J Korean Med Sci.
2022 Oct;37(40):e292. 10.3346/jkms.2022.37.e292.
Neutrophil-Lymphocyte Ratio and Monocyte-Lymphocyte Ratio According to the Radiologic Severity of Mycobacterium avium Complex Pulmonary Disease
- Affiliations
-
- 1Department of Internal Medicine, Dongsan Medical Center, Keimyung University School of Medicine, Daegu, Korea
- 2Division of Pulmonology and Critical Care Medicine, Department of Internal Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 3Department of Infectious Diseases, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2534333
- DOI: http://doi.org/10.3346/jkms.2022.37.e292
Abstract
- Background
To date, no study has investigated whether the neutrophil-lymphocyte ratio (NLR) and monocyte-lymphocyte ratio (MLR) have a clinical value in Mycobacterium avium complex (MAC)-pulmonary disease (PD).
Methods
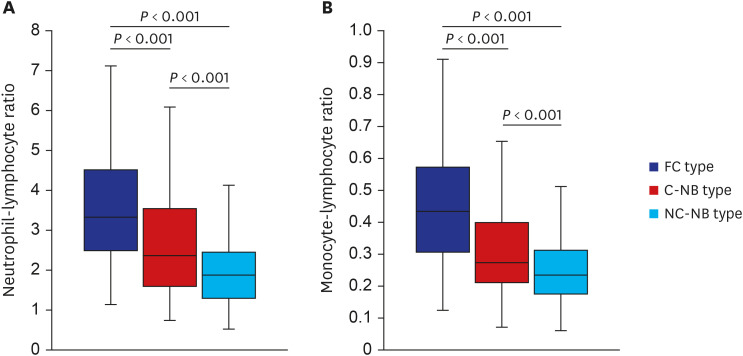
We aimed to assess whether the baseline NLR and MLR were different according to the severity of MAC-PD based on the radiologic classification by retrospectively analyzing 549 patients treated in a tertiary referral center in South Korea.
Results
Both NLR and MLR were significantly higher as 3.33 and 0.43 respectively in the fibrocavitary type, followed by 2.34 and 0.27 in the cavitary nodular bronchiectatic type and significantly lower as 1.88 and 0.23 in the non-cavitary nodular bronchiectatic type.
Conclusion
The baseline NLR and MLR showed a distinct difference in accordance with the radiologic severity of MAC-PD.
Figure
Reference
-
1. Han Y, Kim SJ, Lee SH, Sim YS, Ryu YJ, Chang JH, et al. High blood neutrophil-lymphocyte ratio associated with poor outcomes in miliary tuberculosis. J Thorac Dis. 2018; 10(1):339–346. PMID: 29600065.
Article2. Yin Y, Kuai S, Liu J, Zhang Y, Shan Z, Gu L, et al. Pretreatment neutrophil-to-lymphocyte ratio in peripheral blood was associated with pulmonary tuberculosis retreatment. Arch Med Sci. 2017; 13(2):404–411. PMID: 28261295.
Article3. Iliaz S, Iliaz R, Ortakoylu G, Bahadir A, Bagci BA, Caglar E. Value of neutrophil/lymphocyte ratio in the differential diagnosis of sarcoidosis and tuberculosis. Ann Thorac Med. 2014; 9(4):232–235. PMID: 25276243.
Article4. Ngahane BH, Ebenezer AT, Eveline ND, Raïssa MN, Fernando KL, Lum CV, et al. Diagnostic value of leukocyte count abnormalities in newly diagnosed tuberculosis patients. Open J Respir Dis. 2019; 10(1):1–10.
Article5. Wang W, Wang LF, Liu YY, Yang F, Zhu L, Zhang XH. Value of the ratio of monocytes to lymphocytes for monitoring tuberculosis therapy. Can J Infect Dis Med Microbiol. 2019; 3270393. PMID: 31263513.
Article6. Daley CL, Iaccarino JM, Lange C, Cambau E, Wallace RJ Jr, Andrejak C, et al. Treatment of nontuberculous mycobacterial pulmonary disease: an official ATS/ERS/ESCMID/IDSA clinical practice guideline. Clin Infect Dis. 2020; 71(4):e1–36. PMID: 32628747.
