin Scale at 3 to 6 months at discharge. PHIL and Squid are effective and safe liquid embolic agents for endovascular embolization of cerebral AVM, achieving satisfactory nidal obliteration rates and patient functional outcomes.
Keyword
Figure
Reference
-
1. Pierot L, Cognard C, Herbreteau D, Fransen H, van Rooij WJ, Boccardi E, et al. Endovascular treatment of brain arteriovenous malformations using a liquid embolic agent: results of a prospective, multicentre study (BRAVO). Eur Radiol. 2013; 23:2838–2845.
Article2. Lawton MT, Rutledge WC, Kim H, Stapf C, Whitehead KJ, Li DY, et al. Brain arteriovenous malformations. Nat Rev Dis Primers. 2015; 1:15008.
Article3. Chan DYC, Chan DTM, Zhu CXL, Kan PKY, Ng AY, Hsieh YS, et al. Awake craniotomy for excision of arteriovenous malformations? A qualitative comparison study with stereotactic radiosurgery. J Clin Neurosci. 2018; 51:52–56.
Article4. Vollherbst DF, Chapot R, Bendszus M, Möhlenbruch MA. Glue, onyx, squid or PHIL? Liquid embolic agents for the embolization of cerebral arteriovenous malformations and dural arteriovenous fistulas. Clin Neuroradiol. 2022; 32:25–38.
Article5. Koçer N, Hanımoğlu H, Batur Ş, Kandemirli SG, Kızılkılıç O, Sanus Z, et al. Preliminary experience with precipitating hydrophobic injectable liquid in brain arteriovenous malformations. Diagn Interv Radiol. 2016; 22:184–189.
Article6. Samaniego EA, Kalousek V, Abdo G, Ortega-Gutierrez S. Preliminary experience with precipitating hydrophobic injectable liquid (PHIL) in treating cerebral AVMs. J Neurointerv Surg. 2016; 8:1253–1255.
Article7. Akmangit I, Daglioglu E, Kaya T, Alagoz F, Sahinoglu M, Peker A, et al. Preliminary experience with squid: a new liquid embolizing agent for AVM, AV fistulas and tumors. Turk Neurosurg. 2014; 24:565–570.8. Tam AKY, Chan DYC, Lim K, Poon D, Kam M, Cheung M, et al. Long term treatment efficacy & complications of hypofractionated stereotactic radiosurgery in brain arteriovenous malformations. J Clin Neurosci. 2020; 82(Pt B):241–246.
Article9. Wong GK, Kam MK, Chiu SK, Lam JM, Leung CH, Ng DW, et al. Validation of the modified radiosurgery-based arteriovenous malformation score in a linear accelerator radiosurgery experience in Hong Kong. J Clin Neurosci. 2012; 19:1252–1254.
Article10. Mason JR, Dodge C, Benndorf G. Quantification of tantalum sedimentation rates in liquid embolic agents. Interv Neuroradiol. 2018; 24:574–579.
Article11. Schmitt N, Floca RO, Paech D, El Shafie RA, Neuberger U, Bendszus M, et al. Imaging artifacts of nonadhesive liquid embolic agents in conventional and cone-beam CT in a novel in vitro AVM model. Clin Neuroradiol. 2021; 31:1141–1148.
Article12. Schmitt N, Weyland CS, Wucherpfennig L, Sommer CM, Bendszus M, Möhlenbruch MA, et al. The impact of software-based metal artifact reduction on the liquid embolic agent onyx in cone-beam CT: a systematic in vitro and in vivo study. J Neurointerv Surg. 2022; 14:832–836.
Article13. Samaniego EA, Derdeyn CP, Hayakawa M, Hasan D, OrtegaGutierrez S. In vivo evaluation of the new PHIL low viscosity in a swine rete mirabile model. Interv Neuroradiol. 2018; 24:706–712.
Article14. Mohr JP, Parides MK, Stapf C, Moquete E, Moy CS, Overbey JR, international ARUBA investigators, et al. Medical management with or without interventional therapy for unruptured brain arteriovenous malformations (ARUBA): a multicentre, non-blinded, randomised trial. Lancet. 2014; 383:614–621.
Article15. Elsenousi A, Aletich VA, Alaraj A. Neurological outcomes and cure rates of embolization of brain arteriovenous malformations with n-butyl cyanoacrylate or onyx: a meta-analysis. J Neurointerv Surg. 2016; 8:265–272.
Article16. Jayaraman MV, Marcellus ML, Hamilton S, Do HM, Campbell D, Chang SD, et al. Neurologic complications of arteriovenous malformation embolization using liquid embolic agents. AJNR Am J Neuroradiol. 2008; 29:242–246.
Article17. Taylor CL, Dutton K, Rappard G, Pride GL, Replogle R, Purdy PD, et al. Complications of preoperative embolization of cerebral arteriovenous malformations. J Neurosurg. 2004; 100:810–812.
Article18. Ledezma CJ, Hoh BL, Carter BS, Pryor JC, Putman CM, Ogilvy CS. Complications of cerebral arteriovenous malformation embolization: multivariate analysis of predictive factors. Neurosurgery. 2006; 58:602–611. discussion 602-611.
Article19. Hartmann A, Pile-Spellman J, Stapf C, Sciacca RR, Faulstich A, Mohr JP, et al. Risk of endovascular treatment of brain arteriovenous malformations. Stroke. 2002; 33:1816–1820.
Article20. Haw CS, terBrugge K, Willinsky R, Tomlinson G. Complications of embolization of arteriovenous malformations of the brain. J Neurosurg. 2006; 104:226–232.
Article21. Sirakov SS, Sirakov A, Minkin K, Hristov H, Ninov K, Penkov M, et al. Initial experience with precipitating hydrophobic injectable liquid in cerebral arteriovenous malformations. Interv Neuroradiol. 2019; 25:58–65.
Article22. Luessenhop AJ, Spence WT. Artificial embolization of cerebral arteries. Report of use in a case of arteriovenous malformation. J Am Med Assoc. 1960; 172:1153–1155.23. Wong GK, Yu SC, Zhu XL, Kam MK, Poon WS. Use of onyx (a patented ethylene-vinyl alcohol copolymer formulation) embolisation of cerebral arteriovenous malformations in Hong Kong: initial experience. Hong Kong Med J. 2009; 15:359–364.24. Flores BC, See AP, Weiner GM, Jankowitz BT, Ducruet AF, Albuquerque FC. Use of the Apollo detachable-tip microcatheter for endovascular embolization of arteriovenous malformations and arteriovenous fistulas. J Neurosurg. 2018; 130:963–971.
Article25. Mendes GAC, Kalani MYS, Iosif C, Lucena AF, Carvalho R, Saleme S, et al. Transvenous curative embolization of cerebral arteriovenous malformations: a prospective cohort study. Neurosurgery. 2018; 83:957–964.
Article26. Koyanagi M, Mosimann PJ, Nordmeyer H, Heddier M, Krause J, Narata AP, et al. The transvenous retrograde pressure cooker technique for the curative embolization of high-grade brain arteriovenous malformations. J Neurointerv Surg. 2021; 13:637–641.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Hemodynamic Instability during Squid Embolization of Dural Arteriovenous Fistula: A Case Report
- Pathophysiology of Cerebral Arteiovenous Malformation
- A Case of Multiple Pulmonary Arteriovenous Malformation Treated with Coil Embolization
- Complication Associated with Onyx Embolization of Spinal Cord Arteriovenous Malformation
- A Case of Arteriovenous Malformation of the Nasal Tip