J Korean Assoc Oral Maxillofac Surg.
2022 Oct;48(5):297-302. 10.5125/jkaoms.2022.48.5.297.
Sensory change after implant surgery: related factors for recovery
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, Gangnam Severance Hospital, Yonsei University College of Dentistry, Seoul, Korea
- KMID: 2534810
- DOI: http://doi.org/10.5125/jkaoms.2022.48.5.297
Abstract
Objectives
This retrospective study aimed to analyze data on nerve damage in patients who complained of sensory changes after dental implant surgery, the clinical results according to proximity of the implant fixture to the inferior alveolar nerve (IAN) canal, and the factors affecting recovery of sensation.
Materials and Methods
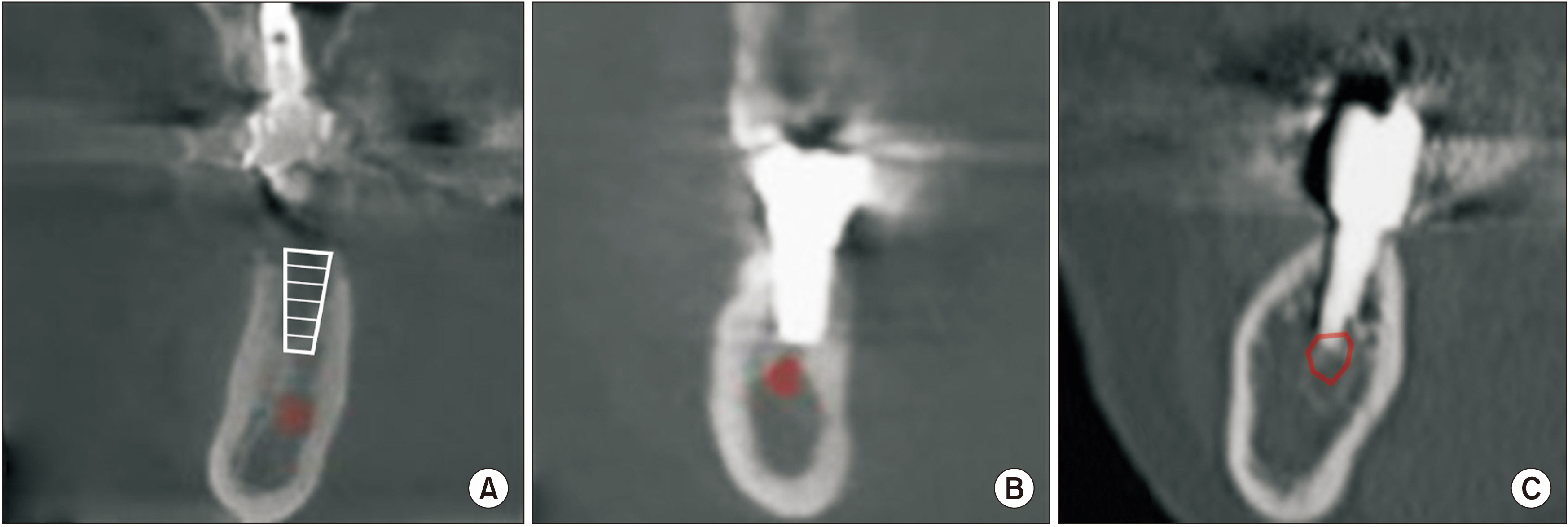
The electronic medical records of 64 patients who had experienced sensory change after implant surgery were reviewed. Patients were classified by sex, age, implant installation sites, recovery rate and the distance between the implant fixture and IAN canal on computed tomography (CT). The distance was classified into Group I (D>2 mm), Group II (2 mm≥D>0 mm), and Group III (D≤0 mm).
