Acute Crit Care.
2022 Aug;37(3):322-331. 10.4266/acc.2022.00367.
Effect of prone positioning on gas exchange according to lung morphology in patients with acute respiratory distress syndrome
- Affiliations
-
- 1Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea
- 2Department of Critical Care Medicine, Seoul National University Hospital, Seoul, Korea
- KMID: 2535295
- DOI: http://doi.org/10.4266/acc.2022.00367
Abstract
- Background
There are limited data on the clinical effects of prone positioning according to lung morphology. We aimed to determine whether the gas exchange response to prone positioning differs according to lung morphology.
Methods
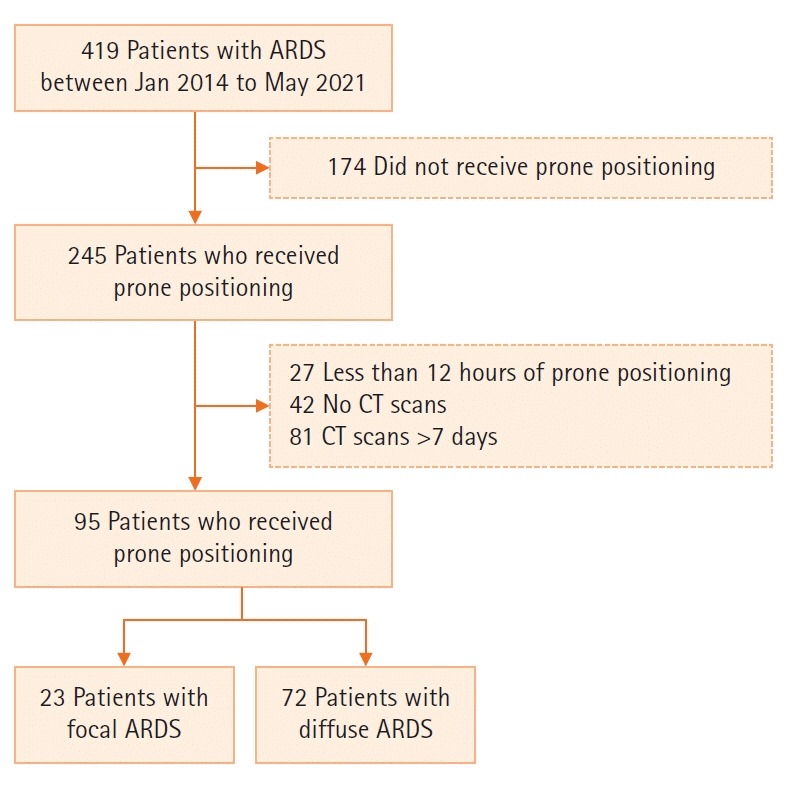
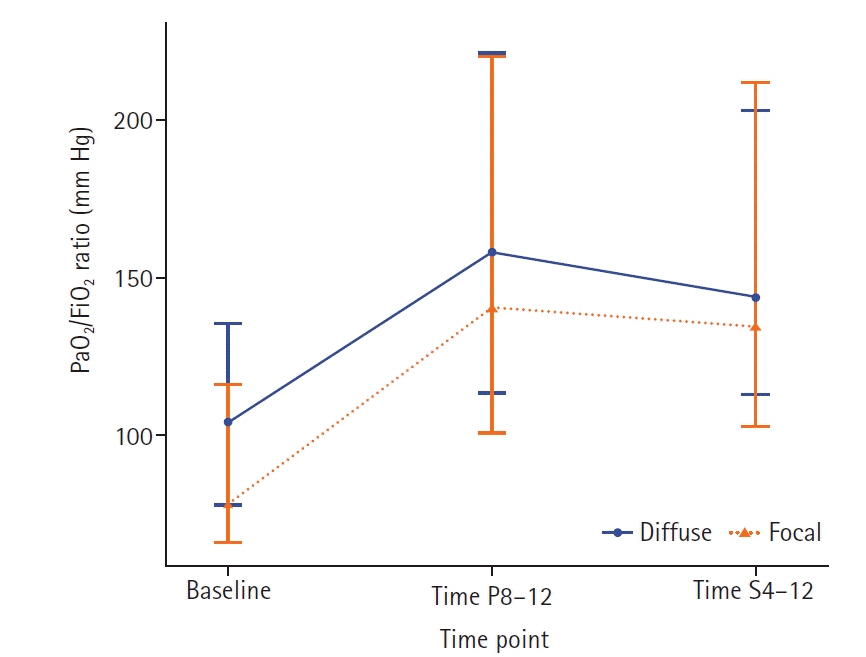
This retrospective study included adult patients with moderate-to-severe acute respiratory distress syndrome (ARDS). The lung morphology of ARDS was assessed by chest computed tomography scan and classified as “diffuse” or “focal.” The primary outcome was change in partial pressure of arterial oxygen to fraction of inspired oxygen (PaO2/FiO2) ratio after the first prone positioning session: first, using the entire cohort, and second, using subgroups of patients with diffuse ARDS matched 2 to 1 with patients with focal ARDS at baseline.
