J Korean Neurosurg Soc.
2022 Nov;65(6):868-874. 10.3340/jkns.2022.0061.
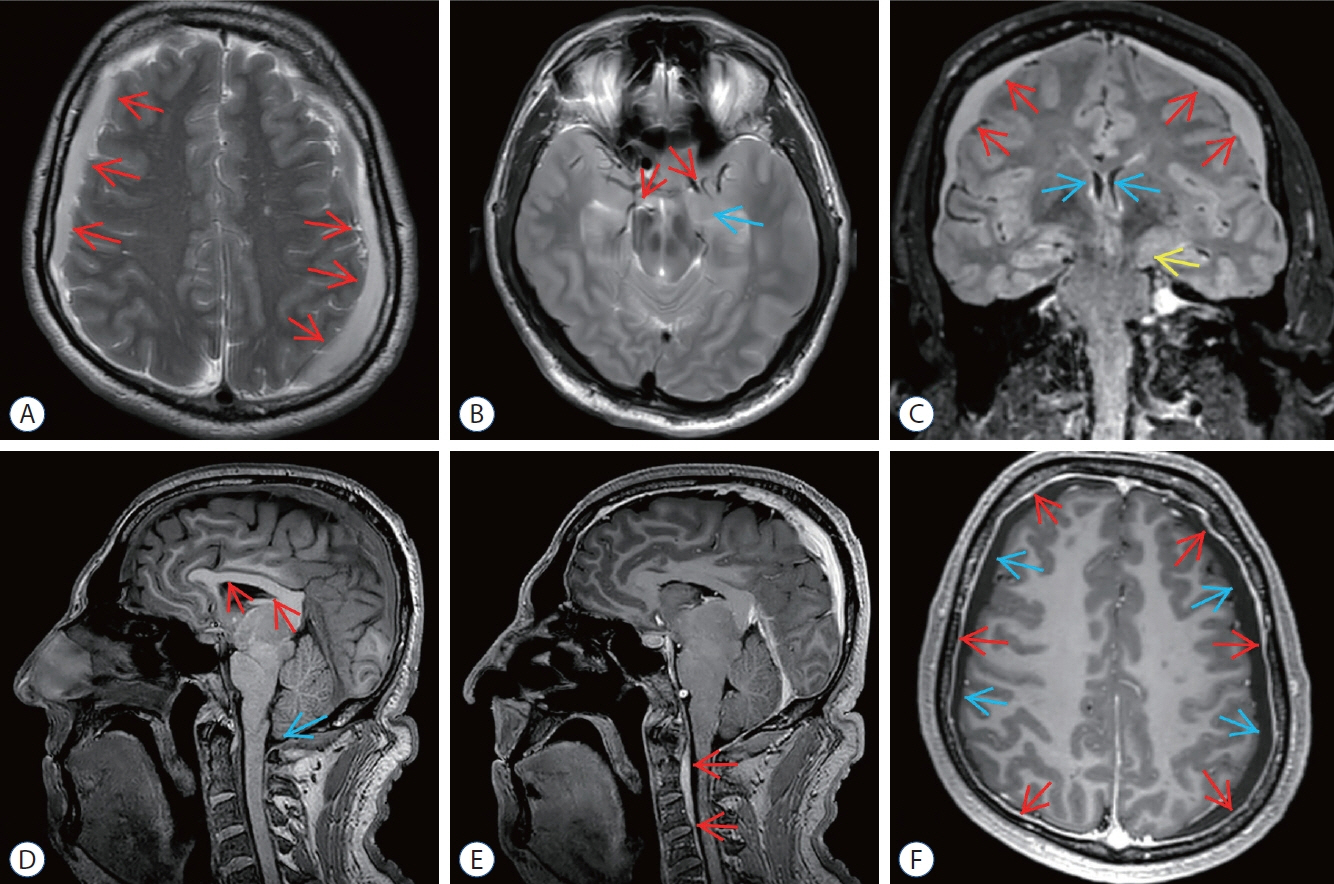
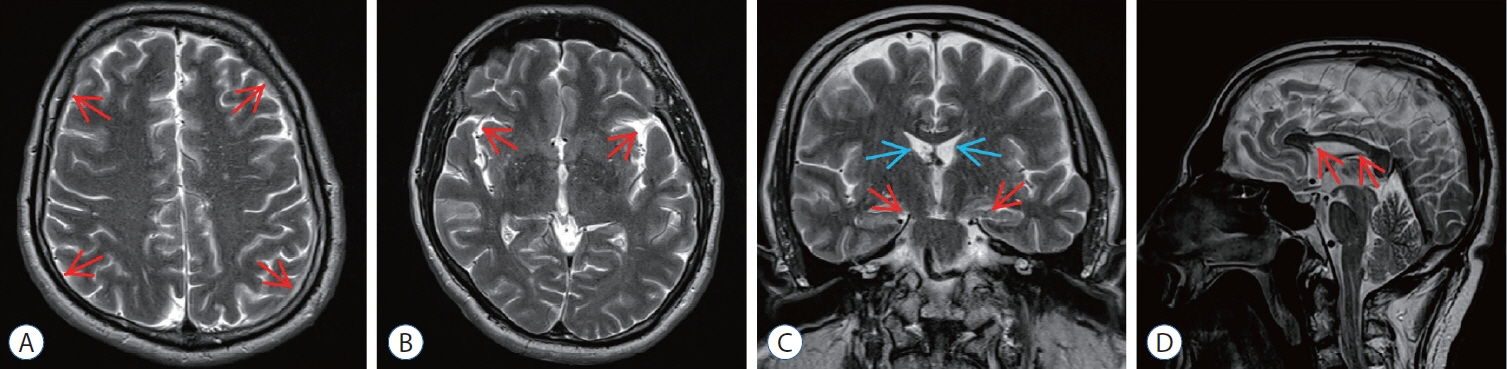
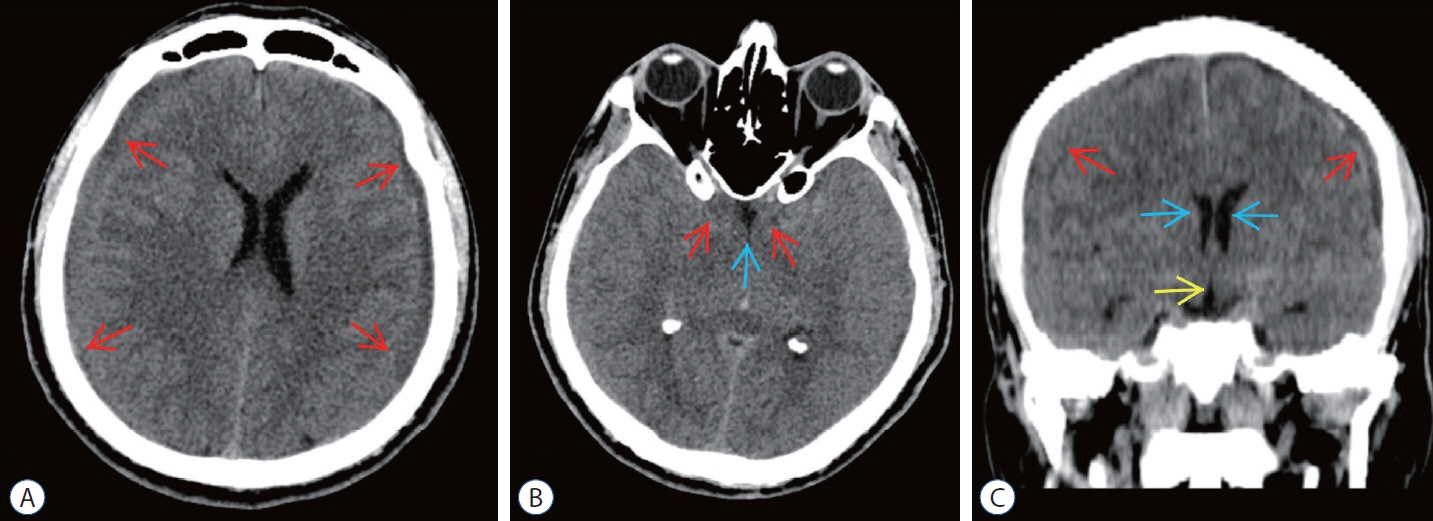
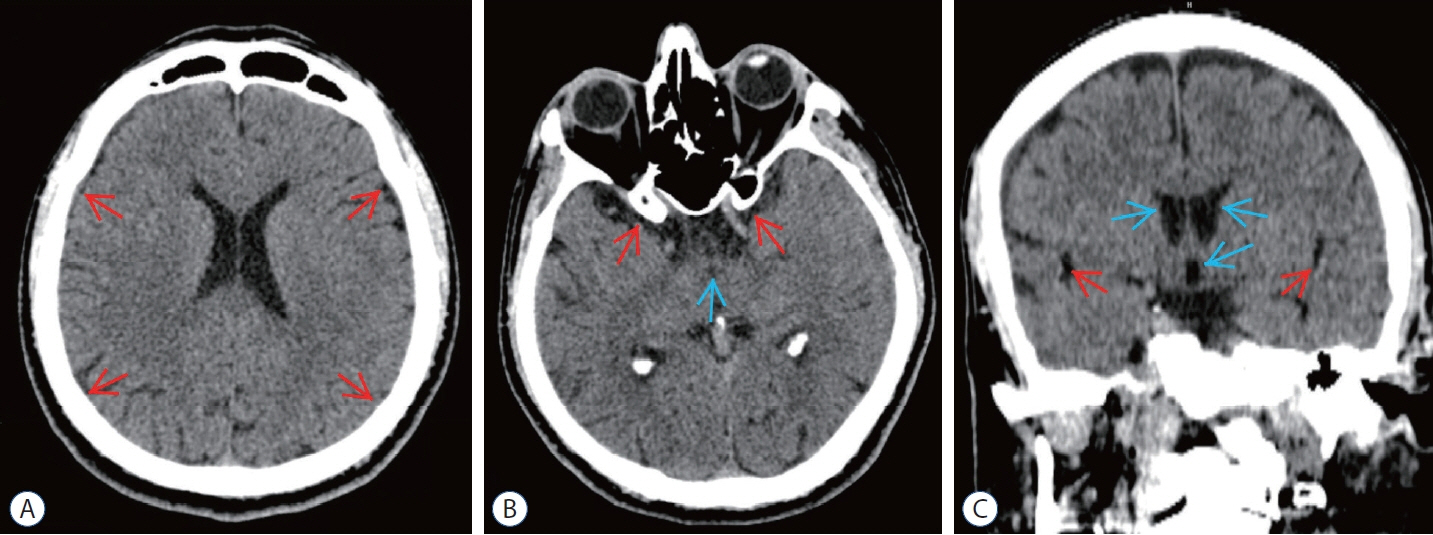
Efficacy of Middle Meningeal Artery Embolization in Treatment Resistant Spontaneous Intracranial Hypotension Caused Subdural Hematoma : Report of Two Cases and Review of the Literature
- Affiliations
-
- 1Department of Neurosurgery, Haseki Training and Research Hospital, University of Health Sciences, İstanbul, Turkey
- 2Department of Neurosurgery, İstanbul Medipol University, İstanbul, Turkey
- 3Department of Radiology, Başakşehir Çam And Sakura City Hospital, İstanbul, Turkey
- KMID: 2535848
- DOI: http://doi.org/10.3340/jkns.2022.0061
Abstract
- Spontaneous intracranial hypotension (SIH) most commonly manifests as bilateral subdural hematoma (SH). SIH cases mostly resolve spontaneously but further treatment would be needed via blind epidural blood patch (EBP). Cerebrospinal fluid (CSF) leakage in EBP-refractory cases can be treated surgically only if the localization of CSF leakage is detectable but it cannot be possible in most of the cases. Also surgical evacuation of SH secondary to SIH (SH-SIH) is not favorable without blocking the CSF leakage. Thus the management of these patients is a challenge and alternative treatment options are needed. Although middle meningeal artery embolization (MMAE) is an effective treatment option in non-SIH SH, there is no report about its application in the treatment of SH-SIH. We present two cases of SH-SIH which their clinical and radiological findings were completely resolved by bilateral MMAE treatment.
