Brain Tumor Res Treat.
2022 Oct;10(4):226-236. 10.14791/btrt.2022.0014.
Surgical Outcomes of Endoscopic Endonasal Versus Transcranial Resections of Adult Craniopharyngioma: A Meta-Analysis
- Affiliations
-
- 1Medical College, Aga Khan University, Karachi, Pakistan
- 2Section of Neurosurgery, Aga Khan University, Karachi, Pakistan
- KMID: 2534721
- DOI: http://doi.org/10.14791/btrt.2022.0014
Abstract
- Background
The endoscopic endonasal approach (EEA) has been gaining popularity for resection of adult craniopharyngiomas. However, the safety and effectiveness of the procedure in comparison to the traditional transcranial approach (TCA) remains unestablished as previous reviews are outdated.
Methods
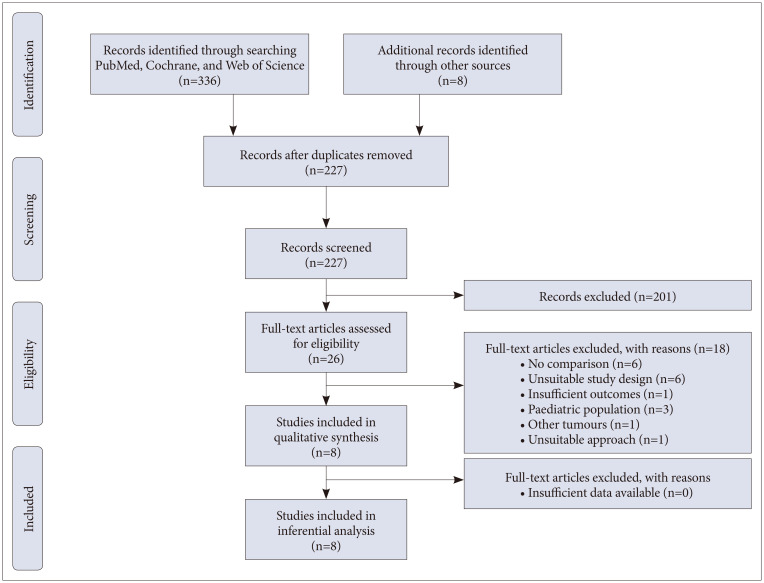
A literature search without language restriction was conducted in PubMed, Cochrane database, and Web of Science from conception to July 9, 2021. Cohort studies and case series that compared EEA with TCA and assessed postoperative complications, recurrence, and 30-day mortality were included. Articles, where data for adult populations could not be extracted or calculated, were excluded. Article selection and data extraction in a predesigned data extraction form were conducted in duplicate. Pooled participant data were included in a random-effects model.
Results
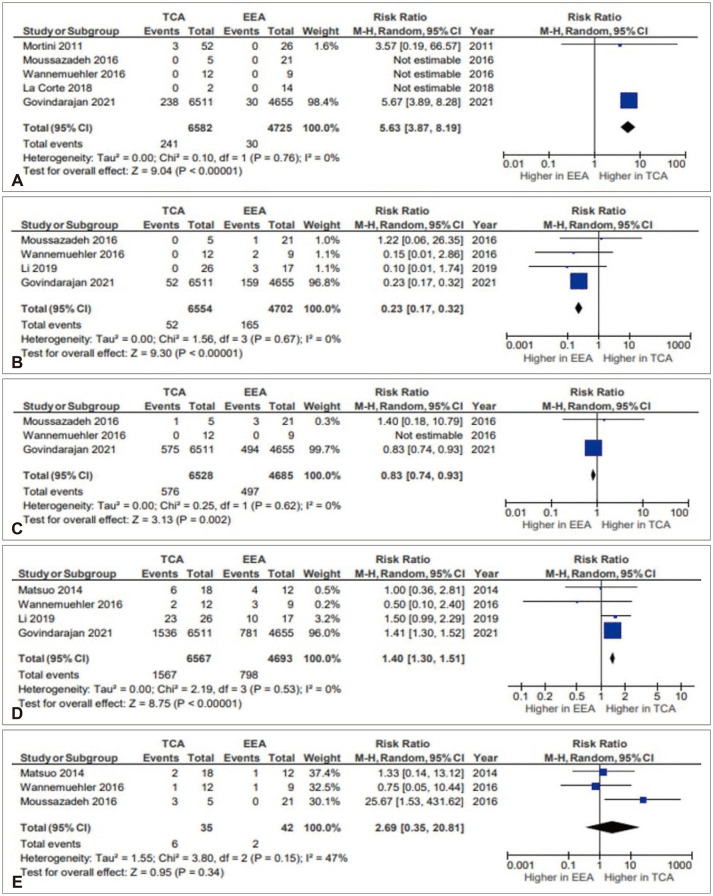
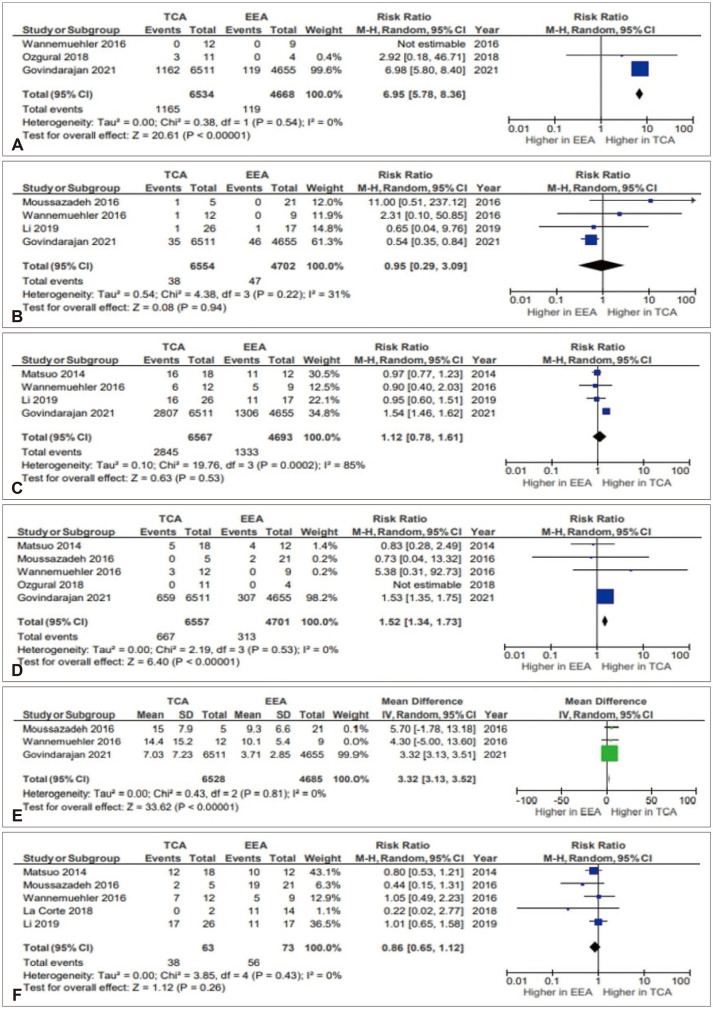
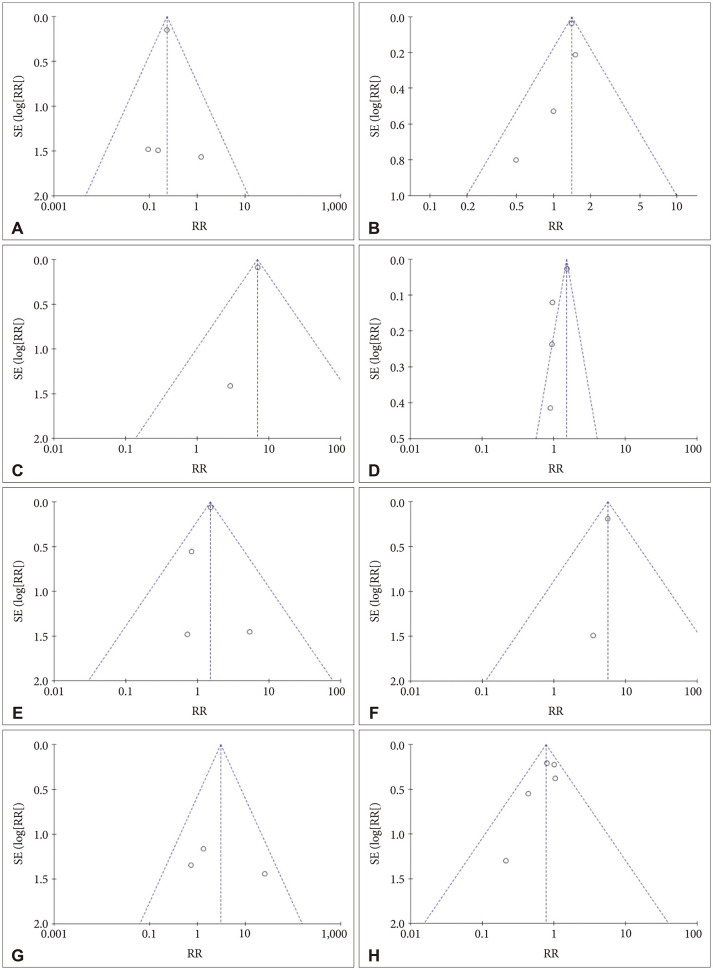
