J Stroke.
2022 Sep;24(3):345-351. 10.5853/jos.2022.02103.
Establishment of the Heart and Brain Team for Patent Foramen Ovale Closure in Stroke Patients: An Expert Opinion
- Affiliations
-
- 1Department of Neurology, Gangneung Asan Hospital, University of Ulsan College of Medicine, Gangneung, Korea
- 2Stroke Theme, Florey Institute of Neuroscience and Mental Health, Heidelberg, Australia
- 3Department of Cardiology, Austin Health, Heidelberg, Australia
- 4Department of Cerebrovascular Medicine, National Cerebral and Cardiovascular Center, Suita, Japan
- 5Department of Neurology, Beijing Tiantan Hospital, Beijing, China
- 6Interventional Cardiology, St. Thomas’ Hospital, London, UK
- 7Albers Clinical Evidence Consultancy, Winterswijk Woold, The Netherlands
- 8Department of Neuroepidemiology, Institute for Medical Informatics, Biometry and Epidemiology (IMIBE), Medical Faculty of the University Duisburg-Essen, Essen, Germany
- KMID: 2534263
- DOI: http://doi.org/10.5853/jos.2022.02103
Abstract
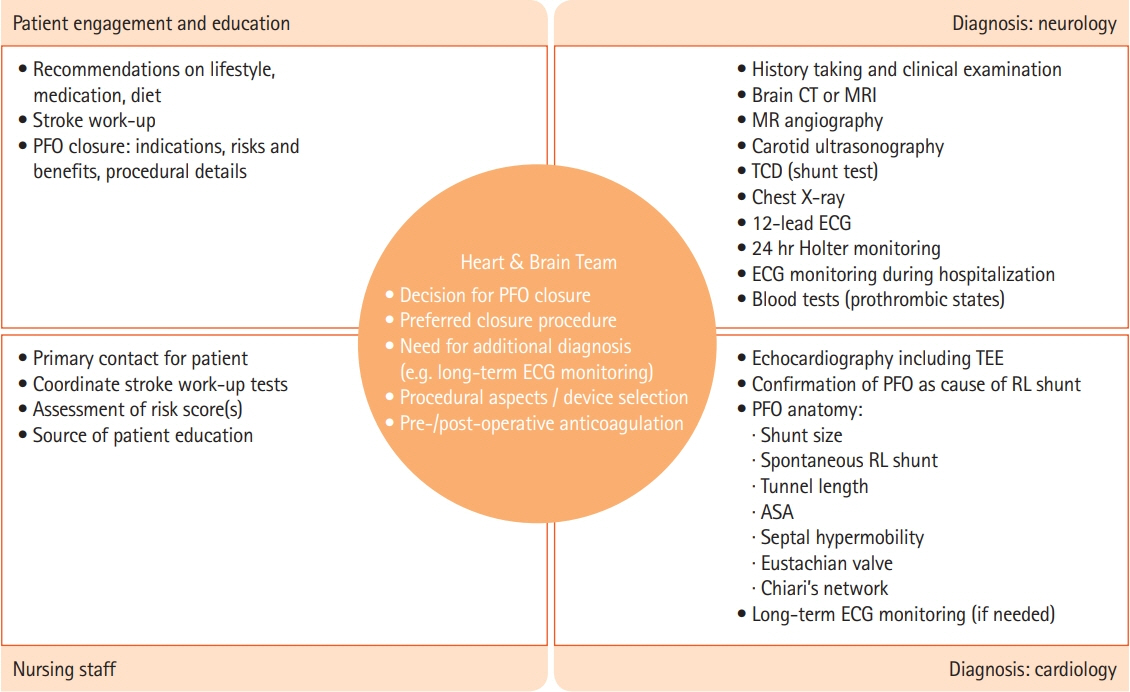
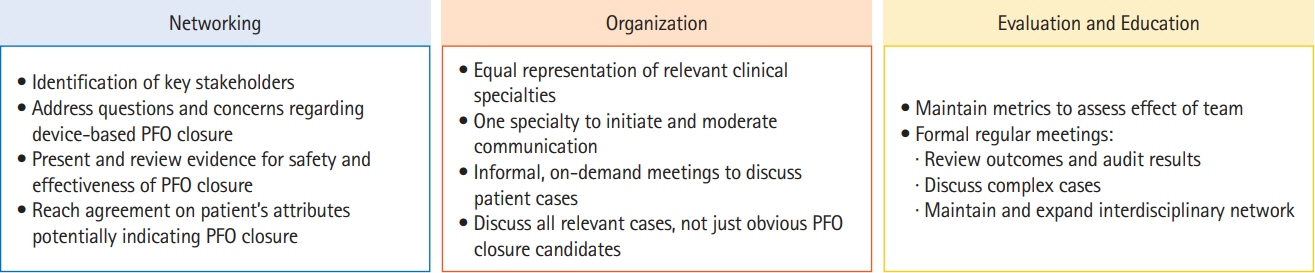
- The online 2021 Asian-Pacific Heart and Brain Summit was organized to present and discuss experiences within leading Asian-Pacific centers with regard to institutional heart and brain teams managing the diagnosis, treatment, and follow-up of cryptogenic stroke (CS) patients with patent foramen ovale (PFO). This manuscript presents a narrative review of presentations and discussions during the summit meeting. Percutaneous PFO closure is an established therapy for CS patients in whom PFO is considered to be causal. Guidelines