J Korean Neurosurg Soc.
2022 Nov;65(6):825-833. 10.3340/jkns.2021.0296.
Comparative Analysis of ABM/P-15, Bone Morphogenic Protein and Demineralized Bone Matrix after Instrumented Lumbar Interbody Fusion
- Affiliations
-
- 1Department of Neurological Surgery, Wooridul Spine Hospital, Seoul, Korea
- 2Department of Orthopedic Surgery, Wooridul Spine Hospital, Seoul, Korea
- KMID: 2535842
- DOI: http://doi.org/10.3340/jkns.2021.0296
Abstract
Objective
: ABM/P-15 (anorganic bone matrix/15-amino acid peptide fragment) is a commercially available synthetically manufactured P-15 collagen peptide fragment, that is adsorbed on ABM. This study was done to investigate the efficacy of ABM/ P-15 in achieving fusion in the lumbar spine and comparing it with that of recombinant bone morphogenic protein-2 (rhBMP-2) and demineralized bone matrix (DBM).
Methods
: A retrospective observational study of prospectively collected data of 140 patients who underwent lumbar spinal fusion surgeries in a single specialty spine hospital between 2016 and 2020, with a minimum 6-month follow-up was conducted. Based on the material used for the augmentation of the bone graft at the fusion site, the patients were divided into three categories namely ABM/P-15, rhBMP-2, and DBM group.
Results
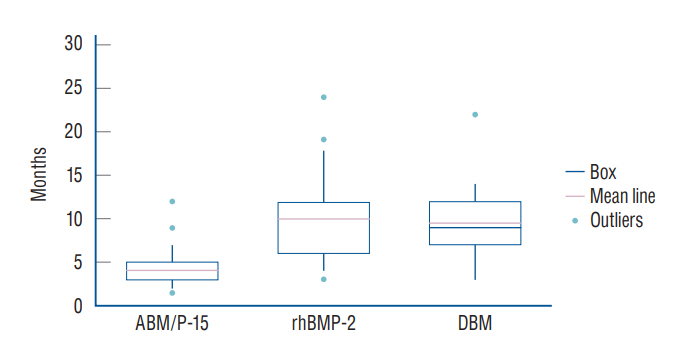
: ABM/P-15, rhBMP-2, and DBM were used in 46, 44, and 50 patients, respectively. Patient characteristics like age, gender, bone mineral density, smoking history, and presence of diabetes mellitus were comparable amongst the three groups. Average follow-up was 16.0±5.2, 17.9±9.8, and 26.2±14.9 months, respectively in ABM/P-15, rhBMP-2, and DBM groups. The fusion was achieved in 97.9%, 93.2%, and 98% patients while the average time-to-union was 4.05±2.01, 10±4.28, and 9.44±3.49 months (p<0.001), respectively for ABM/P-15, rhBMP-2, and DBM groups. The average pre-operative Visual analogue scale score was 6.93±2.42, 7.14±1.97, 7.01±2.14 (p=0.900) for ABM/P-15, rhBMP-2 and DBM groups, respectively, which reduced to 1.02±0.80, 1.21±0.96, and 0.54±0.70 (p=0.112), respectively at the last follow up. Pre-operative Oswestry disability index scores were 52.7±18.02, 55.4±16.8, and 53.56±19.6 (p=0.751) in ABM/P-15, rhBMP-2, and DBM groups, which post-operatively reduced to 33.77±15.52, 39.42±16.47, and 38.3±15.89 (p=0.412) and further to 15.74±8.3, 17.41±10.45, and 16.76±9.81 (p=0.603), respectively at the last follow-up.
Conclusion
: ABM/P-15 appears to achieve union significantly earlier than rhBMP-2 and DBM in lumbar spinal fusion cases while maintaining a comparable clinical and complication profile.