The search yielded 227 articles, from which eight cohort studies containing 11,395 patients were included (EEA: 6,614 patients, TCA: 4,781 patients). Six studies were good quality and two were fair quality according to the Newcastle Ottawa Scale. There were significantly higher rates of cerebrospinal fluid leak (risk ratio [RR]=0.23, 95% confidence interval [CI] 0.17–0.32, p<0.00001, I2 =0%) and lower rates of postoperative hypopituitarism (RR=1.40, 95% CI 1.30–1.51, p<0.00001, I2 =0%), hydrocephalus (RR=6.95, 95% CI 5.78–8.36, p<0.00001, I2 =0%), visual impairment (RR=1.52, 95% CI 1.34–1.73, p<0.00001, I2 =0%), and 30-day mortality (RR=5.63, 95% CI 3.87–8.19, p<0.00001, I2 =0%) after EEA. Non-significant lower rates of postoperative diabetes insipidus (RR=1.12, 95% CI 0.78–1.61, p=0.53, I2 =85%) and recurrence of tumor (RR=2.69, 95% CI 0.35–20.81, p=0.34, I2 =47%) were seen after EEA.
Conclusion
EEA may be associated with reduced postoperative hypopituitarism, hydrocephalus, visual impairment, and 30-day mortality and higher rates of cerebrospinal fluid leak. These findings do not account for differences in tumor size and extension between the EEA and TCA cohorts. Further research on patients with comparable tumor characteristics is required to fully assess outcomes.
Figure
Reference
-
1. Karavitaki N, Cudlip S, Adams CB, Wass JA. Craniopharyngiomas. Endocr Rev. 2006; 27:371–397. PMID: 16543382.