Results
Ninety-five patients were included (focal ARDS group, 23; diffuse ARDS group, 72). Before prone positioning, the focal ARDS group showed worse oxygenation than the diffuse ARDS group (median PaO2/FiO2 ratio, 79.9 mm Hg [interquartile range (IQR)], 67.7–112.6 vs. 104.0 mm Hg [IQR, 77.6–135.7]; P=0.042). During prone positioning, the focal ARDS group showed a greater improvement in the PaO2/FiO2 ratio than the diffuse ARDS group (median, 55.8 mm Hg [IQR, 11.1–109.2] vs. 42.8 mm Hg [IQR, 11.6–83.2]); however, the difference was not significant (P=0.705). Among the PaO2/FiO2-matched cohort, there was no significant difference in change in PaO2/FiO2 ratio after prone positioning between the groups (P=0.904).
Conclusions
In patients with moderate-to-severe ARDS, changes in PaO2/FiO2 ratio after prone positioning did not differ according to lung morphology. Therefore, prone positioning can be considered as soon as indicated, regardless of ARDS lung morphology.
Keyword
Figure
Reference
-
1. Ashbaugh DG, Bigelow DB, Petty TL, Levine BE. Acute respiratory distress in adults. Lancet. 1967; 2:319–23.
Article2. Acute Respiratory Distress Syndrome Network, Brower RG, Matthay MA, Morris A, Schoenfeld D, Thompson BT, et al. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000; 342:1301–8.
Article3. Hager DN, Krishnan JA, Hayden DL, Brower RG; ARDS Clinical Trials Network. Tidal volume reduction in patients with acute lung injury when plateau pressures are not high. Am J Respir Crit Care Med. 2005; 172:1241–5.
Article4. Papazian L, Forel JM, Gacouin A, Penot-Ragon C, Perrin G, Loundou A, et al. Neuromuscular blockers in early acute respiratory distress syndrome. N Engl J Med. 2010; 363:1107–16.
Article5. Briel M, Meade M, Mercat A, Brower RG, Talmor D, Walter SD, et al. Higher vs lower positive end-expiratory pressure in patients with acute lung injury and acute respiratory distress syndrome: systematic review and meta-analysis. JAMA. 2010; 303:865–73.
Article6. Guérin C, Reignier J, Richard JC, Beuret P, Gacouin A, Boulain T, et al. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med. 2013; 368:2159–68.7. Lee HY, Cho J, Kwak N, Choi SM, Lee J, Park YS, et al. Improved oxygenation after prone positioning may be a predictor of survival in patients with acute respiratory distress syndrome. Crit Care Med. 2020; 48:1729–36.
Article8. Scholten EL, Beitler JR, Prisk GK, Malhotra A. Treatment of ARDS with prone positioning. Chest. 2017; 151:215–24.
Article9. Reddy K, Sinha P, O'Kane CM, Gordon AC, Calfee CS, McAuley DF. Subphenotypes in critical care: translation into clinical practice. Lancet Respir Med. 2020; 8:631–43.
Article10. Calfee CS, Delucchi K, Parsons PE, Thompson BT, Ware LB, Matthay MA, et al. Subphenotypes in acute respiratory distress syndrome: latent class analysis of data from two randomised controlled trials. Lancet Respir Med. 2014; 2:611–20.
Article11. Constantin JM, Jabaudon M, Lefrant JY, Jaber S, Quenot JP, Langeron O, et al. Personalised mechanical ventilation tailored to lung morphology versus low positive end-expiratory pressure for patients with acute respiratory distress syndrome in France (the LIVE study): a multicentre, single-blind, randomised controlled trial. Lancet Respir Med. 2019; 7:870–80.12. ARDS Definition Task Force, Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, et al. Acute respiratory distress syndrome: the Berlin Definition. JAMA. 2012; 307:2526–33.13. Hu SL, He HL, Pan C, Liu AR, Liu SQ, Liu L, et al. The effect of prone positioning on mortality in patients with acute respiratory distress syndrome: a meta-analysis of randomized controlled trials. Crit Care. 2014; 18:R109.
Article14. Coppola S, Pozzi T, Gurgitano M, Liguori A, Duka E, Bichi F, et al. Radiological pattern in ARDS patients: partitioned respiratory mechanics, gas exchange and lung recruitability. Ann Intensive Care. 2021; 11:78.
Article15. Costamagna A, Pivetta E, Goffi A, Steinberg I, Arina P, Mazzeo AT, et al. Clinical performance of lung ultrasound in predicting ARDS morphology. Ann Intensive Care. 2021; 11:51.