Keyword
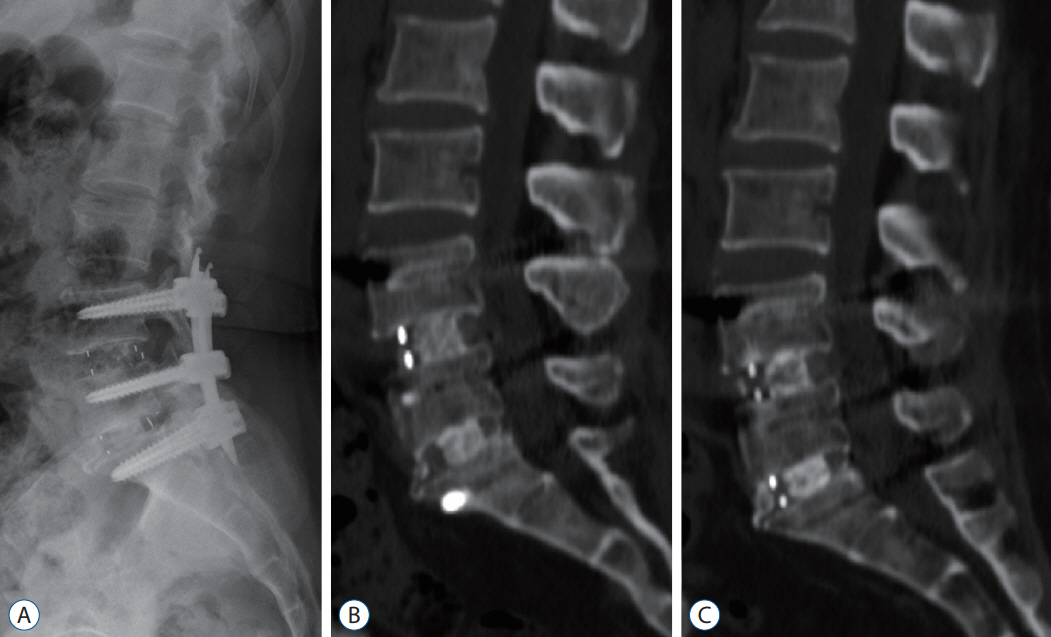
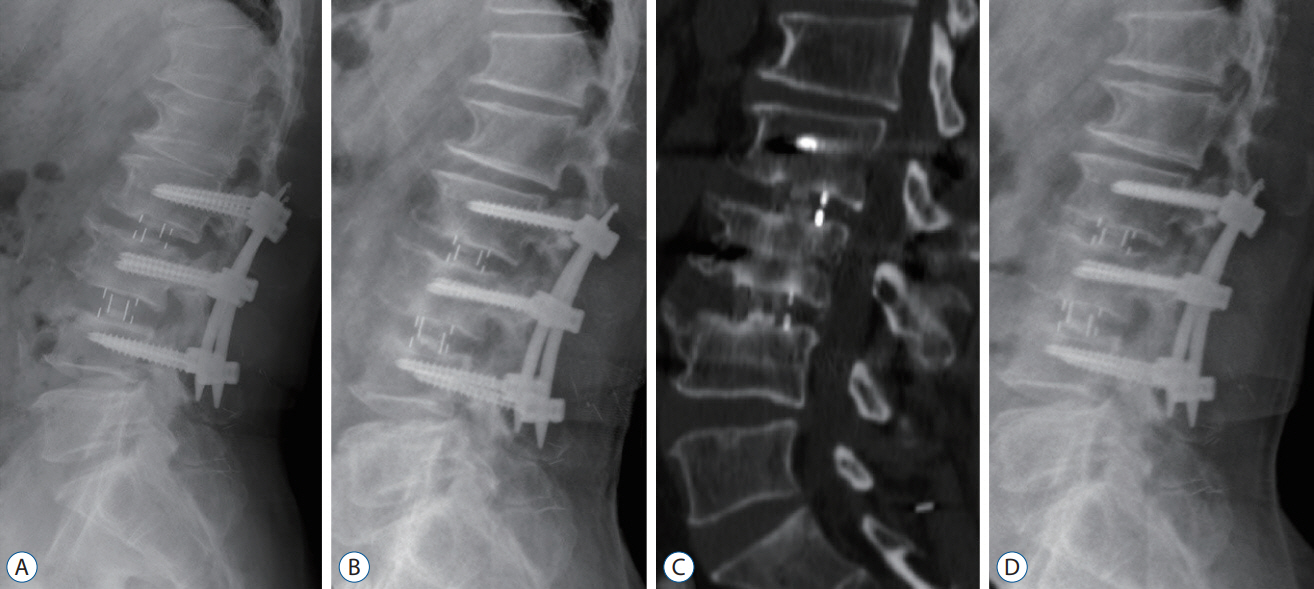
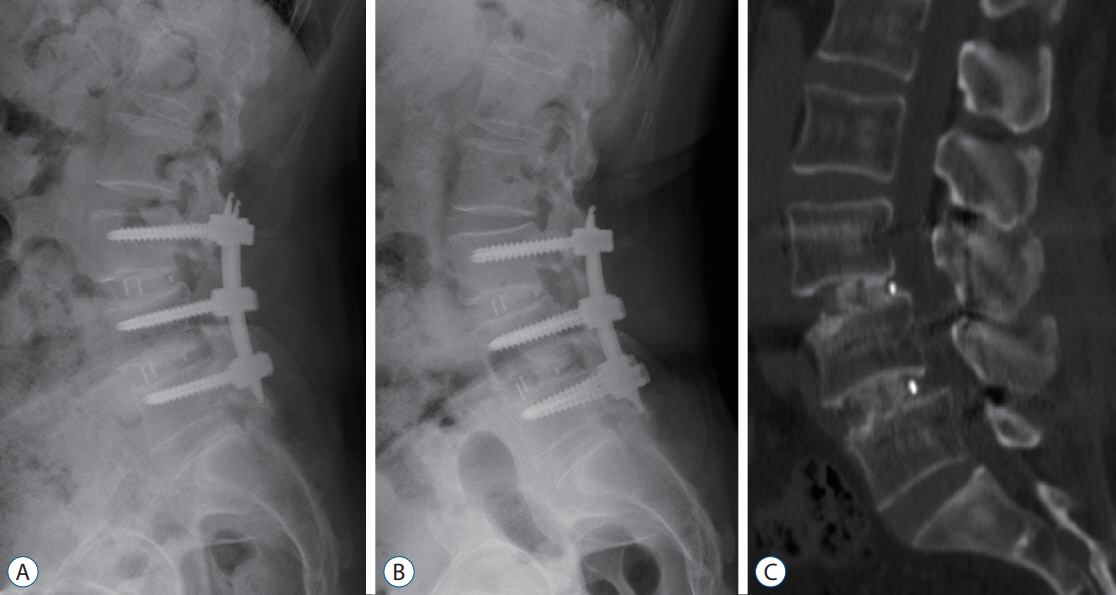
Figure
Reference
-
References
1. Arnold PM, Sasso RC, Janssen ME, Fehlings MG, Heary RF, Vaccaro AR, et al. i-Factor™ bone graft vs autograft in anterior cervical discectomy and fusion: 2-year follow-up of the randomized single-blinded food and drug administration investigational device exemption study. Clin Neurosurg. 83:377–384. 2018.2. Arnold PM, Sasso RC, Janssen ME, Fehlings MG, Smucker JD, Vaccaro AR, et al. Efficacy of i-Factor bone graft versus autograft in anterior cervical discectomy and fusion: results of the prospective, randomized, single-blinded Food and Drug Administration investigational device exemption study. Spine (Phila Pa 1976). 41:1075–1083. 2016.3. Bae J, Lee SH. Minimally invasive spinal surgery for adult spinal deformity. Neurospine. 15:18–24. 2018.4. Banwart JC, Asher MA, Hassanein RS. Iliac crest bone graft harvest donor site morbidity. A statistical evaluation. Spine (Phila Pa 1976). 20:1055–1060. 1995.5. Barros RR, Novaes AB Jr, Roriz VM, Oliveira RR, Grisi MF, Souza SL, et al. Anorganic bovine matrix/P-15 “flow” in the treatment of periodontal defects: case series with 12 months of follow-up. J Periodontol. 77:1280–1287. 2006.6. Bhatnagar RS, Qian JJ, Gough CA. The role in cell binding of a beta-bend within the triple helical region in collagen alpha 1 (I) chain: structural and biological evidence for conformational tautomerism on fiber surface. J Biomol Struct Dyn. 14:547–560. 1997.7. Carragee EJ, Hurwitz EL, Weiner BK. A critical review of recombinant human bone morphogenetic protein-2 trials in spinal surgery: emerging safety concerns and lessons learned. Spine J. 11:471–491. 2011.8. Chung HJ, Hur JW, Ryu KS, Kim JS, Seong JH. Surgical outcomes of anterior cervical fusion using deminaralized bone matrix as stand-alone graft material: single arm, pilot study. Korean J Spine. 13:114–119. 2016.9. Cook RW, Hsu WK. Ceramics: clinical evidence for ceramics in spine fusion. Semin Spine Surg. 28:217–225. 2016.10. Gomar F, Orozco R, Villar JL, Arrizabalaga F. P-15 small peptide bone graft substitute in the treatment of non-unions and delayed union. A pilot clinical trial. Int Orthop. 31:93–99. 2007.11. Gupta A, Kukkar N, Sharif K, Main BJ, Albers CE, El-Amin Iii SF. Bone graft substitutes for spine fusion: a brief review. World J Orthop. 