Korean J Pain.
2022 Oct;35(4):468-474. 10.3344/kjp.2022.35.4.468.
Post-COVID-19 pain syndrome: a descriptive study in Turkish population
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, International School of Medicine, Istanbul Medipol University, Istanbul, Turkiye
- 2Department of Ear Nose Throat Diseases, International School of Medicine, Istanbul Medipol University, Istanbul, Turkiye
- 3Department of Family Medicine, International School of Medicine, Istanbul Medipol University, Istanbul, Turkiye
- KMID: 2533987
- DOI: http://doi.org/10.3344/kjp.2022.35.4.468
Abstract
- Background
The new type of corona virus has a wide range of symptoms. Some people who have COVID-19 can experience long-term effects from their infection, known as post-COVID conditions. The authors aimed to investigate prolonged musculoskeletal pain as a symptom of the post-COVID-19 condition.
Methods
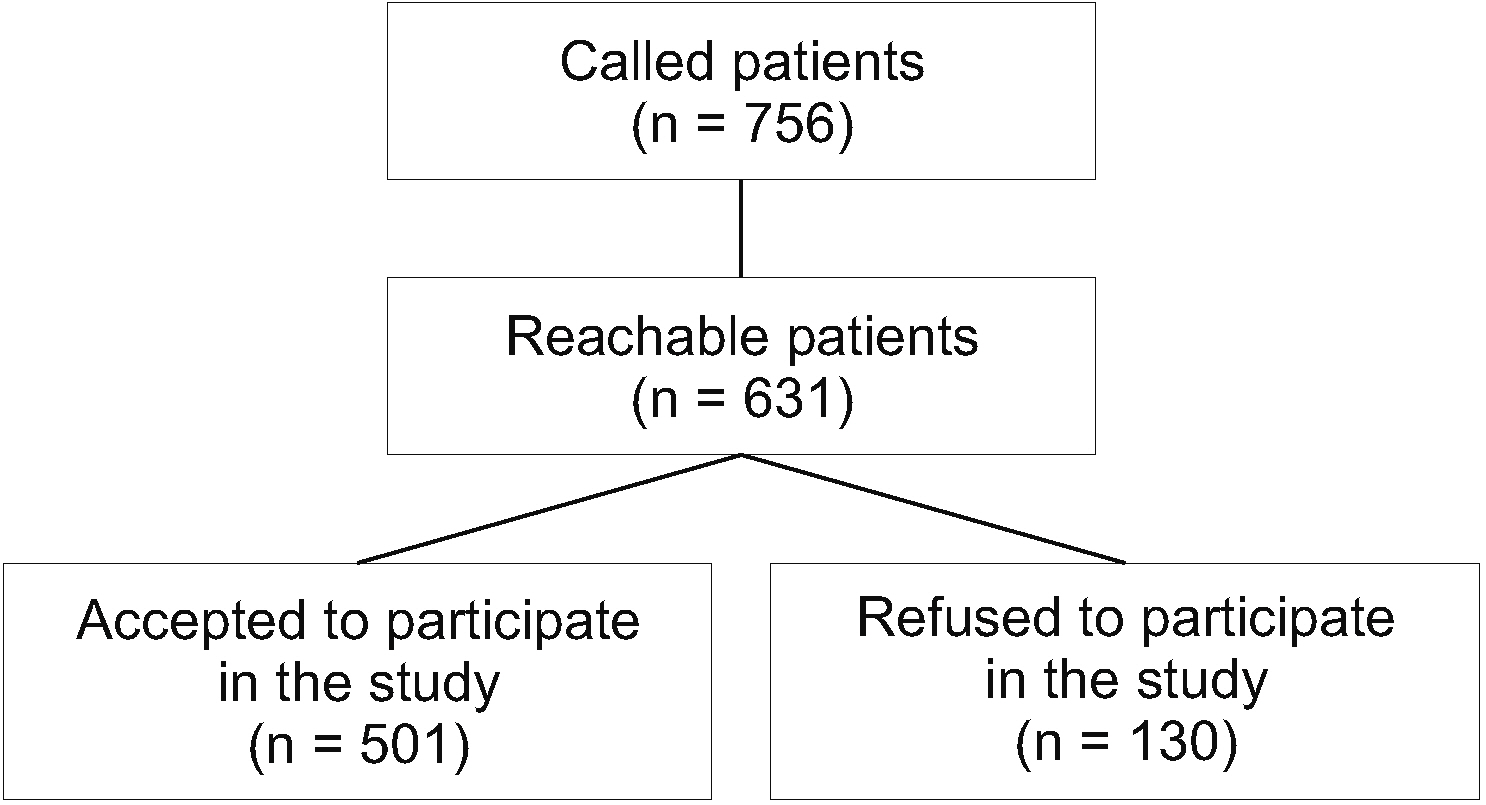
This is a descriptive study on the patients who were diagnosed with COVID-19 in a university hospital, between March 2020 and March 2021. Patient records and an extensive questionnaire were used to obtain relevant demographic and clinical characteristics, including hospitalization history, comorbidities, smoking history, duration of the pain, the area of pain, and the presence of accompanying neuropathic symptoms.