Results
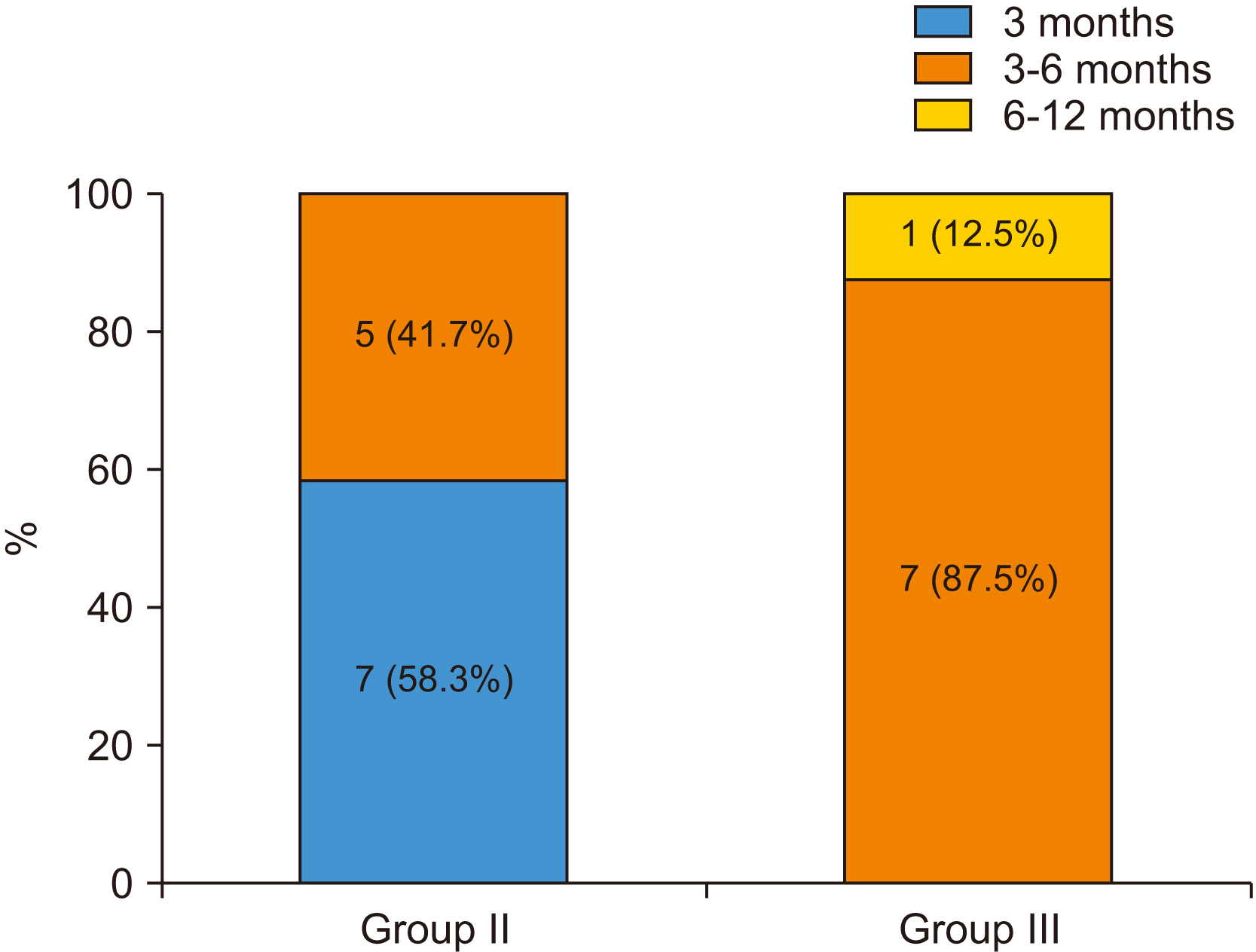
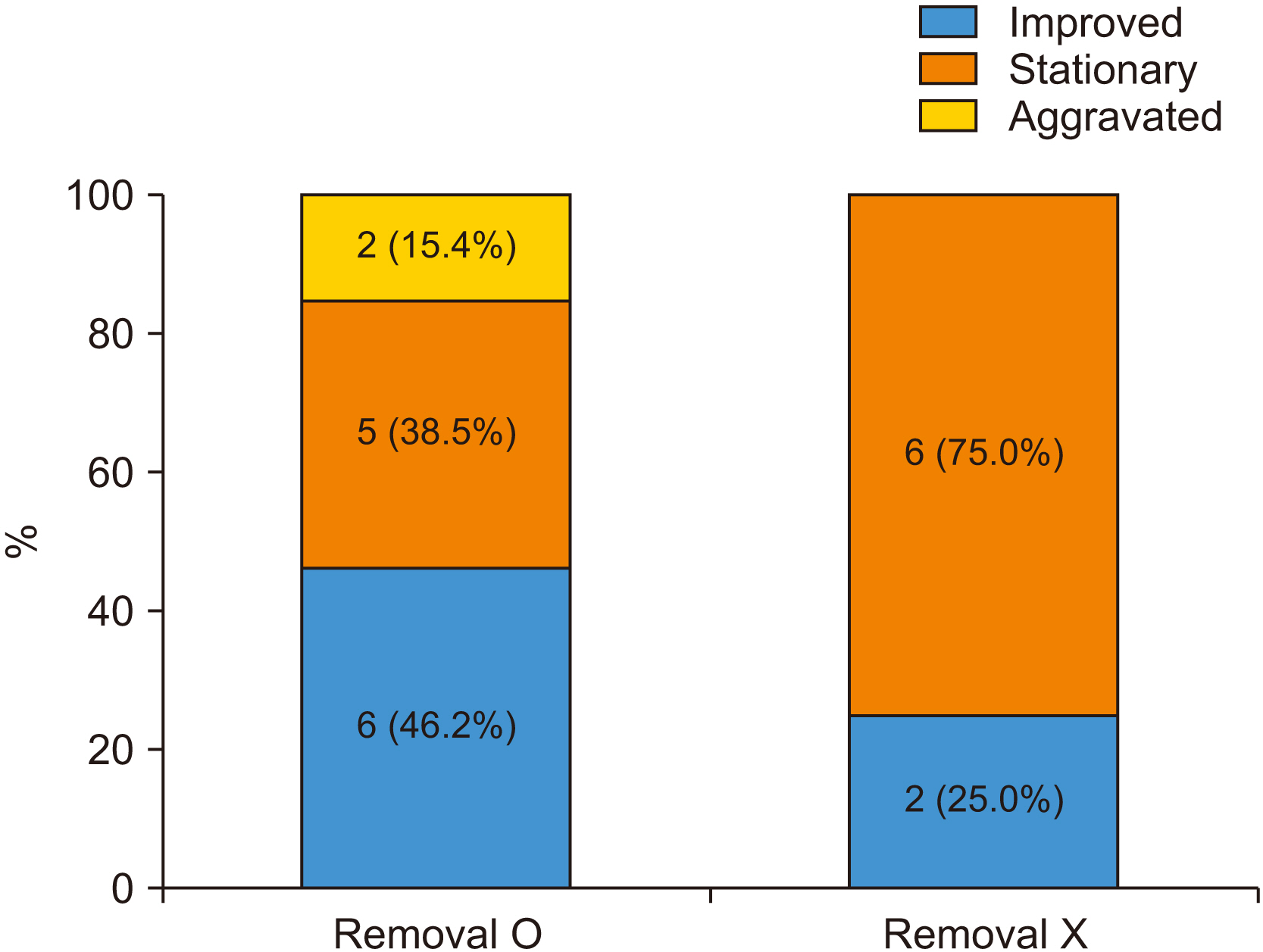
The 64 patients were included and the mean age was 57.3±7.3 years. Among the 36 patients who visited our clinic more than two times, 21 patients (58.3%) reported improvement in sensation, 13 patients (36.1%) had no change in sensation, and 2 patients (5.6%) reported worsening sensation. In Group II, symptom improvement was achieved in all patients regardless of the removal of the implant fixture. In Group III, 8 patients (40.0%) had reported symptom improvement with removal of the implant fixture, and 2 patients (33.3%) of recovered patients showed improvement without removal. Removal of the implant fixture in Group III did not result in any significant difference in recovery (P=0.337), although there was a higher possibility of improvement in sensation in removal cases.