and consensus statements emphasize the importance of multidisciplinary clinical decision-making regarding PFO closure with the involvement of several clinical specialties, including neurology, cardiology, and hematology. It is also recommended that the patient be closely involved in this process. The heart and brain team is a collaborative platform that facilitates such a multidisciplinary decision-making process and patient involvement. It also creates opportunities for education and evaluation of the healthcare provided to patients with CS. This review provides insights into the implementation, composition, organization, and operation of a heart and brain team. Methods and metrics are suggested to evaluate the team’s role. We suggest that an efficient heart and brain team can implement guideline-recommended multidisciplinary clinical decision-making with regard to PFO closure in CS patients and play an important role in the management of these patients.
Figure
Cited by 2 articles
-
Device Closure or Antithrombotic Therapy After Cryptogenic Stroke in Elderly Patients With a High-Risk Patent Foramen Ovale
Pil Hyung Lee, Jung-Sun Kim, Jae-Kwan Song, Sun U. Kwon, Bum Joon Kim, Ji Sung Lee, Byung Joo Sun, Jong Shin Woo, Soe Hee Ann, Jung-Won Suh, Jun Yup Kim, Kyusup Lee, Sang Yeub Lee, Ran Heo, Soo Jeong, Jeong Yoon Jang, Jang-Whan Bae, Young Dae Kim, Sung Hyuk Heo, Jong S. Kim
J Stroke. 2024;26(2):242-251. doi: 10.5853/jos.2023.03265.Patent Foramen Ovale and Other Cardiopathies as Causes of Embolic Stroke With Unknown Source
Jong S. Kim
J Stroke. 2024;26(3):349-359. doi: 10.5853/jos.2024.02670.
