J Yeungnam Med Sci.
2022 Oct;39(4):332-335. 10.12701/yujm.2021.01172.
Recovery of the ascending reticular activating system and consciousness following comprehensive management in a patient with traumatic brain injury: a case report
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, Yeungnam University College of Medicine, Daegu, Korea
- KMID: 2534661
- DOI: http://doi.org/10.12701/yujm.2021.01172
Abstract
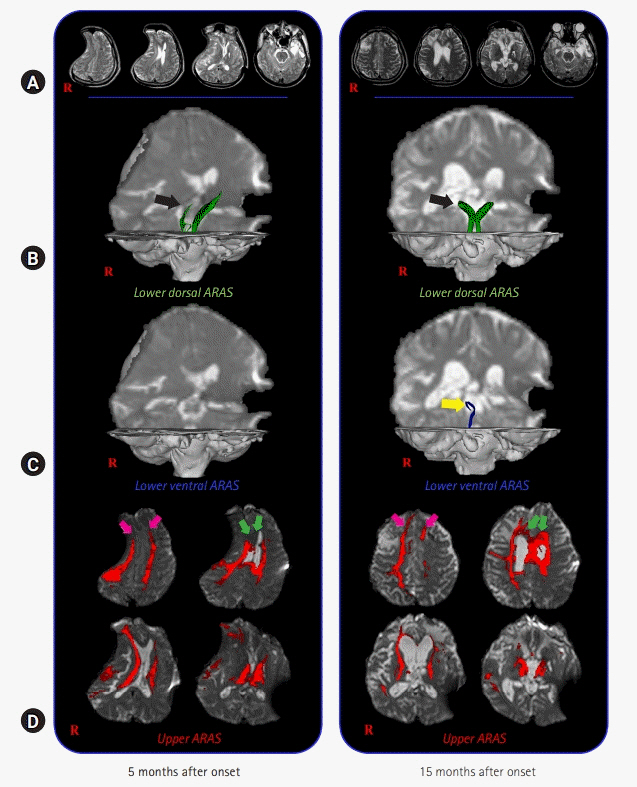
- We report on changes in the ascending reticular activating system (ARAS) concurrent with the recovery of impaired consciousness following rehabilitation and cranioplasty in a patient with traumatic brain injury (TBI), which were demonstrated on diffusion tensor tractography (DTT). A 34-year-old male patient was diagnosed with a traumatic intracerebral hemorrhage after falling from a height of approximately 7 m and underwent a right frontoparietotemporal decompressive craniectomy and hematoma removal. At 5 months after onset, when starting rehabilitation, the patient showed impaired consciousness, with a Glasgow Coma Scale (GCS) score of 4. Comprehensive rehabilitative therapy was provided until 14 months after onset, and his GCS score improved to 8. Cranioplasty was performed using auto-bone at 14 months after onset. One month after cranioplasty, his GCS score improved to 12. On the 15-month DTT, the deviated lower dorsal ARAS was restored on both sides, and the right side had become thicker. The right lower ventral ARAS was reconstructed, and increased neural connectivity of the upper ARAS was detected in both the prefrontal cortices. Thus, changes in the ARAS were demonstrated in a patient with TBI during recovery of consciousness following rehabilitation and cranioplasty.
Keyword
Figure
Reference
-
References
1. Paus T. Functional anatomy of arousal and attention systems in the human brain. Prog Brain Res. 2000; 126:65–77.
Article2. Zeman A. Consciousness. Brain. 2001; 124(Pt 7):1263–89.
Article3. Jang SH, Kim SH, Lim HW, Yeo SS. Recovery of injured lower portion of the ascending reticular activating system in a patient with traumatic brain injury. Am J Phys Med Rehabil. 2015; 94:250–3.
Article4. Jang SH, Chang CH, Jung YJ, Seo YS. Change of ascending reticular activating system with recovery from vegetative state to minimally conscious state in a stroke patient. Medicine (Baltimore). 2016; 95:e5234.
Article5. Jang SH, Hyun YJ, Lee HD. Recovery of consciousness and an injured ascending reticular activating system in a patient who survived cardiac arrest: a case report. Medicine (Baltimore). 2016; 95:e4041.6. Jang SH, Kwon YH. Effect of repetitive transcranial magnetic stimulation on the ascending reticular activating system in a patient with disorder of consciousness: a case report. BMC Neurol. 2020; 20:37.
Article7. Jang SH, Lee HD. Recovery of an injured ascending reticular activating system with recovery from a minimally conscious state to normal consciousness in a stroke patient: a diffusion tensor tractography study. Neural Regen Res. 2020; 15:1767–8.
Article8. Jang SH, Seo YS, Lee SJ. Increased thalamocortical connectivity to the medial prefrontal cortex with recovery of impaired consciousness in a stroke patient: a case report. Medicine (Baltimore). 2020; 99:e19937.9. Jang SH, Kim SH, Seo JP. Long-term recovery from a minimally responsive state with recovery of an injured ascending reticular activating system: a case report. Medicine (Baltimore). 2021; 100:e23933.10. Stelling H, Graham L, Mitchell P. Does cranioplasty following decompressive craniectomy improve consciousness? Br J Neurosurg. 2011; 25:407–9.
Article11. Teasdale G, Jennett B. Assessment of coma and impaired consciousness: a practical scale. Lancet. 1974; 2:81–4.12. Schiff ND. Recovery of consciousness after brain injury: a mesocircuit hypothesis. Trends Neurosci. 2010; 33:1–9.
Article13. Yeo SS, Chang PH, Jang SH. The ascending reticular activating system from pontine reticular formation to the thalamus in the human brain. Front Hum Neurosci. 2013; 7:416.
Article14. Jang SH, Kwon HG. The ascending reticular activating system from pontine reticular formation to the hypothalamus in the human brain: a diffusion tensor imaging study. Neurosci Lett. 2015; 590:58–61.
Article15. Jang SH, Lim HW, Yeo SS. The neural connectivity of the intralaminar thalamic nuclei in the human brain: a diffusion tensor tractography study. Neurosci Lett. 2014; 579:140–4.
Article16. Laureys S, Faymonville ME, Luxen A, Lamy M, Franck G, Maquet P. Restoration of thalamocortical connectivity after recovery from persistent vegetative state. Lancet. 2000; 355:1790–1.
Article17. Yamada K, Sakai K, Akazawa K, Yuen S, Nishimura T. MR tractography: a review of its clinical applications. Magn Reson Med Sci. 2009; 8:165–74.
Article18. Lee SK, Kim DI, Kim J, Kim DJ, Kim HD, Kim DS, et al. Diffusion-tensor MR imaging and fiber tractography: a new method of describing aberrant fiber connections in developmental CNS anomalies. Radiographics. 2005; 25:53–68.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Delayed Surgical Management of Traumatic Pseudoaneurysm of the Ascending Aorta in Multiple Trauma
- The Upper Ascending Reticular Activating System between Intralaminar Thalamic Nuclei and Cerebral Cortex in the Human Brain
- Injury of the Lower Ascending Reticular Activating System by Subfalcine Herniation in a Patient With a Cerebral Infarct
- The Effect of Demeclocycline on the Management of Syndrome of Inappropriate Secretion of Antidiuretic Hormone in Brain Injured Patient
- Anesthetic management of the traumatic brain injury patients undergoing non-neurosurgery