Conclusion
Clinicians first should consider removing the fixture when it directly invades the IAN canal. However, in cases of sensory change after dental implant surgery where the drill or implant fixture did not invade the IAN canal, other indirect factors such as flap elevation and damage due to anesthesia should be considered as causes of sensory change. Removal of the implant should be considered with caution in these situations.
Figure
Reference
-
References
1. Sarikov R, Juodzbalys G. 2014; Inferior alveolar nerve injury after mandibular third molar extraction: a literature review. J Oral Maxillofac Res. 5:e1. https://doi.org/10.5037/jomr.2014.5401. DOI: 10.5037/jomr.2014.5401. PMID: 25635208. PMCID: PMC4306319.
Article2. Juodzbalys G, Wang HL, Sabalys G, Sidlauskas A, Galindo-Moreno P. 2013; Inferior alveolar nerve injury associated with implant surgery. Clin Oral Implants Res. 24:183–90. https://doi.org/10.1111/j.1600-0501.2011.02314.x. DOI: 10.1111/j.1600-0501.2011.02314.x. PMID: 22092662.
Article3. López-López J, Estrugo-Devesa A, Jané-Salas E, Segura-Egea JJ. 2012; Inferior alveolar nerve injury resulting from overextension of an endodontic sealer: non-surgical management using the GABA analogue pregabalin. Int Endod J. 45:98–104. https://doi.org/10.1111/j.1365-2591.2011.01939.x. DOI: 10.1111/j.1365-2591.2011.01939.x. PMID: 21883296.
Article4. Pogrel MA. 2012; Permanent nerve damage from inferior alveolar nerve blocks: a current update. J Calif Dent Assoc. 40:795–7. PMID: 23316560.5. Phillips C, Essick G. 2011; Inferior alveolar nerve injury following orthognathic surgery: a review of assessment issues. J Oral Rehabil. 38:547–54. https://doi.org/10.1111/j.1365-2842.2010.02176.x. DOI: 10.1111/j.1365-2842.2010.02176.x. PMID: 21058973. PMCID: PMC3094736.
Article6. Yekta SS, Koch F, Grosjean MB, Esteves-Oliveira M, Stein JM, Ghassemi A, et al. 2010; Analysis of trigeminal nerve disorders after oral and maxillofacial intervention. Head Face Med. 6:24. https://doi.org/10.1186/1746-160X-6-24. DOI: 10.1186/1746-160X-6-24. PMID: 20977760. PMCID: PMC2984556.
Article7. Pigg M. 2011; Chronic intraoral pain--assessment of diagnostic methods and prognosis. Swed Dent J Suppl. (220):7–91. PMID: 22338784.8. Choi YC, Kwon JS, Kim ST, Ahn HJ. 2009; Analysis of patients with dysesthesia after mandibular nerve injury. J Oral Med Pain. 34:379–85.9. Leung YY, Fung PP, Cheung LK. 2012; Treatment modalities of neurosensory deficit after lower third molar surgery: a systematic review. J Oral Maxillofac Surg. 70:768–78. https://doi.org/10.1016/j.joms.2011.08.032. DOI: 10.1016/j.joms.2011.08.032. PMID: 22177820.
Article10. Kim JW, Cha IH, Kim SJ, Kim MR. 2012; Which risk factors are associated with neurosensory deficits of inferior alveolar nerve after mandibular third molar extraction? J Oral Maxillofac Surg. 70:2508–14. https://doi.org/10.1016/j.joms.2012.06.004. DOI: 10.1016/j.joms.2012.06.004. PMID: 22901857.
Article11. Kjølle GK, Bjørnland T. 2013; Low risk of neurosensory dysfunction after mandibular third molar surgery in patients less than 30 years of age. A prospective study following removal of 1220 mandibular third molars. Oral Surg Oral Med Oral Pathol Oral Radiol. 116:411–7. https://doi.org/10.1016/j.oooo.2013.06.024. DOI: 10.1016/j.oooo.2013.06.024. PMID: 24035108.