Reference
-
References
1. Søndergaard L, Kasner SE, Rhodes JF, Andersen G, Iversen HK, Nielsen-Kudsk JE, et al. Patent foramen ovale closure or antiplatelet therapy for cryptogenic stroke. N Engl J Med. 2017; 377:1033–1042.2. Saver JL, Carroll JD, Thaler DE, Smalling RW, MacDonald LA, Marks DS, et al. Long-term outcomes of patent foramen ovale closure or medical therapy after stroke. N Engl J Med. 2017; 377:1022–1032.3. Mas JL, Derumeaux G, Guillon B, Massardier E, Hosseini H, Mechtouff L, et al. Patent foramen ovale closure or anticoagulation vs. antiplatelets after stroke. N Engl J Med. 2017; 377:1011–1021.4. Lee PH, Song JK, Kim JS, Heo R, Lee S, Kim DH, et al. Cryptogenic stroke and high-risk patent foramen ovale: the DEFENSE-PFO trial. J Am Coll Cardiol. 2018; 71:2335–2342.5. Furlan AJ, Reisman M, Massaro J, Mauri L, Adams H, Albers GW, et al. Closure or medical therapy for cryptogenic stroke with patent foramen ovale. N Engl J Med. 2012; 366:991–999.6. Meier B, Kalesan B, Mattle HP, Khattab AA, Hildick-Smith D, Dudek D, et al. Percutaneous closure of patent foramen ovale in cryptogenic embolism. N Engl J Med. 2013; 368:1083–1091.7. Ntaios G, Papavasileiou V, Sagris D, Makaritsis K, Vemmos K, Steiner T, et al. Closure of patent foramen ovale versus medical therapy in patients with cryptogenic stroke or transient ischemic attack: updated systematic review and meta-analysis. Stroke. 2018; 49:412–418.8. Kent DM, Saver JL, Kasner SE, Nelson J, Carroll JD, Chatellier G, et al. Heterogeneity of treatment effects in an analysis of pooled individual patient data from randomized trials of device closure of patent foramen ovale after stroke. JAMA. 2021; 326:2277–2286.9. Pristipino C, Sievert H, D’Ascenzo F, Mas JL, Meier B, Scacciatella P, et al. European position paper on the management of patients with patent foramen ovale: general approach and left circulation thromboembolism. EuroIntervention. 2019; 14:1389–1402.10. Horlick E, Kavinsky CJ, Amin Z, Boudoulas KD, Carroll JD, Hijazi ZM, et al. SCAI expert consensus statement on operator and institutional requirements for PFO closure for secondary prevention of paradoxical embolic stroke: the American Academy of Neurology affirms the value of this statement as an educational tool for neurologists. Catheter Cardiovasc Interv. 2019; 93:859–874.11. Kleindorfer DO, Towfighi A, Chaturvedi S, Cockroft KM, Gutierrez J, Lombardi-Hill D, et al. 2021 Guideline for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline from the American Heart Association/ American Stroke Association. Stroke. 2021; 52:e364–e467.12. Messé SR, Gronseth GS, Kent DM, Kizer JR, Homma S, Rosterman L, et al. Practice advisory update summary: patent foramen ovale and secondary stroke prevention: report of the guideline subcommittee of the American Academy of Neurology. Neurology. 2020; 94:876–885.13. Amplatzer PFO occlude: instructions for use. Abbott;https:////manuals.sjm.com/Search-Form?re=North-America&cc=US&ln=EN&ct=professional&fam=861f73cb-e36b-4f06-a58f4b11fa263dcf&cat=71260c89-7cb8-475d-950b0262191e7526&seg=dd28d64f-7d0b-4660-aa2c-da987bb7894c&ipp=10. 2022. Accessed August 17, 2022.14. Gore Cardioform: instructions for use. W. L. Gore & Associates Inc.;https://www.goremedical.com. 2022. Accessed August 17, 2022.15. Buck BH, Hill MD, Quinn FR, Butcher KS, Menon BK, Gulamhusein S, et al. Effect of implantable vs prolonged external electrocardiographic monitoring on atrial fibrillation detection in patients with ischemic stroke: the PER DIEM randomized clinical trial. JAMA. 2021; 325:2160–2168.16. Thijs VN, Brachmann J, Morillo CA, Passman RS, Sanna T, Bernstein RA, et al. Predictors for atrial fibrillation detection after cryptogenic stroke: results from CRYSTAL AF. Neurology. 