6:449–456. 2015.12. Hanks T, Atkinson BL. Comparison of cell viability on anorganic bone matrix with or without P-15 cell binding peptide. Biomaterials. 25:4831–4836. 2004.13. Haws BE, Khechen B, Patel DV, Yoo JS, Guntin JA, Cardinal KL, et al. Impact of iliac crest bone grafting on postoperative outcomes and complication rates following minimally invasive transforaminal lumbar interbody fusion. Neurospine. 16:772–779. 2019.14. Jacobsen MK, Andresen AK, Jespersen AB, Støttrup C, Carreon LY, Overgaard S, et al. Randomized double blind clinical trial of ABM/P-15 versus allograft in noninstrumented lumbar fusion surgery. Spine J. 20:677–684. 2020.15. Katsuura Y, Shafi K, Jacques C, Virk S, Iyer S, Cunningham M. New strategies in enhancing spinal fusion. HSS J. 16:177–182. 2020.16. Kukreja S, Ahmed OI, Haydel J, Nanda A, Sin AH. Complications of anterior cervical fusion using a low-dose recombinant human bone morphogenetic protein-2. Korean J Spine. 12:68–74. 2015.17. Kyoh Y. Minimally invasive endoscopic-assisted lateral lumbar interbody fusion: technical report and preliminary results. Neurospine. 16:72–81. 2019.18. Lauweryns P, Raskin Y. Prospective analysis of a new bone graft in lumbar interbody fusion: results of a 2-year prospective clinical and radiological study. Int J Spine Surg. 9:2. 2015.19. Lee DY, Jung TG, Lee SH. Single-level instrumented mini-open transforaminal lumbar interbody fusion in elderly patients. J Neurosurg Spine. 9:137–144. 2008.20. Lim TK, Lee SG, Park CW, Kim WK, Son S, Lee K. Comparative analysis of adjacent levels of degeneration and clinical outcomes between conventional pedicle screws and percutaneous pedicle screws in treatment of degenerative disease at L3-5; a preliminary report. Korean J Spine. 9:66–73. 2012.21. Marchi L, Abdala N, Oliveira L, Amaral R, Coutinho E, Pimenta L. Radiographic and clinical evaluation of cage subsidence after stand-alone lateral interbody fusion. J Neurosurg Spine. 19:110–118. 2013.22. Martin BI, Mirza SK, Spina N, Spiker WR, Lawrence B, Brodke DS. Trends in lumbar fusion procedure rates and associated hospital costs for degenerative spinal diseases in the United States, 2004 to 2015. Spine (Phila Pa 1976). 44:369–376. 2019.23. Meisel HJ, Agarwal N. Commentary on “biomaterials in spinal implants: a review”. Neurospine. 