J Korean Med Sci.
2022 Oct;37(40):e291. 10.3346/jkms.2022.37.e291.
Nationwide Survey for Pediatric Gastrostomy Tube Placement in Korea
- Affiliations
-
- 1Department of Pediatrics, School of Medicine, Kyungpook National University, Daegu, Korea
- 2Department of Pediatrics, Jeonbuk National University Medical School and Hospital, Jeonju, Korea
- 3Research Institute of Clinical Medicine of Jeonbuk National University - Biomedical Research Institute of Jeonbuk National University Hospital, Jeonju, Korea
- KMID: 2534332
- DOI: http://doi.org/10.3346/jkms.2022.37.e291
Abstract
- Background
Various methods have been implemented for pediatric gastrostomy tube placement. We aimed to investigate the performance status of pediatric gastrostomy in South Korea and to present indications and appropriate methods for domestic situations.
Methods
A survey was conducted among pediatric endoscopists who performed upper gastrointestinal endoscopy in Korea. The questionnaire consisted of 16 questions on gastrostomy performance status.
Results
Among the 48 institutions where the survey was applied, 36 (75%) responded. Of the 36 institutions, gastrostomy was performed in 31 (86.1%). The departments in which gastrostomy was performed were pediatrics at 26 institutions (81.3%), surgery at 24 institutions (75.0%), internal medicine at 9 institutions (28.1%), and radiology at 7 institutions (21.9%). There were 18 institutions (66.7%) using the pull method for percutaneous endoscopic gastrostomy (PEG) and nine institutions (33.3%) using the push method. When performing gastrostomies, fundoplication procedures were performed in 19 institutions (61.3%), if deemed necessary. However, 12 institutions (38.7%) answered that gastrostomy was always implemented alone. Complications after gastrostomy included buried bumper syndrome, wound infection, leakage, tube migration, and incorrect opening site in the stomach, but the number of cases with complications was very small.
Conclusion
In Korea, a pediatric gastrostomy is implemented in various ways depending on the institution. Clinicians are concerned about choosing the most effective methods with fewer complications after the procedure. In our study, we reported only a few complications. Korea has good accessibility for pediatric gastrointestinal endoscopy, and this survey showed that it is a safe procedure that can be considered initially in pediatric gastrostomy. This study is expected to help to create optimal pediatric PEG guidelines in Korea.
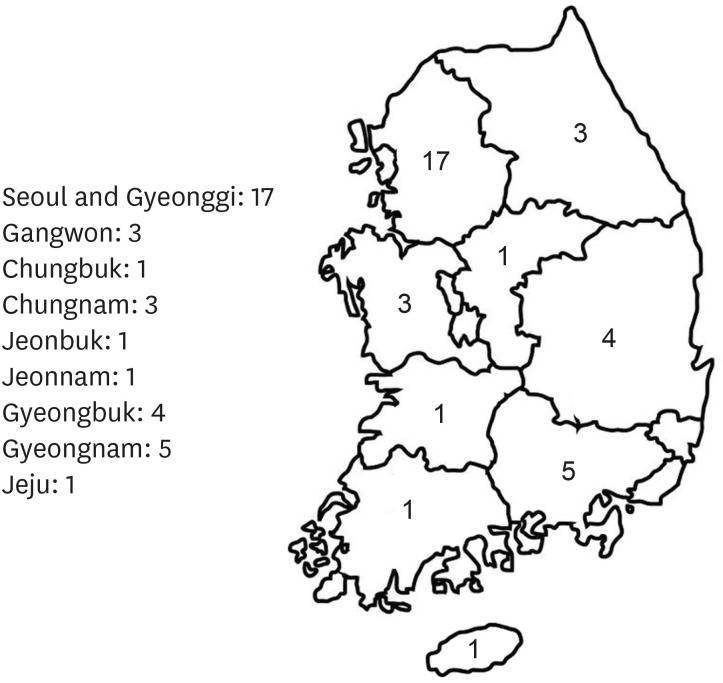
Figure
Cited by 1 articles
-
Pediatric Percutaneous Endoscopic Gastrostomy in Korea - When? By Whom? How?
Yoon Lee
J Korean Med Sci. 2022;37(40):e313. doi: 10.3346/jkms.2022.37.e313.
Reference
-
1. Rahnemai-Azar AA, Rahnemaiazar AA, Naghshizadian R, Kurtz A, Farkas DT. Percutaneous endoscopic gastrostomy: indications, technique, complications and management. World J Gastroenterol. 2014; 20(24):7739–7751. PMID: 24976711.
Article2. Homan M, Hauser B, Romano C, Tzivinikos C, Torroni F, Gottrand F, et al. Percutaneous endoscopic gastrostomy in children: an update to the ESPGHAN position paper. J Pediatr Gastroenterol Nutr. 2021; 73(3):415–426. PMID: 34155150.