Article7. Koh WJ, Moon SM, Kim SY, Woo MA, Kim S, Jhun BW, et al. Outcomes of Mycobacterium avium complex lung disease based on clinical phenotype. Eur Respir J. 2017; 50(3):1602503. PMID: 28954780.8. Jhun BW, Moon SM, Jeon K, Kwon OJ, Yoo H, Carriere KC, et al. Prognostic factors associated with long-term mortality in 1445 patients with nontuberculous mycobacterial pulmonary disease: a 15-year follow-up study. Eur Respir J. 2020; 55(1):1900798. PMID: 31619468.
Article9. Ong CW, Elkington PT, Friedland JS. Tuberculosis, pulmonary cavitation, and matrix metalloproteinases. Am J Respir Crit Care Med. 2014; 190(1):9–18. PMID: 24713029.
Article10. Yoon NB, Son C, Um SJ. Role of the neutrophil-lymphocyte count ratio in the differential diagnosis between pulmonary tuberculosis and bacterial community-acquired pneumonia. Ann Lab Med. 2013; 33(2):105–110. PMID: 23482854.
Article11. Lyadova IV. Neutrophils in tuberculosis: heterogeneity shapes the way? Mediators Inflamm. 2017; 2017:8619307. PMID: 28626346.
Article12. de Melo MG, Mesquita ED, Oliveira MM, da Silva-Monteiro C, Silveira AK, Malaquias TS, et al. Imbalance of NET and alpha-1-antitrypsin in tuberculosis patients is related with hyper inflammation and severe lung tissue damage. Front Immunol. 2019; 9:3147. PMID: 30687336.
Article13. Fenton MJ, Vermeulen MW. Immunopathology of tuberculosis: roles of macrophages and monocytes. Infect Immun. 1996; 64(3):683–690. PMID: 8641767.
Article14. Lavalett L, Ortega H, Barrera LF. Infection of monocytes from tuberculosis patients with two virulent clinical isolates of Mycobacterium tuberculosis induces alterations in myeloid effector functions. Front Cell Infect Microbiol. 2020; 10:163. PMID: 32391286.15. Rakotosamimanana N, Richard V, Raharimanga V, Gicquel B, Doherty TM, Zumla A, et al. Biomarkers for risk of developing active tuberculosis in contacts of TB patients: a prospective cohort study. Eur Respir J. 2015; 46(4):1095–1103. PMID: 26250497.
Article16. Urbanowski ME, Ordonez AA, Ruiz-Bedoya CA, Jain SK, Bishai WR. Cavitary tuberculosis: the gateway of disease transmission. Lancet Infect Dis. 2020; 20(6):e117–e128. PMID: 32482293.
Article17. Cohen R, Muzaffar S, Capellan J, Azar H, Chinikamwala M. The validity of classic symptoms and chest radiographic configuration in predicting pulmonary tuberculosis. Chest. 1996; 109(2):420–423. PMID: 8620716.
Article18. Kwon YS, Koh WJ. Diagnosis and treatment of nontuberculous mycobacterial lung disease. J Korean Med Sci. 2016; 31(5):649–659. PMID: 27134484.
Article19. Kwon BS, Lee JH, Koh Y, Kim WS, Song JW, Oh YM, et al. The natural history of non-cavitary nodular bronchiectatic Mycobacterium avium complex lung disease. Respir Med. 2019; 150:45–50. PMID: 30961950.
Article20. Kim HJ, Kwak N, Hong H, Kang N, Im Y, Jhun BW, et al. BACES score for predicting mortality in nontuberculous mycobacterial pulmonary disease. Am J Respir Crit Care Med. 2021; 203(2):230–236. PMID: 32721164.
Article21. Kwas H, Guermazi E, Zendah I, Ben Jemia E, Khattab A, Khouaja I, et al. C-reactive protein and pulmonary tuberculosis: what correlation with disease severity. Eur Respir J. 2015; 46:PA2751.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Relationships Between Schizophrenia Severity and Inflammatory Biomarker: Neutrophil/Lymphocyte Ratio, Monocyte/Lymphocyte Ratio, Platelet/Lymphocyte Ratio
- Inflammatory Biomarkers and Bipolar Disorder: Neutrophil/Lymphocyte Ratio, Monocyte/Lymphocyte Ratio and Platelet/Lymphocyte Ratio
- Rapid identification of mycobacterium avium and mycobacterium intracellulare by the amplification of rRNA sequences
- Mycobacterium intracellulare pulmonary infection accompanied with pleural effusion
- Association between gestational age at delivery and lymphocyte-monocyte ratio in the routine second trimester complete blood cell count