J Korean Med Sci.
2022 Oct;37(42):e303. 10.3346/jkms.2022.37.e303.
SARS-CoV-2-Naïve Korean Children and Adolescents Hospitalized With COVID-19 in 2021
- Affiliations
-
- 1Department of Pediatrics, National Medical Center, Seoul, Korea
- 2Department of Pediatrics, Pusan National University Hospital, Busan, Korea
- 3Department of Pediatrics, Jeju National University College of Medicine, Jeju, Korea
- 4Department of Pediatrics, Inha University College of Medicine, Incheon, Korea
- 5Department of Pediatrics, Chungbuk National University Hospital, Chungbuk National University College of Medicine, Cheongju, Korea
- 6Department of Pediatrics, Eulji University School of Medicine, Nowon Eulji University Hospital, Seoul, Korea
- 7Department of Pediatrics, Seoul National University Bundang Hospital, Seongnam, Korea
- 8Department of Pediatrics, Seoul National University College of Medicine, Seoul, Korea
- 9Department of Pediatrics, Konkuk University Medical Center, Seoul, Korea
- 10Department of Pediatrics, Seoul National University Children’s Hospital, Seoul, Korea
- KMID: 2534756
- DOI: http://doi.org/10.3346/jkms.2022.37.e303
Abstract
- Background
The risk of severe outcomes with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) delta variant remains low in children and adolescents, but less is known about its effect on the SARS-CoV-2-naïve population. This study evaluated clinical manifestations and risk factors for moderate-to-critical coronavirus disease 2019 (COVID-19) in mostly SARS-CoV-2-naïve children and adolescents in 2021.
Methods
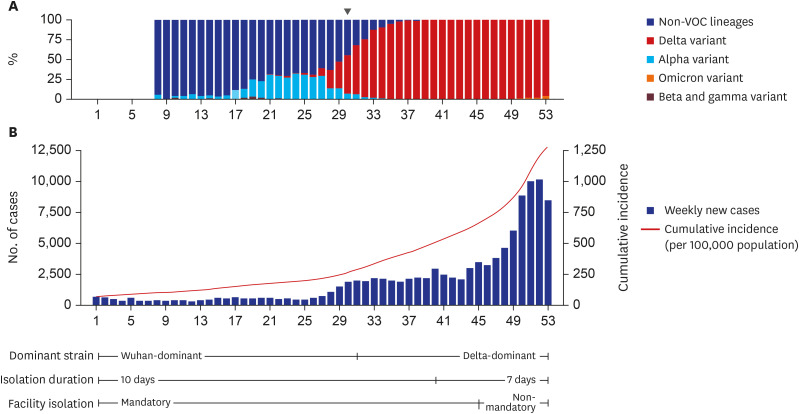
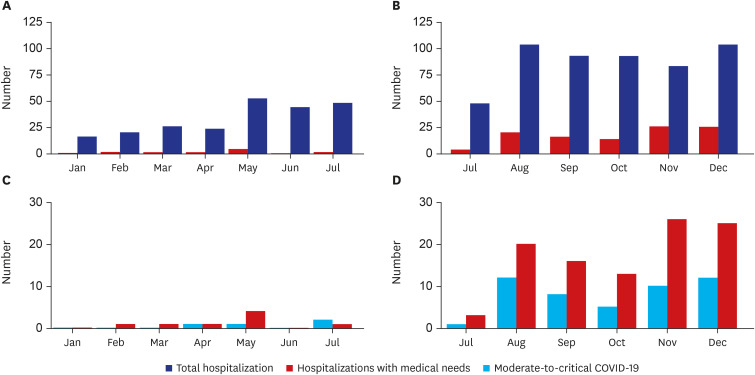
This multicenter retrospective study included patients aged 0–18 years who were hospitalized with COVID-19 at 8 referring hospitals in South Korea during the predeltapredominant and delta-predominant periods in 2021. Each case was labeled as either hospitalization with medical needs or for isolation. Severity was categorized as mild, moderate, severe, or critical with regard to pneumonia presence and illness severity.
Results
Among 753 cases, most (99.5%) had no prior history of COVID-19 or vaccination against COVID-19. The proportions of hospitalization with medical needs (3.5% vs. 19.7%), moderate illness (0.9% vs. 4.0%), and severe/critical illness (0.8% vs. 5.3%) increased during delta predominance. The risk of moderate-to-critical COVID-19 among hospitalizations with medical needs was higher among patients aged 12–18 years (adjusted odds ratio [aOR], 4.1; 95% confidence interval [CI], 1.5–11.8) and with obesity (aOR, 6.9; 95% CI, 2.4–19.6) but not among patients infected during delta predominance. However, children with obesity experienced more severe COVID-19 during delta predominance (aOR, 6.1; 95% CI, 1.2–29.6).
Conclusion
Despite its similar severity among most SARS-CoV-2-naïve children and adolescents, the delta variant may affect COVID-19 severity in those with high-risk underlying medical conditions. Underlying conditions, particularly obesity, may cause severe COVID-19 in children and adolescents, warranting strong consideration for vaccinating high-risk children.
