Ann Clin Neurophysiol.
2022;24(2):107-110. 10.14253/acn.2022.24.2.107.
Adult-onset Leigh syndrome due to m.9176T>C mutation with cortical involvement
- Affiliations
-
- 1Department of Neurology, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 2Department of Neurology, Uijeongbu St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Uijeongbu, Korea
- KMID: 2535729
- DOI: http://doi.org/10.14253/acn.2022.24.2.107
Abstract
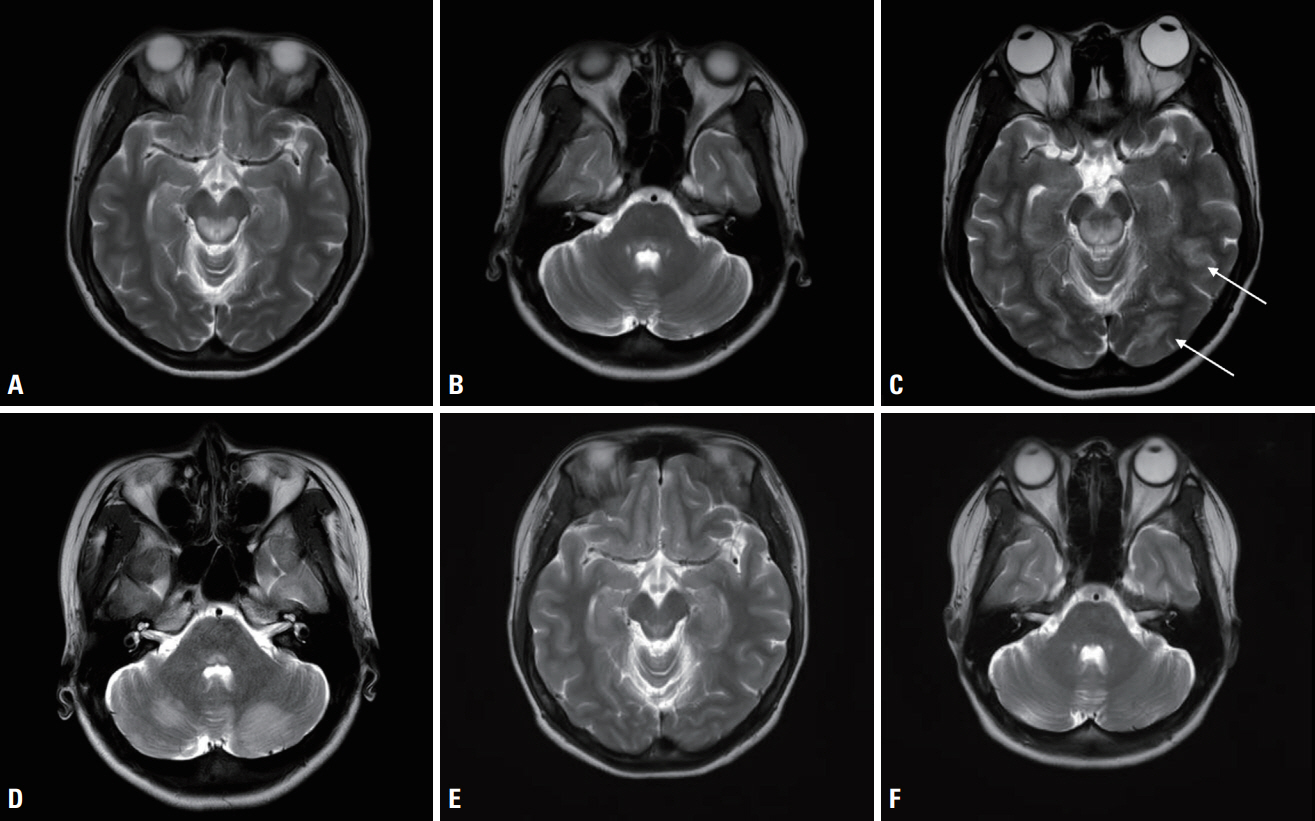
- We describe the case of a 22-year-old female complaining of ophthalmoplegia, which deteriorated with seizure. Leigh syndrome (LS) was diagnosed by identifying the m.9176T>C mutation. She improved with vitamin cocktail therapy plus intravenous methylprednisolone, and had an excellent prognosis. This was the first case of an adult patient with LS presenting with the m.9176T>C mutation and reporting cortical symptoms, which in this case comprised cortical vision loss, and cortical, basal ganglia, and brainstem signal changes on magnetic resonance imaging.