17:111–113. 2020.24. Mobbs RJ, Chung M, Rao PJ. Bone graft substitutes for anterior lumbar interbody fusion. Orthop Surg. 5:77–85. 2013.25. Mobbs RJ, Maharaj M, Rao PJ. Clinical outcomes and fusion rates following anterior lumbar interbody fusion with bone graft substitute iFACTOR, an anorganic bone matrix/P-15 composite. J Neurosurg Spine. 21:867–876. 2014.26. Na YC, Lee HS, Shin DA, Ha Y, Kim KN, Yoon DH. Initial clinical outcomes of minimally invasive lateral lumbar interbody fusion in degenerative lumbar disease: a preliminary report on the experience of a single institution with 30 cases. Korean J Spine. 9:187–192. 2012.27. Nazareth CA, Cury PR. Use of anorganic bovine-derived hydroxyapatite matrix/cell-binding peptide (P-15) in the treatment isolated class i gingival recession of defects: a pilot study. J Periodontol. 82:700–707. 2011.28. Oxborrow N, Sundarapandian R. Heterotopic ossification following use of i-Factor for spinal fusion in mucopolysaccharidosis 1: a case report. J Surg Case Rep. 2018:rjy120. 2018.29. Sasso RC, LeHuec JC, Shaffrey C. Iliac crest bone graft donor site pain after anterior lumbar interbody fusion: a prospective patient satisfaction outcome assessment. J Spinal Disord Tech. 18:S77–S81. 2005.30. Sharma AK, Kepler CK, Girardi FP, Cammisa FP, Huang RC, Sama AA. Lateral lumbar interbody fusion: clinical and radiographic outcomes at 1 year: a preliminary report. J Spinal Disord Tech. 24:242–250. 2011.31. Vaccaro AR, Chiba K, Heller JG, Patel TCh, Thalgott JS, Truumees E, et al. Bone grafting alternatives in spinal surgery. Spine J. 2:206–215. 2002.32. Xi Z, Chou D, Mummaneni PV, Burch S. The navigated oblique lumbar interbody fusion: accuracy rate, effect on surgical time, and complications. Neurospine. 17:260–267. 2020.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Lumbar Posterolateral Fusion Using Demineralized Bone Matrix
- Effect of Mixture of Recombinant Human Bone Morphogenic Protein-2 and Demineralized Bone Matrix in Lateral Lumbar Interbody Fusion
- Bone Union Rate Following Instrumented Posterolateral Lumbar Fusion: Comparison between Demineralized Bone Matrix versus Hydroxyapatite
- Comparison of Fusion Rate between Demineralized Bone Matrix versus Autograft in Lumbar Fusion : Meta-Analysis
- Demineralized Bone Matrix, as a Graft Enhancer of Auto-Local Bone in Posterior Lumbar Interbody Fusion