Article16. Hao D, Low S, Di Fenza R, Shenoy ES, Ananian L, Prout LA, et al. Prone Positioning of Intubated Patients with an Elevated Body-Mass Index. N Engl J Med. 2022; 386:e34.
Article17. Schmidt M, Pham T, Arcadipane A, Agerstrand C, Ohshimo S, Pellegrino V, et al. Mechanical ventilation management during extracorporeal membrane oxygenation for acute respiratory distress syndrome. an international multicenter prospective cohort. Am J Respir Crit Care Med. 2019; 200:1002–12.
Article18. Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol. 1996; 49:1373–9.
Article19. Gattinoni L, Vagginelli F, Carlesso E, Taccone P, Conte V, Chiumello D, et al. Decrease in PaCO2 with prone position is predictive of improved outcome in acute respiratory distress syndrome. Crit Care Med. 2003; 31:2727–33.20. Sjoding MW, Hofer TP, Co I, Courey A, Cooke CR, Iwashyna TJ. Interobserver reliability of the Berlin ARDS definition and strategies to improve the reliability of ARDS diagnosis. Chest. 2018; 153:361–7.
Article21. Bellani G, Laffey JG, Pham T, Fan E, Brochard L, Esteban A, et al. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA. 2016; 315:788–800.
Article22. Rouby JJ, Puybasset L, Nieszkowska A, Lu Q. Acute respiratory distress syndrome: lessons from computed tomography of the whole lung. Crit Care Med. 2003; 31(4 Suppl):S285–95.
Article23. Chiumello D, Langer T, Vecchi V, Luoni S, Colombo A, Brioni M, et al. Low-dose chest computed tomography for quantitative and visual anatomical analysis in patients with acute respiratory distress syndrome. Intensive Care Med. 2014; 40:691–9.
Article24. Simon M, Braune S, Laqmani A, Metschke M, Berliner C, Kalsow M, et al. Value of computed tomography of the chest in subjects with ARDS: a retrospective observational study. Respir Care. 2016; 61:316–23.
Article25. Richter T, Bellani G, Scott Harris R, Vidal Melo MF, Winkler T, Venegas JG, et al. Effect of prone position on regional shunt, aeration, and perfusion in experimental acute lung injury. Am J Respir Crit Care Med. 2005; 172:480–7.
Article26. Petersson J, Glenny RW. Gas exchange and ventilation-perfusion relationships in the lung. Eur Respir J. 2014; 44:1023–41.
Article27. Amato MB, Meade MO, Slutsky AS, Brochard L, Costa EL, Schoenfeld DA, et al. Driving pressure and survival in the acute respiratory distress syndrome. N Engl J Med. 2015; 372:747–55.
Article28. Balzer F, Menk M, Ziegler J, Pille C, Wernecke KD, Spies C, et al. Predictors of survival in critically ill patients with acute respiratory distress syndrome (ARDS): an observational study. BMC Anesthesiol. 2016; 16:108.
Article29. Song M, Liu Y, Lu Z, Luo H, Peng H, Chen P. Prognostic factors for ARDS: clinical, physiological and atypical immunodeficiency. BMC Pulm Med. 2020; 20:102.
Article30. Wu Z, Liu X, Liu J, Zhu F, Liu Y, Liu Y, et al. Correlation between ground-glass opacity on pulmonary CT and the levels of inflammatory cytokines in patients with moderate-to-severe COVID-19 pneumonia. Int J Med Sci. 2021; 18:2394–400.
Article31. Chen YY, Kuo JS, Ruan SY, Chien YC, Ku SC, Yu CJ, et al. Prognostic value of computed tomographic findings in acute respiratory distress syndrome and the response to prone positioning. BMC Pulm Med. 2022; 22:71.
Article32. Scaramuzzo G, Gamberini L, Tonetti T, Zani G, Ottaviani I, Mazzoli CA, et al. Sustained oxygenation improvement after first prone positioning is associated with liberation from mechanical ventilation and mortality in critically ill COVID-19 patients: a cohort study. Ann Intensive Care. 2021; 11:63.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Combined Therapy of Inhaled Nitric Oxide and Prone Positioning Has an Additive Effect on Gas Exchange and Oxygen Transport in Patients with Acute Respiratory Distress Syndrome
- Clinical Meaning of Early Oxygenation Improvement in Severe Acute Respiratory Distress Syndrome under Prolonged Prone Positioning
- Successful Recovery after Drowning by Early Prone Ventilatory Positioning and Use of Nitric Oxide Gas: A Case Report
- Relationship between the Changes of Arterial Blood Gas by Positioning from Prone to Supine and Patients' Survival in ARDS
- Prone Positioning Improves Oxygenation Without Adverse Hemodynamic Effects during Partial Liquid Ventilation in a Canine Model of Acute Lung Injury