Article12. Burstein J, Mastin C, Le B. 2008; Avoiding injury to the inferior alveolar nerve by routine use of intraoperative radiographs during implant placement. J Oral Implantol. 34:34–8. https://doi.org/10.1563/1548-1336(2008)34[34:AITTIA]2.0.CO;2. DOI: 10.1563/1548-1336(2008)34[34:AITTIA]2.0.CO;2. PMID: 18390241.
Article13. Steinberg MJ, Kelly PD. 2015; Implant-related nerve injuries. Dent Clin North Am. 59:357–73. https://doi.org/10.1016/j.cden. 2014.10.003. DOI: 10.1016/j.cden.2014.10.003. PMID: 25835799.
Article14. Greenstein G, Carpentieri JR, Cavallaro J. 2015; Nerve damage related to implant dentistry: incidence, diagnosis, and management. Compend Contin Educ Dent. 36:652–9. quiz 660. PMID: 26448148.15. Velasco-Torres M, Padial-Molina M, Avila-Ortiz G, García-Delgado R, Catena A, Galindo-Moreno P. 2017; Inferior alveolar nerve trajectory, mental foramen location and incidence of mental nerve anterior loop. Med Oral Patol Oral Cir Bucal. 22:e630–5. https://doi.org/10.4317/medoral.21905. DOI: 10.4317/medoral.21905. PMID: 28809376. PMCID: PMC5694187.
Article16. Jang SI, Paeng JY. 2018; Non-surgical management of inferior alveolar nerve damage after implant installation. J Dent Implant Res. 37:18–22. https://doi.org/10.54527/jdir.2018.37.1.18.
Article17. Juodzbalys G, Wang HL, Sabalys G. 2011; Injury of the inferior alveolar nerve during implant placement: a literature review. J Oral Maxillofac Res. 2:e1. https://doi.org/10.5037/jomr.2011.2101. DOI: 10.5037/jomr.2011.2101. PMID: 24421983. PMCID: PMC3886063.
Article18. Greenstein G, Tarnow D. 2006; The mental foramen and nerve: clinical and anatomical factors related to dental implant placement: a literature review. J Periodontol. 77:1933–43. https://doi.org/10.1902/jop.2006.060197. DOI: 10.1902/jop.2006.060197. PMID: 17209776.
Article19. Voon YS, Patil PG. 2018; Safe zone in anterior mandible related to the genial tubercle for implant osteotomy in a Chinese-Malaysian population: a CBCT study. J Prosthet Dent. 119:568–73. https://doi.org/10.1016/j.prosdent.2017.05.011. DOI: 10.1016/j.prosdent.2017.05.011. PMID: 28838820.
Article20. Helmi MF, Huang H, Goodson JM, Hasturk H, Tavares M, Natto ZS. 2019; Prevalence of periodontitis and alveolar bone loss in a patient population at Harvard School of Dental Medicine. BMC Oral Health. 19:254. https://doi.org/10.1186/s12903-019-0925-z. DOI: 10.1186/s12903-019-0925-z. PMID: 31752793. PMCID: PMC6873420.
Article21. Khawaja N, Renton T. 2009; Case studies on implant removal influencing the resolution of inferior alveolar nerve injury. Br Dent J. 206:365–70. https://doi.org/10.1038/sj.bdj.2009.258. DOI: 10.1038/sj.bdj.2009.258. PMID: 19357667.
Article22. Du Toit J, Gluckman H, Gamil R, Renton T. 2015; Implant injury case series and review of the literature part 1: inferior alveolar nerve injury. J Oral Implantol. 41:e144–51. https://doi.org/10.1563/aaid-joi-D-14-00022. DOI: 10.1563/AAID-JOI-D-14-00022. PMID: 24945089.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The prevalence of sensory disturbance after implant surgery - retrospective survey of implant practitioners
- Sensory change and recovery of infraorbital area after zygomaticomaxillary and orbital floor fractures
- Clinical Recovery after Surgical Treatment of Lumbar HIVD
- Tactile Sensation Recovery after Parotidectomy
- Clinical outcome of conservative treatment of injured inferior alveolar nerve during dental implant placement