J Stroke.
2022 Sep;24(3):417-420. 10.5853/jos.2022.01200.
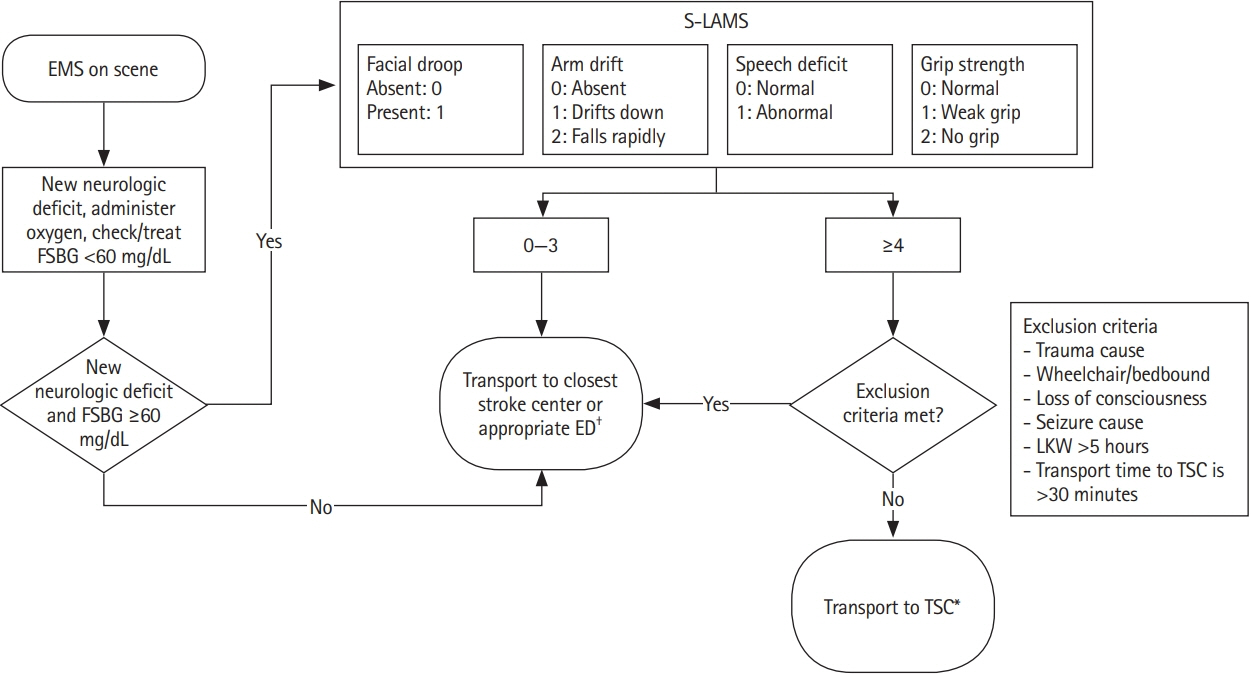
Updated New York City Emergency Medical Services Acute Stroke Triage Protocol Reduces Interfacility Transfers and Time to Endovascular Thrombectomy for Emergent Large Vessel Occlusion Stroke Patients
- Affiliations
-
- 1Department of Emergency Medicine, Icahn School of Medicine at Mount Sinai, New York, NY, USA
- 2Department of Neurology, Icahn School of Medicine at Mount Sinai, New York, NY, USA
- 3Department of Neurosurgery, Icahn School of Medicine at Mount Sinai, New York, NY, USA
- KMID: 2534271
- DOI: http://doi.org/10.5853/jos.2022.01200
Figure
Reference
-
References
1. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke. A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019; 50:e344–e418.2. Jauch EC, Schwamm LH, Panagos PD, Barbazzeni J, Dickson R, Dunne R, et al. Recommendations for regional stroke destination plans in rural, suburban, and urban communities from the Prehospital Stroke System of Care consensus conference: a consensus statement from the American Academy of Neurology, American Heart Association/American Stroke Association, American Society of Neuroradiology, National Association of EMS Physicians, National Association of State EMS Officials, Society of NeuroInterventional Surgery, and Society of Vascular and Interventional Neurology. Endorsed by the Neurocritical Care Society. Stroke. 2021; 52:e133–e152.3. Bosson N, Gausche-Hill M, Saver JL, Sanossian N, Tadeo R, Clare C, et al. Increased access to and use of endovascular therapy following implementation of a 2-tiered regional stroke system. Stroke. 2020; 51:908–913.4. Mazya MV, Berglund A, Ahmed N, von Euler M, Holmin S, Laska AC, et al. Implementation of a prehospital stroke triage system using symptom severity and teleconsultation in the Stockholm Stroke Triage study. JAMA Neurol. 2020; 77:691–699.5. Kass-Hout T, Lee J, Tataris K, Richards CT, Markul E, Weber J, et al. Prehospital comprehensive stroke center vs primary stroke center triage in patients with suspected large vessel occlusion stroke. JAMA Neurol. 2021; 78:1220–1227.6. Cabal M, Machova L, Vaclavik D, Jasso P, Holes D, Volny O, et al. New prehospital triage for stroke patients significantly reduces transport time of EVT patients without delaying IVT. Front Neurol. 2021; 12:676126.7. Magdon-Ismail Z, Benesch C, Cushman JT, Brissette I, Southerland AM, Brandler ES, et al. Establishing recommendations for stroke systems in the thrombectomy era: the upstate New York stakeholder proceedings. Stroke. 2017; 48:2003–2006.8. Brandler ES, Thode H, Fiorella D. The Los Angeles Motor Scale as a predictor of angiographically determined large vessel occlusion. Intern Emerg Med. 2020; 15:695–700.9. Venema E, Groot AE, Lingsma HF, Hinsenveld W, Treurniet KM, Chalos V, et al. Effect of interhospital transfer on endovascular treatment for acute ischemic stroke. Stroke. 2019; 50:923–930.10. Froehler MT, Saver JL, Zaidat OO, Jahan R, Aziz-Sultan MA, Klucznik RP, et al. Interhospital transfer before thrombectomy is associated with delayed treatment and worse outcome in the STRATIS Registry (Systematic Evaluation of Patients Treated With Neurothrombectomy Devices for Acute Ischemic Stroke). Circulation. 2017; 136:2311–2321.11. Ganti L, Oostema JA. How accurate are the stroke severity scales for identifying large vessel occlusions? Ann Emerg Med. 2020; 75:494–496.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intravenous Thrombolysis and Endovascular Thrombectomy in Acute Ischemic Stroke with Minor Symptom
- Emergency management of stroke in the era of mechanical thrombectomy
- Differences in mechanical thrombectomy for acute ischemic stroke on weekdays versus nights/ weekends in a Japanese primary stroke core center
- Endovascular Revascularization Therapy in a Patient with Acute Ischemic Stroke due to Intracranial Multiple Large-vessel Occlusion
- Emergency Microsurgical Embolectomy for the Treatment of Acute Intracranial Artery Occlusion: Report of Two Cases