Figure
Reference
-
1. Rahman S, Blok RB, Dahl HH, Danks DM, Kirby DM, Chow CW, et al. Leigh syndrome: clinical features and biochemical and DNA abnormalities. Ann Neurol. 1996; 39:343–351.2. McKelvie P, Infeld B, Marotta R, Chin J, Thorburn D, Collins S. Lateadult onset Leigh syndrome. J Clin Neurosci. 2012; 19:195–202.3. Campos Y, Martín MA, Rubio JC, Solana LG, García-Benayas C, Terradas JL, et al. Leigh syndrome associated with the T9176C mutation in the ATPase 6 gene of mitochondrial DNA. Neurology. 1997; 49:595–597.4. Makino M, Horai S, Goto Y, Nonaka I. Confirmation that a T-to-C mutation at 9176 in mitochondrial DNA is an additional candidate mutation for Leigh’s syndrome. Neuromuscul Disord. 1998; 8:149–151.5. Ichikawa K, Tsuyusaki Y, Shimbo H, Goto T. Late-onset Leigh syndrome with m.9176T>C mutation in the mitochondrial ATPase 6 gene. Pediatr Int. 2019; 61:1055–1056.6. Ronchi D, Bordoni A, Cosi A, Rizzuti M, Fassone E, Di Fonzo A, et al. Unusual adult-onset Leigh syndrome presentation due to the mitochondrial m.9176T>C mutation. Biochem Biophys Res Commun. 2011; 412:245–248.7. Lake NJ, Compton AG, Rahman S, Thorburn DR. Leigh syndrome: one disorder, more than 75 monogenic causes. Ann Neurol. 2016; 79:190–203.8. Wei Y, Cui L, Peng B. Mitochondrial DNA mutations in late-onset Leigh syndrome. J Neurol. 2018; 265:2388–2395.9. Barcelos I, Shadiack E, Ganetzky RD, Falk MJ. Mitochondrial medicine therapies: rationale, evidence, and dosing guidelines. Curr Opin Pediatr. 2020; 32:707–718.10. Chuquilin M, Govindarajan R, Peck D, Font-Montgomery E. Response to immunotherapy in a patient with adult onset Leigh syndrome and T9176C mtDNA mutation. Mol Genet Metab Rep. 2016; 8:28–32.11. Sage-Schwaede A, Engelstad K, Salazar R, Curcio A, Khandji A, Garvin JH Jr, et al. Exploring mTOR inhibition as treatment for mitochondrial disease. Ann Clin Transl Neurol. 2019; 6:1877–1881.12. Hanaford A, Johnson SC. The immune system as a driver of mitochondrial disease pathogenesis: a review of evidence. Orphanet J Rare Dis. 2022; 17:335.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Leigh Syndrome Mimicking Wernicke's Encephalopathy: A Case Report
- Cardiac Arrest as the Initial Presentation of Leigh Syndrome Associated with Novel NDUFS1 Mutation
- Serial MRI Findings in a Clinically Diagnosed Adult Onset Leigh Syndrome
- Identification of causative mutations in patients with Leigh syndrome and MERRF by mitochondrial DNA-targeted next-generation sequencing
- Arterial hypertension in Leigh syndrome due to m.13513G > A is multicausal, requiring an extensive search to identify its pathphysiology