Article3. de Sousa Magalhães R, Cúrdia Gonçalves T, Sousa-Pinto B, Rosa B, Marinho C, Cotter J. Percutaneous endoscopic gastrostomy: dealing with the issue of dislodgement. Scand J Gastroenterol. 2020; 55(4):485–491. PMID: 32202441.
Article4. Sandberg F, Viktorsdóttir MB, Salö M, Stenström P, Arnbjörnsson E. Comparison of major complications in children after laparoscopy-assisted gastrostomy and percutaneous endoscopic gastrostomy placement: a meta-analysis. Pediatr Surg Int. 2018; 34(12):1321–1327. PMID: 30291404.
Article5. Zenitani M, Nose S, Sasaki T, Oue T. Safety and efficacy of laparoscopy-assisted percutaneous endoscopic gastrostomy in infants and small children weighing less than 10 kg: a comparison with larger patients. Asian J Endosc Surg. 2021; 14(1):44–49. PMID: 32319215.
Article6. Fraser JD, Aguayo P, Sharp SW, Holcomb GW 3rd, Ostlie DJ, St Peter SD. The safety of laparoscopy in pediatric patients with ventriculoperitoneal shunts. J Laparoendosc Adv Surg Tech A. 2009; 19(5):675–678. PMID: 19645606.
Article7. Blumenstein I, Shastri YM, Stein J. Gastroenteric tube feeding: techniques, problems and solutions. World J Gastroenterol. 2014; 20(26):8505–8524. PMID: 25024606.
Article8. Mawatari F, Miyaaki H, Arima T, Ito H, Matsuki K, Fukuda S, et al. Procedure-related complications and survival after gastrostomy: results from a Japanese cohort. Ann Nutr Metab. 2020; 76(6):413–421. PMID: 33626540.
Article9. Gang MH, Kim JY. Short-term complications of percutaneous endoscopic gastrostomy according to the type of technique. Pediatr Gastroenterol Hepatol Nutr. 2014; 17(4):214–222. PMID: 25587521.
Article10. Ota K, Takeuchi T, Masuda D, Sanomura M, Kojima K, Nakanishi Y, et al. Risk factors for postoperative bleeding and early death in percutaneous endoscopic gastrostomy: a multicenter retrospective study. J Gastroenterol Hepatol. 2022; 37(1):97–103. PMID: 34478183.
Article11. Lee SW, Lee JH, Cho H, Ha Y, Lim H, Ahn JY, et al. Comparison of clinical outcomes associated with pull-type and introducer-type percutaneous endoscopic gastrostomies. Clin Endosc. 2014; 47(6):530–537. PMID: 25505719.
Article12. Osei H, Munoz-Abraham AS, Martino A, Chatoorgoon K, Greenspon J, Fitzpatrick C, et al. To button or not to button? Primary gastrostomy tubes offer no significant advantage over buttons. Pediatr Gastroenterol Hepatol Nutr. 2022; 25(3):211–217. PMID: 35611372.
Article13. Kumar AS, Bani Yaghoub M, Rekab K, Hall M, Attard TM. Pediatric multicenter cohort comparison of percutaneous endoscopic and non-endoscopic gastrostomy technique outcomes. J Investig Med. 2020; 68(2):413–418.
Article14. Salazar JH, Spanbauer C, Sood MR, Densmore JC, Van Arendonk KJ. Variability in the method of gastrostomy placement in children. Children (Basel). 2020; 7(6):53.
Article15. Balogh B, Szűcs D, Gavallér G, Rieth A, Kovács T. Laparoscopic-assisted percutaneous endoscopic gastrostomy reduces major complications in high-risk pediatric patients. Pediatr Gastroenterol Hepatol Nutr. 2021; 24(3):273–278. PMID: 34046330.
Article16. Yoon S, Kim SH, Lee YJ, Park JH, Cho YH, Chung JH. Experience with a hybrid procedure involving laparoscopic fundoplication with percutaneous endoscopic gastrostomy in chronically ill children. J Clin Med. 2021; 10(19):4291. PMID: 34640329.
Article17. Kim SC. Letter to the editor: optimal method for sedation of pediatric upper gastrointestinal endoscopy. J Korean Med Sci. 2021; 36(35):e254. PMID: 34490758.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Complications of Gastrostomy and Gastrojejunostomy: The Prevalence in Children
- Percutaneous Gastrostomy Tube Reinsertion after Accidental Dislodgement Using Modified Seldinger's Technique
- A Case of Severe Gastric Ulcer Bleeding after Exchange for Replacement Balloon Gastrostomy Tube in Percutaneous Endoscopic Gastrostomy
- Duodenal Perforation: Unusual Complication of Gastrostomy Tube Replacement
- Massive Gastric Bleeding Occuring after the Replacement of Percutaneous Endoscopic Gastrostomy Tube