Article2. Li X, Wu W, Miao Q, He M, Zhang S, Zhang Z, et al. Endocrine and metabolic outcomes after transcranial and endoscopic endonasal approaches for primary resection of craniopharyngiomas. World Neurosurg. 2019; 121:e8–e14. PMID: 30266691.
Article3. Fernandez-Miranda JC, Gardner PA, Snyderman CH, Devaney KO, Strojan P, Suárez C, et al. Craniopharyngioma: a pathologic, clinical, and surgical review. Head Neck. 2012; 34:1036–1044. PMID: 21584897.
Article4. Kassam AB, Gardner PA, Snyderman CH, Carrau RL, Mintz AH, Prevedello DM. Expanded endonasal approach, a fully endoscopic transnasal approach for the resection of midline suprasellar craniopharyngiomas: a new classification based on the infundibulum. J Neurosurg. 2008; 108:715–728. PMID: 18377251.
Article5. Campbell PG, McGettigan B, Luginbuhl A, Yadla S, Rosen M, Evans JJ. Endocrinological and ophthalmological consequences of an initial endonasal endoscopic approach for resection of craniopharyngiomas. Neurosurg Focus. 2010; 28:E8.
Article6. Liu JK, Cole CD, Kestle JR, Brockmeyer DL, Walker ML. Cranial base strategies for resection of craniopharyngioma in children. Neurosurg Focus. 2005; 18:E9.
Article7. Fahlbusch R, Honegger J, Paulus W, Huk W, Buchfelder M. Surgical treatment of craniopharyngiomas: experience with 168 patients. J Neurosurg. 1999; 90:237–250. PMID: 9950494.
Article8. Komotar RJ, Starke RM, Raper DM, Anand VK, Schwartz TH. Endoscopic endonasal compared with microscopic transsphenoidal and open transcranial resection of craniopharyngiomas. World Neurosurg. 2012; 77:329–341. PMID: 22501020.
