Neurointervention.
2022 Nov;17(3):161-167. 10.5469/neuroint.2022.00332.
Endovascular Treatment of Arterial Steno-Occlusive Lesions in Symptomatic Moyamoya Disease
- Affiliations
-
- 1Department of Radiology, Research Institute of Radiology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2535951
- DOI: http://doi.org/10.5469/neuroint.2022.00332
Abstract
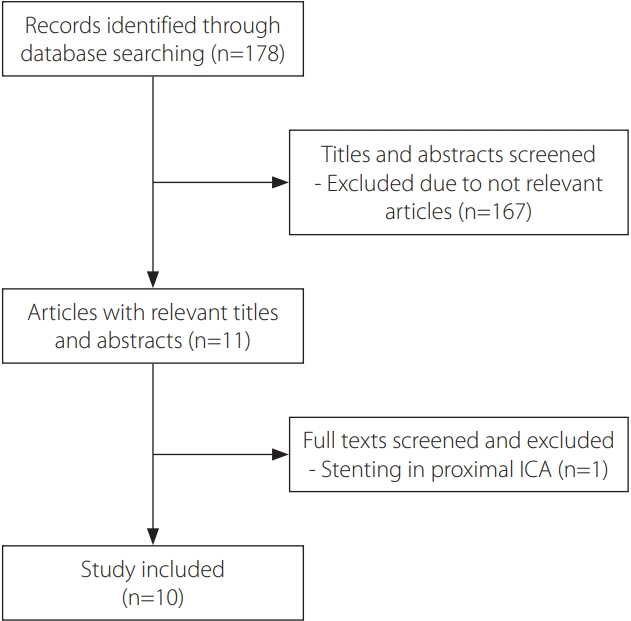
- The efficacy and safety of endovascular treatment (EVT) for moyamoya disease (MMD) have rarely been investigated. The objective of this study was to summarize the clinical outcomes of EVT for MMD and determine the potential role of EVT in treating symptomatic steno-occlusive lesions in MMD. Reports from January 2000 to December 2021 describing EVT in MMD were collected through a literature search. The search terms included “moyamoya”, “stent”, “angioplasty”, and “endovascular”. Data regarding baseline demographics, previous medical history, treated vessel, periprocedural complications, and angiographical recurrence were retrieved. This review included 10 studies with details of 19 patients undergoing a total of 31 EVT procedures. Twenty-one EVTs were performed as initial treatments for MMD, and 10 were performed as additional treatments for angiographical recurrence. The mean follow-up period of the initial EVTs was 9.0±11.9 months, with angiographical recurrence in 11 (68.8%) cases. The mean follow-up period of additional EVTs was 4.3±3.9 months, and seven (70.0%) EVTs showed restenosis of the re-treated vessel. Across all initial and additional EVTs, there were no differences in characteristics between the recurrence and non-recurrence groups. Overall, two periprocedural complications (9.5%) occurred, one vessel rupture and one massive intracerebral hemorrhage with subarachnoid hemorrhage. EVT plays a limited role in the management of symptomatic intracranial arterial steno-occlusive lesions of MMD. Recent advances in understanding the pathomechanism of MMD may urge neuro-interventionists to find a new endovascular approach with better balloon angioplasty or stenting mechanisms.
Keyword
Figure
Cited by 1 articles
-
Medical Management of Adult Moyamoya Disease: A Review and Relevant Cases With Ischemic Events
Oh Young Bang, Miki Fujimura
J Stroke. 2025;27(1):1-18. doi: 10.5853/jos.2024.04273.
Reference
-
1. Kim T, Lee H, Bang JS, Kwon OK, Hwang G, Oh CW. Epidemiology of Moyamoya disease in Korea: based on National Health Insurance Service Data. J Korean Neurosurg Soc. 2015; 57:390–395.
Article2. Powers WJ, Clarke WR, Grubb RL Jr, Videen TO, Adams HP Jr, Derdeyn CP; COSS Investigators. Extracranial-intracranial bypass surgery for stroke prevention in hemodynamic cerebral ischemia: the carotid occlusion surgery study randomized trial. JAMA. 2011; 306:1983–1992.
Article3. Kuroda S, Houkin K. Moyamoya disease: current concepts and future perspectives. Lancet Neurol. 2008; 7:1056–1066.
Article4. Kim T, Oh CW, Bang JS, Kim JE, Cho WS. Moyamoya disease: treatment and outcomes. J Stroke. 2016; 18:21–30.