Keyword
Figure
Cited by 1 articles
-
Clinical characteristics and outcomes of COVID-19 in children and adolescents with diabetes in Daegu, South Korea
Na-Won Lee, You-Min Kim, Young-Hwan Kim, Seok-Jin Kang, Kyung-Mi Jang, Hae-Sook Kim, Jung-Eun Moon, Jin-Kyung Kim
Ann Pediatr Endocrinol Metab. 2024;29(3):167-173. doi: 10.6065/apem.2346124.062.
Reference
-
1. Korea Disease Control and Prevention Agency. Korea COVID-19 update (17 July 2021). Updated 2021. Accessed April 5, 2022. https://www.kdca.go.kr/board/board.es?mid=a20501020000&bid=0015 .2. Korea Disease Control and Prevention Agency. Korea COVID-19 update (16 August 2021). Updated 2021. Accessed July 28, 2022. https://www.kdca.go.kr/board/board.es?mid=a20501020000&bid=0015 .3. Kim IH, Park AK, Lee H, Kim HM, Kim J, Kim JA, et al. Status and characteristics of the SARS-CoV-2 variant outbreak in the Republic of Korea in January 2021. Public Health Wkly Rep. 2022; 15(8):505–510.4. Lee H, Choi S, Park JY, Jo DS, Choi UY, Lee H, et al. Analysis of critical COVID-19 cases among children in Korea. J Korean Med Sci. 2022; 37(1):e13. PMID: 34981683.
Article5. Forrest CB, Burrows EK, Mejias A, Razzaghi H, Christakis D, Jhaveri R, et al. Severity of acute COVID-19 in children <18 years old March 2020 to December 2021. Pediatrics. 2022; 149(4):e2021055765. PMID: 35322270.
Article6. Bundle N, Dave N, Pharris A, Spiteri G, Deogan C, Suk JE. Study group members. COVID-19 trends and severity among symptomatic children aged 0–17 years in 10 European Union countries, 3 August 2020 to 3 October 2021. Euro Surveill. 2021; 26(50):2101098.
Article7. Thelwall S, Aiano F, Harman K, Dabrera G, Ladhani SN. Risk of hospitalisation and death in children with SARS-CoV-2 delta (B.1.612.2) infection. Lancet Child Adolesc Health. 2022; 6(5):e16–e17. PMID: 35364023.8. Delahoy MJ, Ujamaa D, Whitaker M, O’Halloran A, Anglin O, Burns E, et al. Hospitalizations associated with COVID-19 among children and adolescents - COVID-NET, 14 states, March 1, 2020-August 14, 2021. MMWR Morb Mortal Wkly Rep. 2021; 70(36):1255–1260. PMID: 34499627.9. Singanayagam A, Hakki S, Dunning J, Madon KJ, Crone MA, Koycheva A, et al. Community transmission and viral load kinetics of the SARS-CoV-2 delta (B.1.617.2) variant in vaccinated and unvaccinated individuals in the UK: a prospective, longitudinal, cohort study. Lancet Infect Dis. 2022; 22(2):183–195. PMID: 34756186.10. Dagan N, Barda N, Kepten E, Miron O, Perchik S, Katz MA, et al. BNT162b2 mRNA COVID-19 vaccine in a nationwide mass vaccination setting. N Engl J Med. 2021; 384(15):1412–1423. PMID: 33626250.11. Chung H, He S, Nasreen S, Sundaram ME, Buchan SA, Wilson SE, et al. Effectiveness of BNT162b2 and mRNA-1273 covid-19 vaccines against symptomatic SARS-CoV-2 infection and severe covid-19 outcomes in Ontario, Canada: test negative design study. BMJ. 2021; 374:n1943. PMID: 34417165.12. Kim IH, Park AK, Lee H, Kim J, Kim DH, Kim JA, et al. July 2021 status and characteristics of the COVID-19 variant virus outbreak in the Republic of Korea. Public Health Wkly Rep. 2021; 14(36):3388–3396.13. Dong Y, Mo X, Hu Y, Qi X, Jiang F, Jiang Z, et al. Epidemiology of COVID-19 among children in China. Pediatrics. 2020; 145(6):e20200702. PMID: 32179660.14. Bialek S, Gierke R, Hughes M, McNamara LA, Pilishvili T, Skoff T, et al. Coronavirus disease 2019 in children - United States, February 12-April 2, 2020. MMWR Morb Mortal Wkly Rep. 2020; 69(14):422–426. PMID: 32271728.15. Mehta NS, Mytton OT, Mullins EW, Fowler TA, Falconer CL, Murphy OB, et al. SARS-CoV-2 (COVID-19): what do we know about children? A systematic review. Clin Infect Dis. 2020; 71(9):2469–2479. PMID: 32392337.