Results
Of the diagnosed patients, 501 agreed to participate in the study. Among the participants, 318 had musculoskeletal pain during COVID-19 infection, and 69 of them reported prolonged pain symptoms as part of their a post-COVID condition which could not be attributed to any other cause. The mean duration of pain was 4.38 ± 1.73 months, and the mean pain level was 7.2 ± 4.3. Neuropathic pain symptoms such as burning sensation (n = 16, 23.2%), numbness (n = 15, 21.7%), tingling (n = 10, 14.5%), stinging (n = 4, 5.8%), freezing (n = 1, 1.4%) were accompanied in patients with prolonged musculoskeletal pain.
Conclusions
Patients with COVID-19 may develop prolonged musculoskeletal pain. In some patients, neuropathic pain accompanies it. Awareness of prolonged postCOVID-19 pain is crucial for its early detection and management.
Keyword
Figure
Reference
-
1. Wu Z, McGoogan JM. 2020; Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 323:1239–42. DOI: 10.1001/jama.2020.2648. PMID: 32091533. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85081266700&origin=inward.
Article2. Cucinotta D, Vanelli M. 2020; WHO declares COVID-19 a pandemic. Acta Biomed. 91:157–60. DOI: 10.23750/abm.v91i1.9397. PMID: 32191675. PMCID: PMC7569573. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85082061557&origin=inward.3. National Institute for Health and Care Excellence (NICE). Royal College of General Practitioners. Healthcare Improvement Scotland, Scottish Intercollegiate Guidelines Network (SIGN). 2020. COVID-19 rapid guideline: managing the long-term effects of COVID-19 [Internet]. National Institute for Health and Care Excellence;London: Available at: www.nice.org.uk/guidance/ng188.4. Broderick G, Fuite J, Kreitz A, Vernon SD, Klimas N, Fletcher MA. 2010; A formal analysis of cytokine networks in chronic fatigue syndrome. Brain Behav Immun. 24:1209–17. DOI: 10.1016/j.bbi.2010.04.012. PMID: 20447453. PMCID: PMC2939140. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=78049413398&origin=inward.
Article5. Ackermann M, Verleden SE, Kuehnel M, Haverich A, Welte T, Laenger F, et al. 2020; Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in Covid-19. N Engl J Med. 383:120–8. DOI: 10.1056/NEJMoa2015432. PMID: 32437596. PMCID: PMC7412750. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85086722950&origin=inward.
Article6. Garg P, Arora U, Kumar A, Wig N. 2021; The "post-COVID" syndrome: how deep is the damage? J Med Virol. 93:673–4. DOI: 10.1002/jmv.26465. PMID: 32852801. PMCID: PMC7461449. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85091685361&origin=inward.
Article7. Yalcin HC, Sukumaran V, Al-Ruweidi MKAA, Shurbaji S. 2021; Do changes in ACE-2 expression affect SARS-CoV-2 virulence and related complications: a closer look into membrane-bound and soluble forms. Int J Mol Sci. 22:6703. DOI: 10.3390/ijms22136703. PMID: 34201415. PMCID: PMC8269184. PMID: 1ee0fb9e061043cc8b2e132c7759a0bb. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85108201510&origin=inward.
