Acute Crit Care.
2022 Aug;37(3):391-397. 10.4266/acc.2022.00080.
The incidence of phlebitis development of high concentration of continuous amiodarone infusion with in-line filter compared to the low concentration without in-line filter: a retrospective propensity score-matched analysis
- Affiliations
-
- 1Cardiology Unit, Department of Internal Medicine, Faculty of Medicine, Prince of Songkla University, Songkhla, Thailand
- 2Clinical Research Center, Faculty of Medicine, Prince of Songkla University, Songkhla, Thailand
- 3Critical Care Unit, Department of Internal Medicine, Faculty of Medicine, Prince of Songkla University, Songkhla, Thailand
- KMID: 2535303
- DOI: http://doi.org/10.4266/acc.2022.00080
Abstract
- Background
Phlebitis-associated peripheral infusion of intravenous amiodarone is common in clinical practice, with an incidence between 5% and 65%. Several factors, including drug concentration, catheter size, and in-line filter used, are significantly associated with phlebitis occurrence. We performed a retrospective propensity score-matched analysis to find out whether in-line filter will reduce the incidence of amiodarone-induced phlebitis (AIP) in high concentration of amiodarone infusion compared to low concentration without in-line filter.
Methods
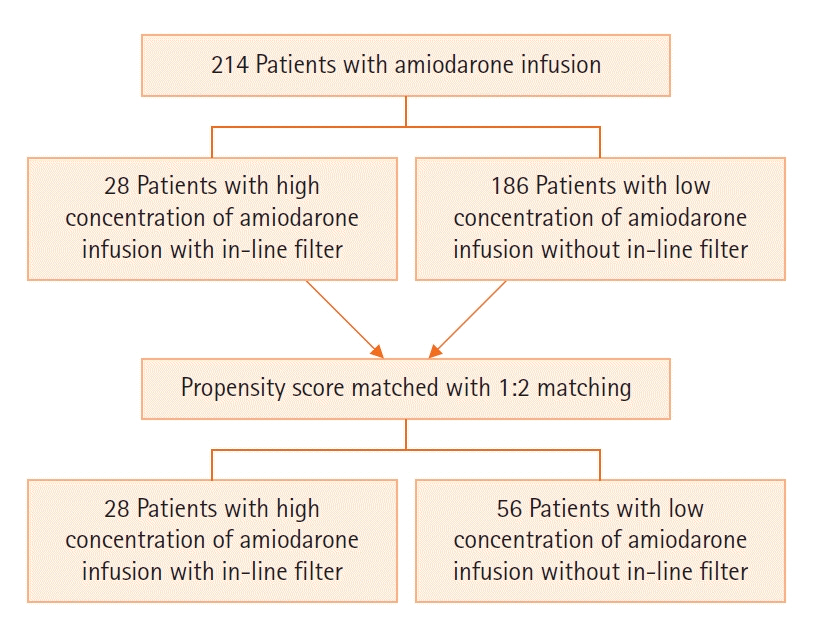
Clinical records of all patients who required intravenous amiodarone infusion for cardiac arrhythmias, between January 2017 to December 2019 were retrieved. The incidence of AIP was recorded and subsequently compared among high concentration (2 mg/ml) with an in-line filter and low concentration (1.5 mg/ml) infusion without an in-line filter after a 1 to 2 propensity score matched.
Results
The data indicated that among the 214 cases of amiodarone infusion collected, 28 cases used an in-line filter with high concentration while 186 cases received a low concentration of amiodarone infusion without an in-line filter. After 1:2 propensity score matching, the incidence of phlebitis in the high concentration with in-line filter group was significantly higher than the low concentration without in-line filter group (28.6% vs. 3.6%, P<0.01).
Conclusions
Despite the usage of in-line filter, the high concentration of amiodarone infusion resulted in a higher incidence of peripheral phlebitis. Central venous catheterization for a high concentration of amiodarone infusion is recommended.
Keyword
Figure
Reference
-
1. Hilleman DE, Hansen JM, Mohiuddin SM. Amiodarone-induced infusion phlebitis. Clin Pharm. 1987; 6:364–367.2. Boyce BA, Yee BH. Incidence and severity of phlebitis in patients receiving peripherally infused amiodarone. Crit Care Nurse. 2012; 32:27–34.3. Dixon HA, Hort AL, Wright CM. Amiodarone-induced phlebitis remains an issue in spite of measures to reduce its occurrence. J Vasc Access. 2019; 20:786–7.4. Hannibal GB. Peripheral phlebitis related to amiodarone infusion. AACN Adv Crit Care. 2016; 27:465–71.5. Norton L, Ottoboni LK, Varady A, Yang-Lu CY, Becker N, Cotter T, et al. Phlebitis in amiodarone administration: incidence, contributing factors, and clinical implications. Am J Crit Care. 2013; 22:498–505.6. Sharifi-Ardani M, Yekefallah L, Asefzadeh S, Nassiri-Asl M. Efficacy of topical chamomile on the incidence of phlebitis due to an amiodarone infusion in coronary care patients: a double-blind, randomized controlled trial. J Integr Med. 2017; 15:373–8.7. Oragano CA, Patton D, Moore Z. Phlebitis in intravenous amiodarone administration: incidence and contributing factors. Crit Care Nurse. 2019; 39:e1–12.8. Hilleman DE, Spinler SA. Conversion of recent-onset atrial fibrillation with intravenous amiodarone: a meta-analysis of randomized controlled trials. Pharmacotherapy. 2002; 22:66–74.9. Infusion Nurses Society. Infusion nursing standards of practice. J Infus Nurs. 2006; 29(Suppl 1):S1–92.10. Murphy K, Murphy J, Fischer-Cartlidge E. Reducing the Incidence of amiodarone-related phlebitis through utilization of evidence-based practice. Worldviews Evid Based Nurs. 2020; 17:385–92.11. Mowry JL, Hartman LS. Intravascular thrombophlebitis related to the peripheral infusion of amiodarone and vancomycin. West J Nurs Res. 2011; 33:457–71.12. Niël-Weise BS, Stijnen T, van den Broek PJ. Should in-line filters be used in peripheral intravenous catheters to prevent infusion-related phlebitis? A systematic review of randomized controlled trials. Anesth Analg. 2010; 110:1624–9.13. Nuttall GA, Houle TT. Liars, damn liars, and propensity scores. Anesthesiology. 2008; 108:3–4.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- In-line Filtration in Parenteral Nutrition
- Factors Contributing to Inferior Vena Cava Filter Removal Failure using Advanced Techniques: A Single-Center Study
- Time course of end-tidal desflurane concentration during delivery and elimination according to the type and location of filters in a semi-closed circuit system
- Correlation between Capillary Blood-spotted Filter Paper Thyrotropin Results and Serum Thyroid Function Tests in Premature Neonates
- Effect of Charcoal Filter on the Emergence from Sevoflurane Anesthesia in a Semi-Closed Rebreathing Circuit