Article16. de Souza TH, Nadal JA, Nogueira RJ, Pereira RM, Brandão MB. Clinical manifestations of children with COVID-19: a systematic review. Pediatr Pulmonol. 2020; 55(8):1892–1899. PMID: 32492251.17. Yasuhara J, Kuno T, Takagi H, Sumitomo N. Clinical characteristics of COVID-19 in children: a systematic review. Pediatr Pulmonol. 2020; 55(10):2565–2575. PMID: 32725955.18. Brookman S, Cook J, Zucherman M, Broughton S, Harman K, Gupta A. Effect of the new SARS-CoV-2 variant B.1.1.7 on children and young people. Lancet Child Adolesc Health. 2021; 5(4):e9–10. PMID: 33581054.19. Somekh I, Stein M, Karakis I, Simões EA, Somekh E. Characteristics of SARS-CoV-2 infections in Israeli children during the circulation of different SARS-CoV-2 variants. JAMA Netw Open. 2021; 4(9):e2124343. PMID: 34491353.20. Murillo-Zamora E, Trujillo X, Huerta M, Ríos-Silva M, Baltazar-Rodríguez LM, Guzmán-Esquivel J, et al. Decreased risk of COVID-19 pneumonia in children and adolescents during the Delta variant emergence. Public Health. 2022; 204:9–11. PMID: 35085915.21. Shoji K, Akiyama T, Tsuzuki S, Matsunaga N, Asai Y, Suzuki S, et al. Comparison of the clinical characteristics and outcomes of COVID-19 in children before and after the emergence of Delta variant of concern in Japan. J Infect Chemother. 2022; 28(4):591–594. PMID: 35074258.
Article22. Roser M, Ritchie H, Ortiz-Ospina E, Hasell J. Coronavirus Disease (COVID-19)–Statistics and Research-Our World in Data. Oxford, United Kingdom: University of Oxford;2020.23. Ryu BH, Hong SI, Lim SJ, Cho Y, Hong KW, Bae IG, et al. Features of COVID-19 among children and adolescents without risk factors before and after the delta variant outbreak in South Korea. Pediatr Infect Dis J. 2022; 41(1):e34–e35. PMID: 34773397.24. Graff K, Smith C, Silveira L, Jung S, Curran-Hays S, Jarjour J, et al. Risk factors for severe COVID-19 in children. Pediatr Infect Dis J. 2021; 40(4):e137–e145. PMID: 33538539.25. Kompaniyets L, Agathis NT, Nelson JM, Preston LE, Ko JY, Belay B, et al. Underlying medical conditions associated with severe COVID-19 illness among children. JAMA Netw Open. 2021; 4(6):e2111182. PMID: 34097050.26. Campbell JI, Dubois MM, Savage TJ, Hood-Pishchany MI, Sharma TS, Petty CR, et al. Comorbidities associated with hospitalization and progression among adolescents with symptomatic coronavirus disease 2019. J Pediatr. 2022; 245:102–110.e2. PMID: 35240138.27. Ward JL, Harwood R, Smith C, Kenny S, Clark M, Davis PJ, et al. Risk factors for PICU admission and death among children and young people hospitalized with COVID-19 and PIMS-TS in England during the first pandemic year. Nat Med. 2022; 28(1):193–200. PMID: 34931076.28. Choi JH, Choi SH, Yun KW. Risk factors for severe COVID-19 in children: a systematic review and meta-analysis. J Korean Med Sci. 2022; 37(5):e35. PMID: 35132841.29. Harwood R, Yan H, Talawila Da Camara N, Smith C, Ward J, Tudur-Smith C, et al. Which children and young people are at higher risk of severe disease and death after hospitalisation with SARS-CoV-2 infection in children and young people: A systematic review and individual patient meta-analysis. EClinicalMedicine. 2022; 44:101287. PMID: 35169689.30. Coleman BL, Fadel SA, Fitzpatrick T, Thomas SM. Risk factors for serious outcomes associated with influenza illness in high- versus low- and middle-income countries: Systematic literature review and meta-analysis. Influenza Other Respi Viruses. 2018; 12(1):22–29.31. Saatci D, Ranger TA, Garriga C, Clift AK, Zaccardi F, Tan PS, et al. Association between race and COVID-19 outcomes among 2.6 million children in England. JAMA Pediatr. 2021; 175(9):928–938. PMID: 34152371.32. Bourgeois FT, Gutiérrez-Sacristán A, Keller MS, Liu M, Hong C, Bonzel CL, et al. International analysis of electronic health records of children and youth hospitalized with COVID-19 infection in 6 countries. JAMA Netw Open. 2021; 4(6):e2112596. PMID: 34115127.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- COVID-19 and diabetes in children
- COVID-19 and Breastfeeding
- Clinical implications of coronavirus disease 2019 in neonates
- SARS-CoV-2-Specific T Cell Responses in Patients with COVID-19 and Unexposed Individuals
- Epidemiology, Virology, and Clinical Features of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2; Coronavirus Disease-19)