Article9. Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015; 4:1. PMID: 25554246.
Article10. Higgins JP, Savović J, Page MJ, Elbers RG, Sterne JA. Assessing risk of bias in a randomized trial. Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editors. Cochrane handbook for systematic reviews of interventions. 2nd ed. Hoboken, NJ: Wiley-Blackwell;2019. p. 205–228.11. McGuinness LA, Higgins JPT. Risk-of-bias VISualization (robvis): an R package and Shiny web app for visualizing risk-of-bias assessments. Res Synth Methods. 2021; 12:55–61. PMID: 32336025.
Article12. Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa: Ottawa Hospital Research Institute;2011. p. 1–12.13. The Cochrane Collaboration. Review Manager (RevMan) [Computer program] Version 5.4. London: The Cochrane Collaboration;2020.14. Mortini P, Losa M, Pozzobon G, Barzaghi R, Riva M, Acerno S, et al. Neurosurgical treatment of craniopharyngioma in adults and children: early and long-term results in a large case series. J Neurosurg. 2011; 114:1350–1359. PMID: 21214336.
Article15. Matsuo T, Kamada K, Izumo T, Nagata I. Indication and limitations of endoscopic extended transsphenoidal surgery for craniopharyngioma. Neurol Med Chir (Tokyo). 2014; 54:974–982.
Article16. La Corte E, Younus I, Pivari F, Selimi A, Ottenhausen M, Forbes JA, et al. BRAF V600E mutant papillary craniopharyngiomas: a single-institutional case series. Pituitary. 2018; 21:571–583. PMID: 30187175.
Article17. Govindarajan V, Luther EM, Morell AA, Burks JD, King H, Eichberg DG, et al. Perioperative complications in endoscopic endonasal versus transcranial resections of adult craniopharyngiomas. World Neurosurg. 2021; 152:e729–e737. PMID: 34153480.18. Ozgural O, Kahilogullari G, Dogan I, Al-Beyati ESM, Bozkurt M, Tetik B, et al. Single-center surgical experience of the treatment of craniopharyngiomas with emphasis on the operative approach: endoscopic endonasal and open microscopic transcranial approaches. J Craniofac Surg. 2018; 29:e572–e578. PMID: 29863551.19. Wannemuehler TJ, Rubel KE, Hendricks BK, Ting JY, Payner TD, Shah MV, et al. Outcomes in transcranial microsurgery versus extended endoscopic endonasal approach for primary resection of adult craniopharyngiomas. Neurosurg Focus. 2016; 41:E6.
Article20. Moussazadeh N, Prabhu V, Bander ED, Cusic RC, Tsiouris AJ, Anand VK, et al. Endoscopic endonasal versus open transcranial resection of craniopharyngiomas: a case-matched single-institution analysis. Neurosurg Focus. 2016; 41:E7.
Article21. Dasenbrock HH, Liu KX, Devine CA, Chavakula V, Smith TR, Gormley WB, et al. Length of hospital stay after craniotomy for tumor: a national surgical quality improvement program analysis. Neurosurg Focus. 2015; 39:E12.
Article22. Fraser S, Gardner PA, Koutourousiou M, Kubik M, Fernandez-Miranda JC, Snyderman CH, et al. Risk factors associated with postoperative cerebrospinal fluid leak after endoscopic endonasal skull base surgery. J Neurosurg. 2018; 128:1066–1071. PMID: 28598276.
Article23. Qiao N. Endocrine outcomes of endoscopic versus transcranial resection of craniopharyngiomas: a system review and meta-analysis. Clin Neurol Neurosurg. 2018; 169:107–115. PMID: 29655011.24. Cossu G, Jouanneau E, Cavallo LM, Elbabaa SK, Giammattei L, Starnoni D, et al. Surgical management of craniopharyngiomas in adult patients: a systematic review and consensus statement on behalf of the EANS skull base section. Acta Neurochir (Wien). 2020; 162:1159–1177. PMID: 32112169.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of an Orbital Abscess Managed by Endonasal Endoscopic Surgery
- Papillary Craniopharyngiona: A report of two cases
- Endoscopic Endonasal Skull Base Repair with Nasoseptal Flap
- Success Rate of Endonasal Dacryocystorhinostomy Based on the Location of the Lacrimal Sac
- Endoscopic Endonasal Transsphenoidal Skull Base Surgery