2016; 86:261–269.17. Xu J, Sethi P, Biby S, Allred J, Seiler A, Sabir R. Predictors of atrial fibrillation detection and features of recurrent strokes in patients after cryptogenic stroke. J Stroke Cerebrovasc Dis. 2020; 29:104934.18. Sudacevschi V, Bertrand C, Chadenat ML, Tarnaud C, Pico F. Predictors of occult atrial fibrillation in one hundred seventy-one patients with cryptogenic transient ischemic attack and minor stroke. J Stroke Cerebrovasc Dis. 2016; 25:2673–2677.19. Elgendy AY, Saver JL, Amin Z, Boudoulas KD, Carroll JD, Elgendy IY, et al. Proposal for updated nomenclature and classification of potential causative mechanism in patent foramen ovale-associated stroke. JAMA Neurol. 2020; 77:878–886.20. Kent DM, Ruthazer R, Weimar C, Mas JL, Serena J, Homma S, et al. An index to identify stroke-related vs incidental patent foramen ovale in cryptogenic stroke. Neurology. 2013; 81:619–625.21. Schellinger PD, Tsivgoulis G, Steiner T, Köhrmann M. Percutaneous left atrial appendage occlusion for the prevention of stroke in patients with atrial fibrillation: review and critical appraisal. J Stroke. 2018; 20:281–291.22. Cruz-González I, Trejo-Velasco B, Redondo-Robles L, López-Mesonero L, González-Ferreiro R, Núñez JC, et al. Left atrial appendage occlusion: an alternative to triple therapy in stroke patients undergoing carotid angioplasty. J Stroke. 2020; 22:268–270.23. Collado FM, Kavinsky CJ. The heart-brain team approach in patent foramen ovale closure. Front Neurol. 2020; 11:561938.24. Kasner SE, Lattanzi S, Fonseca AC, Elgendy AY. Uncertainties and controversies in the management of ischemic stroke and transient ischemic attack patients with patent foramen ovale. Stroke. 2021; 52:e806–e819.25. Morais LA, Sousa L, Fiarresga A, Martins JD, Timóteo AT, Monteiro AV, et al. RoPE score as a predictor of recurrent ischemic events after percutaneous patent foramen ovale closure. Int Heart J. 2018; 59:1327–1332.26. Mazzucco S, Li L, Binney L, Rothwell PM; Oxford Vascular Study Phenotyped Cohort. Prevalence of patent foramen ovale in cryptogenic transient ischaemic attack and non-disabling stroke at older ages: a population-based study, systematic review, and meta-analysis. Lancet Neurol. 2018; 17:609–617.27. Kwon H, Lee PH, Song JK, Kwon SU, Kang DW, Kim JS. Patent foramen ovale closure in old stroke patients: a subgroup analysis of the DEFENSE-PFO trial. J Stroke. 2021; 23:289–292.28. Kim JS, Hong KS. Patent foramen ovale closure: opportunity closed in old patients? J Stroke. 2021; 23:147–148.29. Baik M, Shim CY, Gwak SY, Kim YD, Nam HS, Lee HS, et al. Patent foramen ovale and risk of recurrence in stroke of determined etiology. Ann Neurol. 2022; Jun. 26. [Epub]. https://doi.org/10.1002/ana.26449.30. Tobis JM, Charles A, Silberstein SD, Sorensen S, Maini B, Horwitz PA, et al. Percutaneous closure of patent foramen ovale in patients with migraine: the premium trial. J Am Coll Cardiol. 2017; 70:2766–2774.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Transcatheter Closure of Patent Foramen Ovale in a Stroke Patient under the Guidance of Transesophageal Echocardiography
- Patent Foramen Ovale and Cryptogenic Stroke
- Patent Foramen Ovale and Stroke-Current Status
- A New Method for Patent Foramen Ovale Closure: Delivering Sheath Over Coronary Sinus Catheter into Left Atrium
- Percutaneous Patent Foramen Ovale Closure After Stroke