Figure
Reference
-
References
1. Ahn C, Lee E, Lee JW, Chee CG, Kang Y, Kang HS. Two-site blind epidural blood patch versus targeted epidural blood patch in spontaneous intracranial hypotension. J Clin Neurosci. 62:147–154. 2019.2. Ban SP, Hwang G, Byoun HS, Kim T, Lee SU, Bang JS, et al. Middle meningeal artery embolization for chronic subdural hematoma. Radiology. 286:992–999. 2018.3. Cho KI, Moon HS, Jeon HJ, Park K, Kong DS. Spontaneous intracranial hypotension: efficacy of radiologic targeting vs blind blood patch. Neurology. 76:1139–1144. 2011.4. Chotai S, Kim JH, Kim JH, Kwon TH. Brain herniation induced by drainage of subdural hematoma in spontaneous intracranial hypotension. Asian J Neurosurg. 8:112–115. 2013.5. Chung SJ, Kim JS, Lee MC. Syndrome of cerebral spinal fluid hypovolemia: clinical and imaging features and outcome. Neurology. 55:1321–1327. 2000.6. Dhillon AK, Rabinstein AA, Wijdicks EF. Coma from worsening spontaneous intracranial hypotension after subdural hematoma evacuation. Neurocrit Care. 12:390–394. 2010.7. Ferrante E, Rubino F, Beretta F, Regna-Gladin C, Ferrante MM. Treatment and outcome of subdural hematoma in patients with spontaneous intracranial hypotension: a report of 35 cases. Acta Neurol Belg. 118:61–70. 2018.8. Forghani R, Farb RI. Diagnosis and temporal evolution of signs of intracranial hypotension on MRI of the brain. Neuroradiology. 50:1025–1034. 2008.9. García-Morales I, Porta-Etessam J, Galán L, Lagares A, Molina JA. Recurrent subdural haematomas in a patient with spontaneous intracranial hypotension. Cephalalgia. 21:703–705. 2001.10. Girão MMV, Sousa RMP, Ribeiro MC, Cardoso TAM de O, França Júnior MC, Reis F. Spontaneous intracranial hypotension and its complications. Arq Neuropsiquiatr. 76:507–511. 2018.11. Headache Classification Committee of the International Headache Society (IHS). The international classification of headache disorders, 3rd edition (beta version). Cephalalgia. 33:629–808. 2013.12. Inenaga C, Tanaka T, Sakai N, Nishizawa S. Diagnostic and surgical strategies for intractable spontaneous intracranial hypotension. Case report. J Neurosurg. 94:642–645. 2001.13. Link TW, Boddu S, Marcus J, Rapoport BI, Lavi E, Knopman J. Middle meningeal artery embolization as treatment for chronic subdural hematoma: a case series. Oper Neurosurg (Hagerstown). 14:556–562. 2018.14. Link TW, Boddu S, Paine SM, Kamel H, Knopman J. Middle meningeal artery embolization for chronic subdural hematoma: a series of 60 cases. Neurosurgery. 85:801–807. 2019.15. Link TW, Schwarz JT, Paine SM, Kamel H, Knopman J. Middle meningeal artery embolization for recurrent chronic subdural hematoma: a case series. World Neurosurg. 118:e570–e574. 2018.16. Schievink WI, Maya MM, Moser FG, Tourje J. Spectrum of subdural fluid collections in spontaneous intracranial hypotension. J Neurosurg. 103:608–613. 2005.17. Takahashi K, Mima T, Akiba Y. Chronic subdural hematoma associated with spontaneous intracranial hypotension: therapeutic strategies and outcomes of 55 cases. Neurol Med Chir (Tokyo). 56:69–76. 2016.18. Wu JW, Hseu SS, Fuh JL, Lirng JF, Wang YF, Chen WT, et al. Factors predicting response to the first epidural blood patch in spontaneous intracranial hypotension. Brain. 140:344–352. 2017.19. Yadav YR, Parihar V, Namdev H, Bajaj J. Chronic subdural hematoma. Asian J Neurosurg. 11:330–342. 2016.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Delayed-Onset Subdural Hematoma and Oculomotor Nerve Palsy After Improving Spontaneous Intracranial Hypotension
- Usefulness of Middle Meningeal Embolization to Prevent Recurrent Spontaneous Chronic Subdural Hemorrhage
- Spontaneous Spinal Subdural and Subarachnoid Hemorrhage with Concomitant Intracerebral Hemorrhage: A Case Report
- A Case of Spontaneous Intracranial Hypotension with Subdural Hematoma Mimicking Meningitis
- Spontaneous Intracranial Hypotension, a Possible Cause of Chronic Subdural Hematoma