Article8. Pons S, Fodil S, Azoulay E, Zafrani L. 2020; The vascular endothelium: the cornerstone of organ dysfunction in severe SARS-CoV-2 infection. Crit Care. 24:353. DOI: 10.1186/s13054-020-03062-7. PMID: 32546188. PMCID: PMC7296907. PMID: 3956db0a549d4e29858228d9de82731d. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85086622787&origin=inward.
Article9. Paliwal VK, Garg RK, Gupta A, Tejan N. 2020; Neuromuscular presentations in patients with COVID-19. Neurol Sci. 41:3039–56. DOI: 10.1007/s10072-020-04708-8. PMID: 32935156. PMCID: PMC7491599. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85091117000&origin=inward.
Article10. To KF, Lo AW. 2004; Exploring the pathogenesis of severe acute respiratory syndrome (SARS): the tissue distribution of the coronavirus (SARS-CoV) and its putative receptor, angiotensin-converting enzyme 2 (ACE2). J Pathol. 203:740–3. DOI: 10.1002/path.1597. PMID: 15221932. PMCID: PMC7167902. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=3242709581&origin=inward.11. Grichnik KP, Ferrante FM. 1991; The difference between acute and chronic pain. Mt Sinai J Med. 58:217–20. PMID: 1875958. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=0026162142&origin=inward.12. Treede RD, Rief W, Barke A, Aziz Q, Bennett MI, Benoliel R, et al. 2015; A classification of chronic pain for ICD-11. Pain. 156:1003–7. DOI: 10.1097/j.pain.0000000000000160. PMID: 25844555. PMCID: PMC4450869. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=84942259601&origin=inward.
Article13. Trouvin AP, Perrot S. 2019; New concepts of pain. Best Pract Res Clin Rheumatol. 33:101415. DOI: 10.1016/j.berh.2019.04.007. PMID: 31703792. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85065518421&origin=inward.
Article14. Campbell WI, Lewis S. 1990; Visual analogue measurement of pain. Ulster Med J. 59:149–54. PMID: 2278111. PMCID: PMC2448309. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=0025507627&origin=inward.15. Li LQ, Huang T, Wang YQ, Wang ZP, Liang Y, Huang TB, et al. 2020; COVID-19 patients' clinical characteristics, discharge rate, and fatality rate of meta-analysis. J Med Virol. 92:577–83. DOI: 10.1002/jmv.25757. PMID: 32162702. PMCID: PMC7228329. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85082667577&origin=inward.
Article16. Zhu J, Zhong Z, Ji P, Li H, Li B, Pang J, et al. 2020; Clinicopathological characteristics of 8697 patients with COVID-19 in China: a meta-analysis. Fam Med Community Health. 8:e000406. Erratum in: Fam Med Community Health 2020; 8: e000406corr1. DOI: 10.1136/fmch-2020-000406corr1. PMID: 32448784. PMCID: PMC7253001. PMID: 503b41c7cb554290952d4980161cc1f1. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85086332470&origin=inward.
Article17. Lechien JR, Chiesa-Estomba CM, De Siati DR, Horoi M, Le Bon SD, Rodriguez A, et al. 2020; Olfactory and gustatory dysfunctions as a clinical presentation of mild-to-moderate forms of the coronavirus disease (COVID-19): a multicenter European study. Eur Arch Otorhinolaryngol. 277:2251–61. DOI: 10.1007/s00405-020-05965-1. PMID: 32253535. PMCID: PMC7134551. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85083255744&origin=inward.
Article18. Lechien JR, Chiesa-Estomba CM, Place S, Van Laethem Y, Cabaraux P, Mat Q, et al. 2020; Clinical and epidemiological characteristics of 1420 European patients with mild-to-moderate coronavirus disease 2019. J Intern Med. 288:335–44. DOI: 10.1111/joim.13089. PMID: 32352202. PMCID: PMC7267446. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85084488518&origin=inward.