Article5. Natarajan SK, Karmon Y, Tawk RG, Hauck EF, Hopkins LN, Siddiqui AH, et al. Endovascular treatment of patients with intracranial stenosis with Moyamoya-type collaterals. J Neurointerv Surg. 2011; 3:369–374.
Article6. Khan N, Dodd R, Marks MP, Bell-Stephens T, Vavao J, Steinberg GK. Failure of primary percutaneous angioplasty and stenting in the prevention of ischemia in Moyamoya angiopathy. Cerebrovasc Dis. 2011; 31:147–153.
Article7. Drazin D, Calayag M, Gifford E, Dalfino J, Yamamoto J, Boulos AS. Endovascular treatment for Moyamoya disease in a Caucasian twin with angioplasty and Wingspan stent. Clin Neurol Neurosurg. 2009; 111:913–917.
Article8. Argetsinger DS, Miller JW, Fletcher JJ. Intravenous thrombolysis, mechanical embolectomy, and intracranial stenting for hyperacute ischemic stroke in a patient with Moyamoya disease. J Clin Neurosci. 2016; 29:173–175.
Article9. Eicker S, Etminan N, Turowski B, Steiger HJ, Hänggi D. Intracranial carotid artery stent placement causes delayed severe intracranial hemorrhage in a patient with Moyamoya disease. J Neurointerv Surg. 2011; 3:160–162.
Article10. Rodriguez GJ, Kirmani JF, Ezzeddine MA, Qureshi AI. Primary percutaneous transluminal angioplasty for early Moyamoya disease. J Neuroimaging. 2007; 17:48–53.
Article11. El-Hakam LM, Volpi J, Mawad M, Clark G. Angioplasty for acute stroke with pediatric Moyamoya syndrome. J Child Neurol. 2010; 25:1278–1283.
Article12. Kim T, Kwon OK, Oh CW, Bang JS, Hwang G, Lee YJ. Intracranial stenting using a drug-eluting stent for Moyamoya disease involving supraclinoid ICA: a case report. Neurol Med Chir (Tokyo). 2014; 54:136–138.
Article13. Santirso D, Oliva P, González M, Murias E, Vega P, Gil A, et al. Intracranial stent placement in a patient with Moyamoya disease. J Neurol. 2012; 259:170–171.
Article14. Kornblihtt LI, Cocorullo S, Miranda C, Lylyk P, Heller PG, Molinas FC. Moyamoya syndrome in an adolescent with essential thrombocythemia: successful intracranial carotid stent placement. Stroke. 2005; 36:E71–E73.15. Gross BA, Thomas AJ, Frerichs KU. Endovascular treatment of symptomatic Moyamoya. Neurosurg Rev. 2014; 37:579–583.
Article16. Ohkubo K, Sakai Y, Inoue H, Akamine S, Ishizaki Y, Matsushita Y, et al. Moyamoya disease susceptibility gene RNF213 links inflammatory and angiogenic signals in endothelial cells. Sci Rep. 2015; 5:13191.
Article17. Han C, Li ML, Xu YY, Ye T, Xie CF, Gao S, et al. Adult Moyamoya-atherosclerosis syndrome: clinical and vessel wall imaging features. J Neurol Sci. 2016; 369:181–184.
Article18. Kim HJ, Choi EH, Chung JW, Kim JH, Kim YS, Seo WK, et al. Role of the RNF213 variant in vascular outcomes in patients with intracranial atherosclerosis. J Am Heart Assoc. 2021; 10:e017660.
Article19. Miyamoto S, Yoshimoto T, Hashimoto N, Okada Y, Tsuji I, Tominaga T, JAM Trial Investigators, et al. Effects of extracranial-intracranial bypass for patients with hemorrhagic Moyamoya disease: results of the Japan Adult Moyamoya Trial. Stroke. 2014; 45:1415–1421.
Article20. Morice MC, Serruys PW, Sousa JE, Fajadet J, Ban Hayashi E, Perin M, RAVEL Study Group, et al. A randomized comparison of a sirolimus-eluting stent with a standard stent for coronary revascularization. N Engl J Med. 2002; 346:1773–1780.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endovascular Management for Chronic Steno-occlusion of Iliac and Femoral Arteries
- A Case of Neurofibromatosis Associated with Moyamoya Disease
- Endovascular Revascularization for Aortoiliac Occlusive Disease
- The Relationship between Cerebral Infarction on MR and Angiographic Findings in Moyamoya Disease: Significance of the Posterior Circulation
- Intractable Coronary Spasm Requiring Percutaneous Coronary Intervention after Coronary Artery Bypass Grafting in a Patient with Moyamoya Disease