Article19. Corsini Campioli C, Cano Cevallos E, Assi M, Patel R, Binnicker MJ, O'Horo JC. 2020; Clinical predictors and timing of cessation of viral RNA shedding in patients with COVID-19. J Clin Virol. 130:104577. DOI: 10.1016/j.jcv.2020.104577. PMID: 32777762. PMCID: PMC7405830. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85089145335&origin=inward.
Article20. Attal N, Martinez V, Bouhassira D. 2021; Potential for increased prevalence of neuropathic pain after the COVID-19 pandemic. Pain Rep. 6:e884. DOI: 10.1097/PR9.0000000000000884. PMID: 33537521. PMCID: PMC7850724. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85105564590&origin=inward.
Article21. Gan EY, Tian EA, Tey HL. 2013; Management of herpes zoster and post-herpetic neuralgia. Am J Clin Dermatol. 14:77–85. DOI: 10.1007/s40257-013-0011-2. PMID: 23456596. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=84879545856&origin=inward.
Article22. Aksan F, Nelson EA, Swedish KA. 2020; A COVID-19 patient with intense burning pain. J Neurovirol. 26:800–1. DOI: 10.1007/s13365-020-00887-4. PMID: 32779108. PMCID: PMC7416991. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85089292149&origin=inward.
Article23. Agyeman AA, Chin KL, Landersdorfer CB, Liew D, Ofori-Asenso R. 2020; Smell and taste dysfunction in patients with COVID-19: a systematic review and meta-analysis. Mayo Clin Proc. 95:1621–31. DOI: 10.1016/j.mayocp.2020.05.030. PMID: 32753137. PMCID: PMC7275152. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85088513676&origin=inward.
Article24. Chung TW, idhar S Sr, Zhang AJ, Chan KH, Li HL, Wong FK, et al. 2020; Olfactory dysfunction in coronavirus disease 2019 patients: observational cohort study and systematic review. Open Forum Infect Dis. 7:ofaa199. DOI: 10.1093/ofid/ofaa199. PMID: 32548209. PMCID: PMC7284010. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85086922537&origin=inward.
Article25. Bolay H, Gül A, Baykan B. 2020; COVID-19 is a real headache! Headache. 60:1415–21. DOI: 10.1111/head.13856. PMID: 32412101. PMCID: PMC7272895. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85085547912&origin=inward.
Article26. Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel AS, et al. 2020; Endothelial cell infection and endotheliitis in COVID-19. Lancet. 395:1417–8. DOI: 10.1016/S0140-6736(20)30937-5. PMID: 32325026. PMCID: PMC7172722. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85083837578&origin=inward.
Article27. Pinzon RT, Wijaya VO, Buana RB, Al Jody A, Nunsio PN. 2020; Neurologic characteristics in coronavirus disease 2019 (COVID-19): a systematic review and meta-analysis. Front Neurol. 11:565. DOI: 10.3389/fneur.2020.00565. PMID: 32574250. PMCID: PMC7273516. PMID: 441680e97df041e7b5cb63fb0ccecae5. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85086782866&origin=inward.
Article28. Uygun Ö, Ertaş M, Ekizoğlu E, Bolay H, Özge A, Kocasoy Orhan E, et al. 2020; Headache characteristics in COVID-19 pandemic-a survey study. J Headache Pain. 21:121. DOI: 10.1186/s10194-020-01188-1. PMID: 33050880. PMCID: PMC7552597. PMID: a04c3ae44a5a429aa4d868b4ee76583a. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85092756063&origin=inward.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Post-COVID-19 Syndrome
- Validity and Reliability of the Turkish Version of the COVID Stress Scale
- Descriptive analysis of the incidence rate of post-acute COVID-19 syndrome in the Republic of Korea Army
- The Prevalence of Post-Traumatic Stress Disorder in the General Population during the COVID-19 Pandemic: A Systematic Review and Single-Arm Meta-Analysis
- Associations of unspecified pain, idiopathic pain and COVID-19 in South Korea: a nationwide cohort study